Transepithelial corneal cross-linking (CXL), more commonly referred to as epithelium-on (epi-on) CXL, is a proposed strategy to reduce the postoperative pain and wound-related complications such as microbial keratitis and corneal scarring that have been observed after conventional CXL with the epithelium-off (epi-off) Dresden protocol.1-3
Although epi-on CXL has obvious benefits compared to epi-off CXL, previously published epi-on techniques have allowed progression of keratoconus after 1 year. Corneal stiffness measurements in animal models and shallower demarcation lines in the human eye with epi-on CXL suggest less effectiveness with these protocols.
AT A GLANCE
- A novel technique for epithelium-on corneal cross-linking (epi-on CXL) and a new riboflavin solution could solve the problem of poor riboflavin penetration into the corneal stroma that is ubiquitous among other current epi-on techniques.
- Findings of a recent study indicated that epi-on CXL using the protocol developed by CXL Ophthalmics halted the progression of ectatic disease for 24 months after treatment, improved corrected distance visual acuity to a similar extent as epithelium-off CXL, and avoided the complications of epithelial removal.
In attempts to increase penetration during epi-on CXL, investigators have proposed several different enhanced riboflavin solutions—0.01% and 0.02% benzalkonium chloride, 0.44% NaCl, tris(hydroxymethyl)aminomethane (TRIS), ethylenediaminetetraacetic acid (EDTA), hydroxypropyl methylcellulose (HPMC), and hypotonic saline. None, however, has effectively halted the progression of keratoconus, and all, in fact, could induce significant epithelial damage.4
Now, with a novel technique and a new riboflavin solution developed by CXL Ophthalmics, the problem of poor penetration into the corneal stroma during epi-on CXL may be solved, R. Doyle Stulting, MD, PhD, said at the 2017 ASCRS/ASOA Annual Symposium & Congress.5 According to Dr. Stulting, the CXLUSA epi-on CXL protocol includes
- A patented riboflavin formulation with optimized osmolarity, pH, and concentration as well as an enhancer that allows riboflavin to penetrate an intact epithelium
- Special wands and sponges to enhance penetration
- No riboflavin application during ultraviolet A (UV-A) exposure to avoid blocking UV-A light from entering the stroma
- A 12-mm–diameter light
- Unique pulsed UV-A light irradiation that allows oxygen to diffuse into the stroma during the off phase of CXL
- Increased UV-A light fluence of 4 mW/cm2
STUDY RESULTS
Dr. Stulting reported 12- and 24-month follow-up of 592 eyes with keratoconus or ectasia after LASIK that were treated with epi-on CXL.5 He concluded that this approach achieved corneal strengthening that was structurally and functionally similar to that produced by conventional epi-off CXL (unpublished data, 2017). Although the mean reduction in maximum keratometry (Kmax) was not as pronounced as is seen with epi-off CXL, eyes treated with the CXLUSA epi-on protocol in the study also achieved an improvement in uncorrected acuity, an improvement in corrected acuity, a reduction in higher-order aberrations, and a reduction in coma during the follow-up period.
All enrolled eyes had either keratoconus or ectasia. By 12 months postoperatively, mean BCVA improved by about 1 line, and this improvement was not lost between 12 and 24 months, as had been reported in previous studies with other epi-on protocols. About 10% of eyes gained 1.00 D or more of Kmax, but three times more eyes had a reduction of 1.00 D or more of Kmax. The mean BCVA of eyes that experienced an increase of 1.00 D or more of Kmax actually improved, and no eyes with an increase in Kmax of 1.00 D or more lost more than 1 line of BCVA. These results indicate that the treatment truly halted the progression of disease and that the observed improvement in outcome measures was not due to random variation, Dr. Stulting said.
Of note, the study included 49 eyes of patients who were 18 years of age or younger. According to previous publications, 88% (43) of these eyes should have experienced disease progression during 1 year of observation. Interestingly, Dr. Stulting related that some of the most impressive improvements in visual acuity in the study were in this population of pediatric patients (Figure).
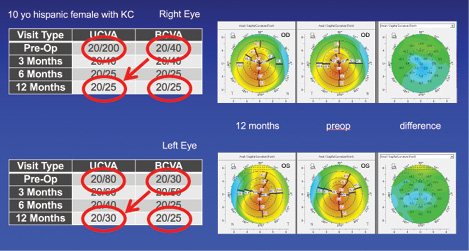
Figure. Topographical maps of a 10-year-old patient with keratoconus.
CONCLUSION
The findings of this study indicate that epi-on CXL using the CXLUSA protocol halted the progression of ectatic disease, improving Kmax, visual acuity, higher-order aberrations, and coma and avoiding the complications of epithelial removal—an effect that is not lost between 12 and 24 months after treatment. The question now is this: Will the CXLUSA protocol become more widely accepted as the standard of care for the treatment of ectatic corneal disease?
1. Spoerl E, Huhle M, Seiler T. Induction of cross-links in corneal tissue. Exp Eye Res. 1998;66:97-103.
2. Wollensak G, Spoerl E, Seiler T. Riboflavin/ultraviolet-A-induced collagen crosslinking for the treatment of keratoconus. Am J Ophthalmol. 2003;135:620-627.
3. Leccisotti A, Islam T. Transepithelial corneal collagen cross-linking in keratoconus. J Refract Surg. 2010;26:942-948.
4. Caporossi A, Mazzotta C, Baiocchi S, Caporossi T, Paradiso AL. Transepithelial corneal collagen crosslinking for keratoconus: qualitative investigation by in vivo HRT II confocal analysis. Eur J Ophthalmol. 2012;22(suppl 7):S81-88.
5. Stulting RD. Effective corneal collagen crosslinking without removal of the epithelium. Paper presented at the: 2017 ASCRS/ASOA Annual Symposium & Congress; May 5-9, 2017; Los Angeles, CA.