In the 1980s, surgeons performed radial keratotomy (RK) to reduce patients’ myopia. Radial incisions made in the peripheral cornea weakened and steepened this area, while causing concomitant flattening of the central cornea. Unfortunately, this controlled corneal ectasia resulted in significant side effects. First, a large proportion of RK eyes have experienced progressive hyperopia from gradual steepening of the overall cornea. Second, many patients suffer diurnal visual fluctuation as the corneal curvature varies during the day.
AT A GLANCE
- In the 1980s, surgeons performed radial keratotomy (RK) to reduce patients’ myopia. Unfortunately, a large proportion of patients experienced progressive hyperopia from gradual steepening of the overall cornea, and many suffer diurnal visual fluctuation from variability in the corneal curvature.
- The author and his colleagues sought to examine whether corneal cross-linking (CXL) could stabilize the side effects of RK. The investigators conducted a retrospective analysis of 14 post-RK eyes of seven patients who had undergone transepithelial CXL.
- Most RK patients are hyperopic, so they may be unhappy if the corneal flattening caused by CXL worsens their refraction. For the minority of undercorrected myopic RK patients, however, CXL may improve their refraction.
Corneal cross-linking (CXL) has been performed worldwide for around 20 years and was approved by the FDA in April 2016. Surgeons have performed CXL to treat keratoconus and other corneal degenerative diseases, including pellucid marginal degeneration and ectasia after refractive surgery. Fundamentally, CXL strengthens the cornea through the cross-linking of collagen fibrils within the corneal stroma. With these points in mind, investigators such as myself began to wonder if the procedure could reduce the side effects of RK.
BACKGROUND
Fuentes-Páez and colleagues reported the 6-month results of CXL on seven eyes of four RK patients.1 The average manifest spherical equivalent changed from -2.10 to +0.53 D. The mean UCVA changed from 0.3 to 0.6 (20/67 to 20/33), and the mean BCVA changed from 0.63 to 0.9 (20/32 to 20/22). The investigators concluded that RK patients treated with CXL experienced a clinical and statistically significant improvement.
OUR STUDY
Methods
Based on the corneal strengthening properties of CXL and the results reported by Fuentes-Páez et al, my colleagues and I decided to examine whether CXL could stabilize the diurnal fluctuation and/or reduce the hyperopic refractive drift in post-RK eyes. We performed a retrospective analysis of patients with a history of RK who had undergone transepithelial CXL (Figure). Our review included 14 post-RK eyes of seven patients, three male and four female. The patients ranged in age from 39 to 75 years. All of the eyes had at least 6 months of follow-up.
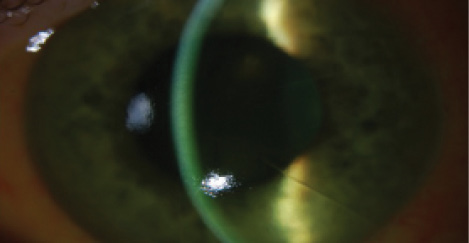
Figure. Riboflavin penetration during CXL in an RK eye.
Objective Results
The preoperative BCVA ranged from 20/20 to 20/50. Postoperatively, seven eyes had no change in BCVA, three gained 1 line, and two gained 2 lines. Two eyes, however, lost 4 lines of BCVA; both developed cataracts, which we felt to be consistent with the level of vision loss.
With all eyes considered, the average manifest refraction underwent a +0.72 D hyperopic shift. Only two eyes experienced a myopic shift, -0.53 D for one and -0.63 D for the other. Five eyes had a hyperopic shift of less than +1.00 D, and seven eyes had a hyperopic shift of more than +1.00 D.
When analyzing the corneal curvature, we found that the average keratometry reading demonstrated 0.71 D of corneal flattening. Nine eyes had a minimal change of ±0.50 D, whereas five eyes experienced more than 1.00 D of flattening.
Subjective Results
All patients were asked to share their perceptions of their vision. Two noted no subjective change. Two others felt that their vision had improved; in both cases, their preoperative refraction was myopic and shifted toward plano after CXL. Three patients stated that their vision had worsened; all of them had a hyperopic refraction preoperatively, and their level of hyperopia increased postoperatively. Because of the relatively short follow-up, we were unable to assess CXL’s overall subjective effect on diurnal visual fluctuation.
CONCLUSION
After CXL for keratoconus, eyes usually experience a gradual flattening of the cornea, evidenced by a decrease in the steepest radius of anterior corneal curvature (ie, Kmax). Similarly, transepithelial CXL produces corneal flattening in eyes with a history of RK, which tends to induce a hyperopic shift. Because most RK patients are hyperopic, the corneal flattening caused by CXL may worsen their refraction. For the minority of undercorrected myopic RK patients, however, CXL may improve their refraction.
Although CXL may stabilize a post-RK cornea and improve BCVA, patients may be unhappy with the hyperopic shift in their refractions. It is therefore imperative to determine an RK patient’s refractive state prior to considering CXL. If a patient is hyperopic and phakic, one effective strategy is to perform CXL to stabilize the cornea, wait approximately 6 months for refractive stability, and then perform a refractive lens exchange or cataract surgery to correct the increased hyperopia.
1. Fuentes-Páez G, Castanera F, Gómez de Salazar-Martinez R, et al. Corneal cross-linking in patients with radial keratotomy: short-term follow-up. Cornea. 2012;31(3):232-235.