
With the baby boomer population aging and tech-wielding millennials coming into their own, the pool of potential refractive surgery patients has been growing in recent years. At the same time, however, a gap is developing in the number of eye surgeons available to cater to these prospective patients’ needs. There has been minimal change in the number of ophthalmology residents graduating in the past 10 years: from 447 resident positions in 2006 to 469 positions in 2016.1 Meanwhile, retirement rates continue to rise.
With procedural volume increasing for both refractive and cataract surgery, spending face-to-face chair time with patients is becoming more difficult for surgeons. An answer exists, and many optometrists and ophthalmologists have already been practicing this way for years: collaborative care.
The number of ophthalmologists and optometrists engaging in shared care continues to increase. A 2017 poll of the group “ODs on Facebook” asked whether group members currently practice collaborative care for refractive surgery patients. Of 103 optometrists who responded, 97 stated that they currently practice shared care for these patients. Granted, this is an unscientific poll and a small sampling, but it is notable that 94% of respondents said they do practice shared care with ophthalmologists (Figure 1).
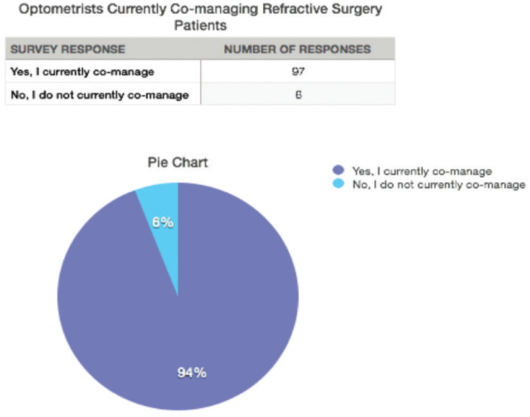
Figure 1. A 2017 poll of the group “ODs on Facebook.”
One of the largest and most well-known examples of refractive surgery collaborative care, TLC Laser Eye Centers, has used the concept of team-based shared care of patients for more than 20 years. In its care model, optometrists working directly for the company perform evaluations and perioperative care at the company’s centers, and affiliated optometrists in the community also use a team-based approach to patients’ surgical care.2 The use of all available assets allows increased surgical volume, more individualized patient care, and increased revenue for all. Although this example is of a large company, the same economies can also be achieved on a smaller scale with collaboration among local practices of optometrists and ophthalmologists.
WHO BENEFITS?
Using an optometrist either within a practice or within the community to help collaboratively care for surgical patients is beneficial for all parties involved. Optometrists get the opportunity to be more involved in their patients’ care before, during, and after their surgical journeys. Shared care is also a revenue builder for the optometric practice, both in fees from the patient management itself and in potential referrals from the ophthalmologist in the future. For surgeons, working closely with optometrists can help to decrease their chair time with patients and increase their referrals.
Not only is this arrangement beneficial for the doctors involved, but it is to patients’ advantage as well. A more streamlined team approach decreases the time, number of appointments, and in some cases, the amount of travel required of patients. They often have spent years seeing their optometrist, and having a familiar face involved can increase their confidence when making the decision to have surgery.
In our practice, Virginia Eye Consultants, there are four full-time optometrists who work with more than 100 optometrists in our area caring for our refractive surgery patients.
WHAT DOES SHARED CARE INVOLVE?
Preoperatively, optometrists who perform collaborative care should discuss the surgical options with patients and be involved in the process as much as possible. Optometrists should also aggressively treat any dry eye or ocular surface disease before sending patients to the surgeon for refractive surgery evaluation. This helps to maximize potential outcomes and minimize the surgeon’s overall chair time and need for repeated measurements.3 A retrospective study by Albietz et al looked at ocular surface management of both PRK and LASIK patients. The study found that patients who underwent ocular surface management before and after surgery had significantly fewer postoperative dry eye symptoms and less myopic outcomes.3
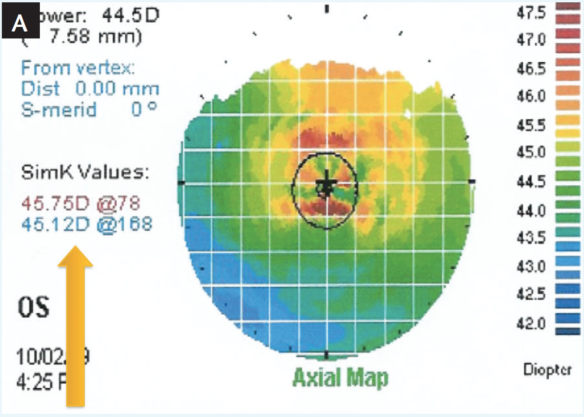
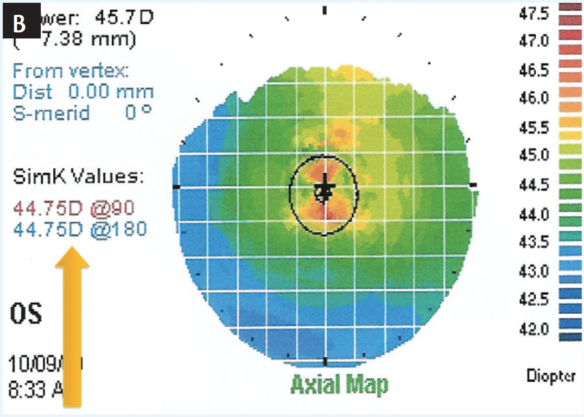
Figure 2. Initial topographic evaluation of a 60-year-old patient before ocular surface management (A). Same patient 1 week later, after dry eye was identified and treated with topical steroids and cyclosporine (B).
Figure 2 shows an example of dry eye management in a 60-year-old man. The patient’s topography before dry eye treatment shows irregular hot spots in the center of the cornea and keratometry values that are 1.00 D steeper than the topography 1 week later, after treatment was initiated. Imagine if this patient’s surgical plan had been made from the original measurements.
Postoperative collaborative care can take many forms; there is not a one-size-fits-all structure. Many practices include both ophthalmologists and optometrists, with the optometrists seeing primary care and postoperative patients. Another option is shared care with a community optometrist who is not directly associated with the ophthalmologist’s practice. In both cases, discussion between the surgeon and the optometrist about what is to be expected and the surgeon’s protocols and preferences for postoperative medications and directions is all-important. Some surgeons prefer to see patients in-house themselves the day after surgery and then for the optometrist to see patients at subsequent visits. Some surgeons may want to see patients 6 months later.
These logistics must be discussed in order to make the collaborative relationship work. They can always be revisited to ensure that each part of the team feels comfortable.
Long-term vision care of patients who have had LASIK, PRK, or other refractive surgeries should be managed by the optometrist. Even though patients may not need glasses or contacts after refractive surgery, their ocular health management and ocular surface disease still must be monitored. Returning patients to their optometrists gives surgeons more time to do what they do best: surgery!
HOW TO MAKE IT WORK FOR YOU
Developing a relationship and a good rapport with fellow eye care physicians is key to forming an effective shared care team. Reaching out to area providers to see who is receptive to this type of patient care is one way to broach the subject. Our practice, an optometrist-ophthalmologist referral-based practice, hosts training lectures for doctors in the area who might be interested in shared care of their patients. This allows the optometrists and surgeons to meet and opens the door for discussion regarding patients’ care.
Maintaining an open line of communication between the doctors is important so that patients’ care can be freely discussed and both parties can feel comfortable. Medical notes sent after each visit, along with a quick email message or phone call discussing any concerns, can quickly update all parties on the patient’s healing process and care issues.
MUTUAL RESPECT
Respect and trust are needed on both sides of the team; this is the only way to make a collaborative relationship work. Each party has a role to play, and both parties are well equipped to take care of their aspects of their patients’ needs. Part of this respect is making sure that patients are returned to their primary ocular care physician at the end of the postoperative care period. This helps to build trust that patients who are referred for surgery will be returned to their optometrist and, in turn, likely increases referral volume for refractive surgery.
Collaborative or shared care is a great practice-building option for everyone involved and an efficient way to deliver care to patients. Those not already practicing this model may wish to consider branching out and adding refractive surgery collaborative care to their ever-growing medical repertoire.
1. SF Match. Residency matching service. Ophthalmology. https://www.sfmatch.org/SpecialtyInsideAll.aspx?id=6&typ=2&name=Ophthalmology# . Accessed February 9, 2017.
2. TLC LASIK Center Affiliated Doctors. TLC Laser Eye Centers website. http://www.tlcvision.com/the-tlc-eye-center-difference/partnering-with-your-eye-doctor/. Accessed February 9, 2017.
3. Albietz JM, McLennan SG, Lenton LM. Ocular surface management of photorefractive keratectomy and laser in situ keratomileusis. J Refract Surg. 2003;19(6):636-644.




