Corneal cross-linking (CXL) is a safe and effective treatment for keratoconus and for ectasia after refractive surgery, but determining the procedure’s success is not always simple. Generally, CXL is considered to have been effective when, at least 6 months after treatment, there is a clear reduction in maximum keratometry (K
Not all eyes, however, respond equally to CXL. Many variables, including preoperative corneal thickness, K
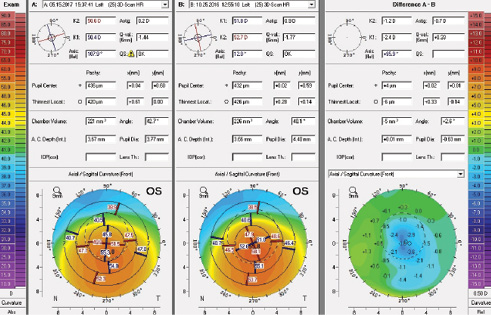
Figure 1. Tomography compare and difference maps demonstrate central flattening in a patient before and 7 months after CXL. The patient noted a subjective improvement in BCVA.
DEFINING PROGRESSION
Maximum Keratometry
Based on a review of the literature, a common variable in the definition of disease progression after CXL is an increase of more than 0.50 to 1.00 D in K
AT A GLANCE
- Not all eyes respond equally to corneal cross-linking, and the definition of posttreatment disease progression varies. Establishing progression is therefore challenging but includes evaluating maximum keratometry, corneal thickness, and the cone’s location.
- Some clear signs of progression are worsening BCVA and increased, consistent tomographic and topographic steepening of the cone. These cases warrant consideration of a cross-linking retreatment.
Stulting and colleagues reported on a large series of patients (n = 592) with keratoconus or post-LASIK ectasia who underwent epi-on CXL. None experienced an increase in K
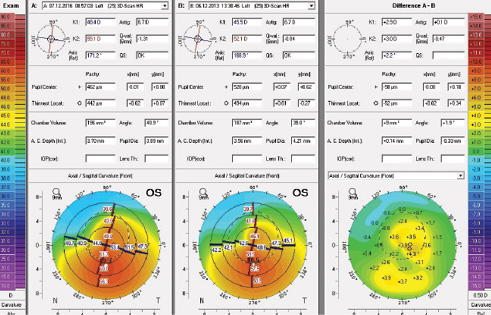
Figure 2. Tomography compare and difference maps demonstrate central steepening and likely progression in a patient with a loss of BCVA over 3 years after initial CXL.
Raiskup and colleagues reported a rate of disease progression lower than 1% (2/241 cases) 18 months after epi-off CXL.4 In contrast, Koller and colleagues reported disease progression in 7.6% of epi-off cases during the first postoperative year.2 These investigators identified a K
Corneal Thickness and the Cone’s Location
Extreme corneal thinning (< 330 µm) and more eccentrically located cones may be additional risk factors for disease progression.6 Ensuring that the cornea is at least 400 mm thick prior to the application of ultraviolet-A radiation may be necessary both to prevent endothelial damage and to improve the efficacy of treatment. Given that progression rates differ dramatically among studies, protocol variation clearly may have a significant effect on CXL outcomes. Because the epi-off protocols by Koller et al2 and by Wisse et al6 mentioned earlier found that steep and thin corneas are at increased risk of progression, other approaches, including a primary epi-on protocol, could be considered for these advanced cones. An additional benefit would be the lower risk of complications during healing.7 Rubinfeld and colleagues reported a case of progression 4 years after epi-off CXL; treatment with conductive keratoplasty and epi-on CXL stabilized the patient’s vision.8
Challenges
Establishing progression can be challenging, especially in eyes with advanced disease that require rigid gas permeable (RGP) contact lenses for functional vision. Accurately and consistently obtaining quality tomography, topography, and keratometry readings can be extremely difficult or impossible. Additionally, K
Moreover, RGP lens use can cause significant warpage on corneal topography, so requiring patients to go on a “contact lens holiday” for at least 7 to 10 days prior to testing is recommended. Because the effect of RGP lenses can last weeks to months, however, a much longer discontinuation of wear would be preferable. Contact lens holidays can present a practical problem for patients, but those who rely on RGP lenses for functional vision inevitably have more advanced disease, have eyes that are harder to image consistently, and are at higher risk for progression.
HOW TO PROCEED AFTER PROGRESSION
When the signs of progression are clear, including worsening BCVA and increased, consistent tomographic and topographic steepening of the cone, considering a CXL retreatment is warranted. A subjective worsening of vision is another important symptom. Given limited research on CXL retreatments and because progression is rare, it is important to gather reproducible data, sometimes with a series of evaluations conducted several weeks apart. It is advisable to perform a detailed surface examination looking for punctate keratopathy, scarring, or nodule formation, because these signs may affect topography and tomography readings. When the data points show consistent worsening, a retreatment is considered. When the data are not clear or reproducible or the signs are not consistent (eg, improved BCVA with increased steepening on tomography), repeat testing in 6 to 8 weeks is warranted.

Other factors in the decision on retreatment are if the patient has maintained quality vision worth preserving despite progression and whether the cornea is thick enough for CXL. If scarring is significant or if the current lens system limits vision, a deep anterior lamellar or penetrating keratoplasty could be indicated. The same considerations apply when establishing a patient’s candidacy for initial or repeat CXL treatment. There have been no case reports in the literature of more than one retreatment on any single eye. Although there is limited information on the efficacy of repeat CXL treatment, the risk of progression after a retreatment is likely to be very low. Reevaluation of the rigid contact lens system to maximize vision and fit may also be indicated.
CONCLUSION
The challenge when managing patients with suspected disease progression is establishing its presence and/or extent. Thereafter, deciding on a course of treatment—including retreatment, a contact lens refitting, or possibly keratoplasty—is fairly straightforward.
1. Soeters N, Wisse R, Godefrooij, D. A et al. Transepithelial versus epithelium-off corneal cross-linking for the treatment of progressive keratoconus: a randomized controlled trial. Am J Ophthalmol. 2015;159(5):821-828.
2. Koller T, Mrochen M, Seiler T. Complication and failure rates after corneal crosslinking. J Cataract Refract Surg. 2009;35(8):1358-1362.
3. Agrawal V. Long-term results of cornea collagen cross-linking with riboflavin for keratoconus. Indian J Ophthalmol. 2013;61(8):433-434.
4. Raiskup F, Hoyer A, Spoerl E. Permanent corneal haze after riboflavin-UVA-induced cross-linking in keratoconus. J Refract Surg. 2009;25(9):S824–S828.
5. Stulting D, Woolfson J, Trattler W, et al. Effective corneal collagen crosslinking without removal of the epithelium. Paper presented at: ASCRS/ASOA Congress & Symposium; May 5-9, 2017; Los Angeles, CA.
6. Wisse R, Godefrooij D, Soeters N, et al. A multivariate analysis and statistical model for predicting visual acuity and keratometry one year after cross-linking for keratoconus. Am J Ophthalmol. 2014;157(3):519-525.e1-2.
7. Hatch KM, Talamo JH. Trans-epithelial or “Epi on” collagen crosslinking. In: Sinjab MM, Cummings A, eds. Corneal Collagen Cross Linking. 1st ed. Cham, Switzerland: Springer International Publishing; 2017:XVI, 296.
8. Rubinfeld RS, Epstein RH, Majmudar PA, et al. Transepithelial crosslinking retreatment of progressive corneal ectasia unresponsive to classic crosslinking. J Cataract Refract Surg. 2017;43(1):131-135.