Epi-on Techniques are Still Considered Less Efficacious
By Cosimo Mazzotta, MD, PhD

The technique most widely studied for the prevention of progression of keratoconus and secondary ectasia is conventional epithelium-off corneal cross-linking (epi-off CXL) , with a standardized fluence of 5.4 J/cm2 ultraviolet A (UV-A) light delivered in the corneal tissue.
Transepithelial, or epithelium-on (epi-on), CXL techniques have been described with the aims of reducing postoperative pain, wound-related complications, and infectious risk and offering the promise of treatment delivery outside of the OR. In order to understand why these epi-on techniques are still considered less efficacious, we must understand three basic concepts:
AT A GLANCE
- To date, the efficacy of epithelium-on corneal cross-linking (epi-on CXL) has been limited. Further investigation into its ability to halt the progression of keratoconus while reducing patients’ postoperative pain, risk of infection, and wound-related complications is required.
- Iontophoresis CXL was recently introduced in an attempt to overcome the major limitations of the original epi-on treatments—inhomogeneous and insufficient intrastromal riboflavin penetration and concentration and the natural shield against ultraviolet A light penetration provided by the corneal epithelium.
- Future epi-on accelerated CXL procedures with oxygen or ozone supplementation could be a key to success.
Concept No. 1. The riboflavin-epithelium relationship. The removal of the corneal epithelium is necessary in CXL, because riboflavin is a large, hydrophilic molecule that cannot penetrate an intact epithelium. Additionally, the epithelium and the Bowman lamina, depending on the waveband, block about 30% of the UV-A light energy used in the CXL procedure.1
Concept No. 2. The origin of corneal ectasia. The ectatic process that causes keratoconus comes from the posterior surface of the cornea—the weakest portion of the stroma—driving toward consequent deformation of the anterior surface and corneal thinning.
Concept No. 3. The volume of CXL. Only epi-off CXL has demonstrated sufficient treatment penetration to at least 250 to 300 µm of stromal depth, overcoming the stiff anterior cornea and conferring sufficient stiffening of total stromal volume.2,3 By sufficient, I mean that the cross-linked stromal volume necessary to induce long-term stabilization of ectasia, maximizing the efficacy of CXL therapy, must penetrate beyond the anterior 200 µm of the corneal stroma. This is particularly true in patients 18 years of age and younger, who generally experience more aggressive keratoconus progression. This therapeutic performance is still beyond the capability of the epi-on CXL techniques that have been proposed, even with enhanced riboflavin solutions, leading to a surface CXL treatment. The volume-based CXL treatments are more effective in bringing about the stabilization of ectasia.
COMPARING TECHNIQUES
Ex vivo biomechanical studies with Brillouin microscopy, by assigning a corneal stiffening index as a quantitative measure of the biomechanical efficacy of CXL, have allowed a direct comparison of epi-on techniques to the epi-off Dresden protocol.4 These investigations have documented that the biomechanical rigidity induced with epi-on CXL is approximately 70% less than that with conventional epi-off CXL.
Moreover, comparison of in vivo corneal OCT scans has clearly shown the absence of a demarcation line with inhomogeneous slightly increased reflectivity of the sub-Bowman stroma after epi-on CXL (Figure 1), generally less than 100 µm of stromal depth.5 In vivo confocal microscopy investigations after conventional and epi-on CXL have also shown keratocyte apoptosis unevenly distributed in the anterior 80 to 100 µm of the corneal stroma in epi-on CXL (Figure 2A),5 compared with 250 to 300 µm with the conventional epi-off technique (Figure 2B).
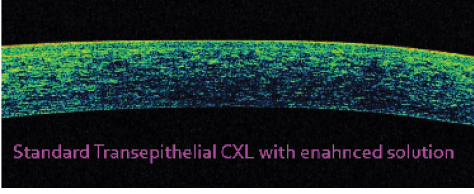
Figure 1. Spectral-domain optical coherence tomography (OCT) scan of the cornea taken 1 month after epi-on CXL with enhanced solution. Note the absence of a demarcation line with slightly increased reflectivity unevenly distributed in the sub-Bowman stroma.
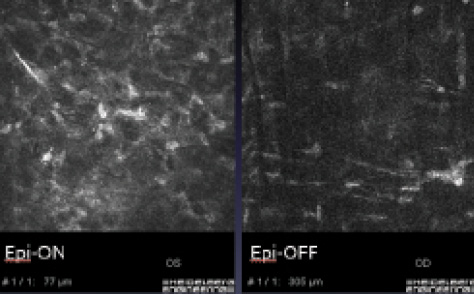
Figure 2. In vivo confocal microscopy after CXL. Superficial and inhomogeneous keratocyte apoptosis is seen 1 month after epi-on CXL (Left). Deep homogeneous keratocyte apoptosis to a depth of 300 µm is seen after conventional epi-off CXL 1 month after treatment (Right).
It is clear that epi-on treatments, acting on the anterior stromal surface, may have a temporary refractive impact, but they lack sufficient stromal penetration. The limited penetration and the insufficient biomechanical power of epi-on CXL—one-third the power of epi-off treatments—do not guarantee the long-term ectasia stabilization that is the goal of CXL treatment.
There is general consensus that epi-on CXL is a safe procedure with no complications associated with the healing process. A number of enhanced riboflavin solutions have been proposed for use in epi-on CXL, including 0.01% and 0.02% benzalkonium chloride, 0.44% NaCl, tris(hydroxymethyl)aminomethane (TRIS), ethylenediaminetetraacetic acid (EDTA), hydroxypropyl methylcellulose (HPMC), and hypotonic and isotonic saline. Use of these solutions did not effectively halt progression of keratoconus, but it did induce significant epithelial damage, with marked punctate epitheliopathy in the early postoperative period.6
According to data in the literature, keratoconus progression, defined as an increase in maximum keratometry greater than 1.00 D, occurred in approximately 50% of eyes by 12 months after epi-on CXL.7 In our experience, 36% of patients between 19 and 26 years of age and more than 50% of pediatric patients 18 years old and younger, when treated with epi-on CXL, required an epi-off retreatment after 15 to 24 months of follow-up.8
Epi-on CXL could offer a noninvasive therapeutic approach for young keratoconic patients, but it is still not as efficacious as epi-off CXL.
Iontophoresis CXL
Recently, iontophoresis CXL (I-CXL) was introduced in an attempt to overcome the major limitations of the original epi-on treatments—inhomogeneous and insufficient intrastromal riboflavin penetration and concentration and the natural shield against UV-A light penetration provided by the corneal epithelium (about 30% to 60% depending on UV-A light waveband). According to data in the literature, iontophoresis-assisted transepithelial imbibition with Ricrolin+ (Sooft; not available in the United States) yielded greater and deeper riboflavin saturation compared with epi-on CXL with enhanced solutions.9 This approach also maintained the advantages of avoiding epithelial removal and shortened procedural time, but it did not reach the riboflavin concentrations obtained with standard epi-off riboflavin diffusion.
I-CXL has the potential to become a possible alternative for halting the progression of keratoconus and for reducing patients’ postoperative pain, reducing the risks of infection and wound-related complications, and maintaining a short treatment time. The 1-year outcomes of I-CXL were almost comparable with those of conventional epi-off CXL regarding stabilizing the progression of keratoconus10; however, the 2-year follow-up showed less efficacy in halting keratoconus progression than conventional CXL.11 Therefore, the relative efficacy of this technique compared with standard epi-off techniques remains to be determined. There are two limitations of this method that require adjustments and further investigation: (1) the halved riboflavin intrastromal concentration compared with conventional CXL and (2) the uneven demarcation line that is superficially visible in only 35% of eyes compared with 95% of eyes after conventional CXL.
At the Siena Crosslinking Center, we recently started a new interventional protocol with a customized iontophoresis epi-on treatment. The treatment fluence is calibrated in relation to the UV-A light photoattenuation provided by the corneal epithelium and the Bowman lamina. During the treatment, pulsed UV-A light is applied, and the total treatment time is 17 to 20 minutes on average (Figure 3).
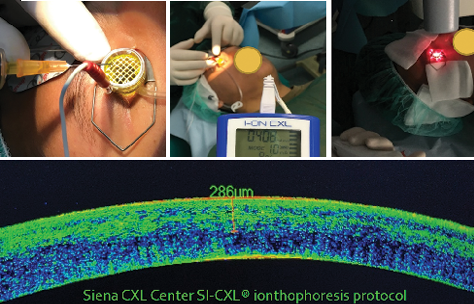
Figure 3. Iontophoresis-assisted transepithelial A-CXL with increased fluence at Siena Crosslinking Center. The corneal suction ring is placed, and the riboflavin solution is administered (Top left); electrically assisted transepithelial riboflavin transfer is administered for 5 minutes (Top center); and pulsed light UV-A A-CXL with increased fluence is applied (Top right). Spectral-domain OCT scan of the cornea after therapeutic contact lens removal shows a clear demarcation line at 290-µm depth (Bottom).
A second epi-on CXL protocol, accelerated CXL (A-CXL), is based on the supplemental use of oxygen with new riboflavin formulations, and a third research line will be started soon with the intraoperative use of ozone. We know that oxygen is the driver of CXL reaction and that the biomechanical effect of CXL seems to be oxygen dependent. Higher oxygen availability could possibly increase the overall efficacy of riboflavin UV-A CXL,12 and a great potential could be offered by the intraoperative use of supplemental oxygen and/or ozone delivered intraoperatively during accelerated transepithelial CXL procedures.
CONCLUSION
To date, the efficacy of epi-on CXL has been limited. It requires further investigation in order to fulfill its potential to become a valid option in select cases for halting the progression of keratoconus while also reducing patients’ postoperative pain, risk of infection, and wound-related complications.
Future research in CXL must include investigations of epi-off and epi-on A-CXL procedures, customized according to the specifics of each case, including the individual patient’s keratoconus parameters, the patient’s needs, and the likelihood of compliance.
A-CXL procedures, as they emerge, will be calibrated to a specific efficacy range window, with a duration of 20 minutes on average and a programmed treatment dose, UV-A power level, and penetration depth. In the near future, I believe the combination of sufficient stromal riboflavin uptake, adequate exposure time, increased stromal oxygenation, and calibrated UV-A fluence could lead to better efficacy of epi-on A-CXL procedures. Increasing reactive oxygen availability may increase the amount of cross-linking and the efficacy of epi-on CXL procedures in the future.
Epi-off procedures are recommended for pediatric patients and with CXL plus phototherapeutic keratectomy or PRK techniques. Future research on increased fluence compensating for the UV-A light photoattenuation provided by the epithelium, calibrated UV-A power and exposure time, and oxygen or special intraoperative ozone supplementation could increase the efficacy of transepithelial procedures with the relative advantages.
1. Podskochy A. Protective role of corneal epithelium against ultraviolet radiation damage. Acta Ophthalmol Scand. 2004;82:714-717.
2. Kohlhaas M, Spoerl E, Schilde T, et al. Biomechanical evidence of the distribution of cross-links in corneas treated with riboflavin and ultraviolet A light. J Cataract Refract Surg. 2006;32(2):279-283.
3. Schumacher S, Mrochen M, Wernli J, et al. Optimization model for UV-riboflavin corneal cross-linking. Invest Ophthalmol Vis Sci. 2012;53(2):762-769.
4. Scarcelli G, Kling S, Quijano E, et al. Brillouin microscopy of collagen crosslinking: noncontact depth-dependent analysis of corneal elastic modulus. Invest Ophthalmol Vis Sci. 2013;54:1418-1425.
5. Mazzotta C, Hafezi F, Kymionis G, et al. In vivo confocal microscopy after corneal collagen crosslinking. Ocul Surf. 2015;13(4):298-314.
6. Caporossi A, Mazzotta C, Baiocchi S, et al. Transepithelial corneal collagen crosslinking for keratoconus: qualitative investigation by in vivo HRT II confocal analysis. Eur J Ophthalmol. 2012;22 suppl 7:S81-88.
7. Gatzioufas Z, Raiskup F, O’Brart D, et al. Transepithelial corneal cross-linking using an enhanced riboflavin solution. J Refract Surg. 2016;32(6):372-377.
8. Caporossi A, Mazzotta C, Paradiso AL, et al. Transepithelial corneal collagen crosslinking for progressive keratoconus: 24-month clinical results. J Cataract Refract Surg. 2013;39(8):1157-1163.
9. Franch A, Birattari F, Dal Mas G, et al. Evaluation of intrastromal riboflavin concentration in human corneas after three corneal cross-linking imbibition procedures: a pilot study. J Ophthalmol. 2015;2015:794256.
10. Vinciguerra P, Randleman JB, Romano V, et al. Transepithelial iontophoresis corneal collagen cross-linking for progressive keratoconus: initial clinical outcomes. J Refract Surg. 2014;30(11):746-753.
11. Jouve L, Borderie V, Sandali O, et al. Conventional and iontophoresis corneal cross-linking for keratoconus: efficacy and assessment by optical coherence tomography and confocal microscopy. Cornea. 2017;36(2):153-162.
12. Richoz O, Hammer A, Tabibian D, et al. The biomechanical effect of corneal collagen cross-linking (CXL) with riboflavin and UV-A is oxygen dependent. Transl Vis Sci Technol. 2013;2(7):6.
Epi-on CXL: Effective When Done Right
By Roy S. Rubinfeld, MD, MA

The discussion of whether corneal cross-linking (CXL) works best with the epithelium on (epi-on) or off (epi-off) is often framed as a debate between the two approaches: Which is better, epi-on or epi-off? In my opinion, that is the wrong question. The real question is: What is the safest, most effective technology to perform corneal strengthening?
Think about the choice for our patients. Epi-off CXL means having their corneal epithelium surgically removed, waiting in pain for a week for re-epithelialization, then waiting another month or more until they recover their preoperative vision. Who would choose this option if there were an equally effective, noninvasive epi-on procedure that would reduce the risk, reduce the pain, reduce the recovery time, and allow patients to return to work the next morning?
AT A GLANCE
- The most recent iteration of a novel epithelim-on corneal cross-linking method, developed by CXLUSA and performed in a cohort of 88 eyes followed for 2 years or more, produced improvements in visual acuity, maximum keratometry, and higher-order aberration measurements.
- The CXLUSA group has performed this version of epithelim-on corneal cross-linking over many years in thousands of eyes under ongoing investigational review board-approved clinical protocols; a manuscript is in preparation.
Epi-on is, therefore, the more attractive procedure to patients, and an effective and safe epi-on technique is highly desirable for those who need corneal strengthening. Unfortunately, numerous commercial and investigational epi-on techniques have been tried by a wide range of investigators worldwide, with disappointing results—until recently. Now, a proprietary, patented approach to epi-on CXL, currently under investigation in an ongoing multicenter study in the United States, is showing great promise. This article explains some of the historical perspective on epi-on CXL and explores prospects for the future.
HISTORICAL PERSPECTIVE
We all know the story of the breakthrough in Dresden, Germany, in 1998, with the realization by Seiler and colleagues that corneas could be strengthened using ultraviolet A (UV-A) and riboflavin, followed several years later by successful clinical application of the technique to halt the progression of ectasia in patients with keratoconus.1,2 Like many other surgical procedures, the CXL technique has since undergone refinements to try to make it safer and less invasive.
Problems that have been reported after epi-off CXL include corneal edema, corneal haze, infections, sterile infiltrates or delayed epithelial healing, pain, photophobia, slow visual recovery, and perforations.3-6 Haze has, in some cases, been permanent.6 Infectious agents have included Escherichia coli, Staphylococcus epidermidis, streptococcal species, and Acanthamoeba.
The root cause of most of these complications, it should be noted, is the removal of the protective layer of the corneal epithelium. It stands to reason, then, that an effective, noninvasive CXL procedure that eliminates epithelial removal would be a major benefit. In addition to avoiding the complications noted earlier, an effective epi-on technique would eliminate the long recovery time for patients; allow treatment of thinner, steeper, younger corneas; and allow patients to return to work and visual functionality on postoperative day 1, return to contact lens wear within days, and reduce the duration of their discomfort to a single day.
If the availability of an effective epi-on CXL procedure led to earlier and broader adoption of this therapeutic approach, it could also potentially reduce the need for corneal transplantation in keratoconus. In Europe, where epi-off CXL has been performed more extensively than in the United States, an effect on corneal transplantation volume has already been seen. A Dutch group reported this past year that the number of corneal transplants in the Netherlands was reduced by 25% in the 3 years after the introduction of CXL, compared with the 3 years before its introduction.7
Restoration of Lost Vision With CK Plus Epi-on CXL
By Roy S. Rubinfeld, MD, MA
Based on an observation by Arthur B. Cummings, MB ChB, FCS(SA), MMed(Ophth), FRCS(Edin), we have been able to restore lost vision in some keratoconus patients with the off-label use of conductive keratoplasty (CK) in combination with epithelium-on corneal cross-linking (CXL). We perform the thermokeratoplasty corneal flattening procedure at one visit and then the corneal strengthening procedure the following day. It appears that the CXL locks in the improved vision effect provided by the CK, and we have seen this effect persist in patients who have been observed for several years now (Figure). We look forward to further exploring the synergy of these two noninvasive, nonsubtractive procedures in larger cohorts with longer follow-up.
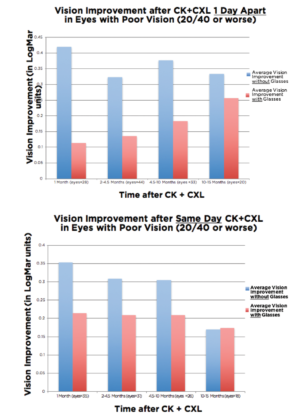
Figure. Vision improvement occurs when CXL is performed 1 day after CK (top). The effect is greater when the procedures are separated by 1 day than when performed together (bottom).
One might ask, given all the potential benefits of an epi-on approach: Why was the epithelium removed in the first place in the early work on CXL in Dresden? The reason was that the commercial formulation of riboflavin could not penetrate the epithelium. That formulation contained the large polysaccharide dextran and had other properties that interfered with penetration through the corneal epithelium. Therefore, because the researchers could not load the stroma sufficiently with riboflavin, they surgically removed the epithelium. Until now, no subsequent formulations of riboflavin, even including other molecules such as benzalkonium chloride, tris(hydroxymethyl)aminomethane (TRIS), and ethylenediaminetetraacetic acid (EDTA), have been shown to be effective for transepithelial CXL in long-term follow-up studies.
There was initial excitement when Caporossi and colleagues discussed early results of an epi-on technique at professional meetings. Although their results at 3 to 6 months showed relative improvements, distance BCVA and distance UCVA gradually returned to baseline, and their published results with 2 years of follow-up were disappointing.8 No subsequent publications reporting long-term results of epi-on techniques, whether with alternative formulations of riboflavin or with iontophoresis, have shown efficacy matching that of epi-off CXL.9,10 We, too, in our clinical trials, investigated the use of iontophoresis and were disappointed with the poor stromal loading, postoperative epithelial sloughing, and consistent reports of marked patient discomfort.
THE PROBLEM WITH PREVIOUS EPI-ON TECHNIQUES
Successful CXL requires three components:
No. 1. Adequate, homogeneous stromal loading of riboflavin
No. 2. Adequate, unblocked transmission of UV-A light energy through the epithelium to the stroma
No. 3. Adequate oxygen, the rate-limiting reagent for the photochemical reaction that causes cross-linking when both Nos. 1 and 2 are present
If there is an inadequate amount of any of the three components, inadequate CXL is the result. Three basic principles are necessary for success:
No. 1. The riboflavin has to get through intact epithelium without disrupting it or causing it to slough off.
No. 2. The riboflavin must be homogeneously loaded into the stroma, where the cross-linking occurs, but it must not build up in the epithelium, because it would block UV-A transmission.
No. 3. The oxygen in the stroma must be maximized, because it is generally the rate-limiting reagent in the cross-linking reaction.
The problem with previous epi-on techniques is that they failed to get these three components, in the right mixture, into the stroma.
ANOTHER APPROACH
The CXLUSA study group, a multicenter group of eye surgeons in the United States, has been working since 2009 to improve the treatment of patients with keratoconus. As a member of the group, our center’s efforts include trying to overcome the limitations of earlier epi-on CXL techniques. With the guidance of the highly experienced photochemical expert Raymond Hartman, we have explored a series of iterative changes in riboflavin formulations, UV-A exposure patterns, delivery systems, and other treatment parameters.
Over the course of several years, we optimized the pH concentration and osmolarity of the formulation; identified a novel, patented additive that was nontoxic to the epithelium; and adopted a unique patent-pending UV-A pulsing cycle technology to allow the rate-limiting oxygen to replenish in the stroma and facilitate the cross-linking reaction using half the UV-A exposure of the standard Dresden epi-off method. We now have animal and clinical data showing that our most recent, optimized iterations work extremely well in our novel method of epi-on CXL.11,12 Ex vivo work in rabbit tissue, analyzed by an independent laboratory, has demonstrated rapid, homogeneous, consistent stromal loading in 10 minutes with our proprietary, patented riboflavin formulation, as reported in 2015 at the International CXL Congress.11 Subsequently, R. Doyle Stulting, MD, PhD, presented these animal as well as human clinical data in his 2016 Binkhorst Lecture.12
At the recent International CXL Congress in Zurich, Switzerland, Dr. Stulting then reported on 608 eyes, of which only two (0.3%) needed repeat treatment.13 A cohort of 88 eyes followed for 2 years or more showed improvements in visual acuity, maximum keratometry, and higher-order aberration measurements. Notably, these data included follow-up for all patients at 2 years, the interval at which Caporossi et al8 had observed regression with their epi-on technique. Dr. Stulting’s data, in which not a single eye treated with the CXLUSA protocol demonstrated progression at 2 years or longer postoperatively, are currently being prepared for publication.
Bilateral simultaneous delivery
By now, the CXLUSA group has performed this specific version of epi-on CXL in thousands of eyes under ongoing investigational review board-approved clinical protocols. Because visual recovery is immediate, the procedures can be done with bilateral simultaneous delivery of UV-A energy.
Several aspects of the CXLUSA epi-on protocol are proprietary and patented or patent-pending, and a company called CXL Ophthalmics (CXLO) has been formed to pursue commercialization of the technologies within and outside the United States.
Because I have been able to spend some time in Europe, I know there is a great deal of skepticism there about the prospects for epi-on CXL. I must emphasize that CXLO is not advocating that all epi-on CXL works. In fact, none of the commercial transepithelial CXL products works. Only one proprietary transepithelial formulation and system has been demonstrated to effectively load the stroma and achieve good long-term results. As European ophthalmologists learn more about the data and the results we are achieving with the CXLUSA protocol, there has been increasing interest from well-respected clinicians in Europe in exploring this technology.
LOOKING FORWARD
If a safe and effective epi-on CXL technique becomes widely available, why would anyone still use an epi-off technique? Epi-off would be appropriate in select cases, for example, if a patient required combined topography-guided PRK plus CXL. If the epithelium is to be removed for the PRK, then epi-off CXL makes sense. Otherwise, for the reasons outlined herein, given equivalent results, it seems likely that patient preference will favor the less invasive procedure. This has certainly been our experience since 2012.
1. Spoerl E, Huhle M, Seiler T. Induction of cross-links in corneal tissue. Exp Eye Res. 1998;66:97-103.
2. Wollensak G, Spoerl E, Seiler T. Riboflavin/ultraviolet-A-induced collagen crosslinking for the treatment of keratoconus. Am J Ophthalmol. 2003;135:620-627.
3. Koller T, Mrochen M, Seiler T. Complication and failure rates after corneal crosslinking. J Cataract Refract Surg. 2009;35(8):1358-1362.
4. Pérez-Santonja JJ, Artola A, Javaloy J, et al. Microbial keratitis after corneal collagen crosslinking. J Cataract Refract Surg. 2009;35(6):1138-1140.
5. Sharma N, Maharana P, Singh G, Titiyal JS. Pseudomonas keratitis after collagen crosslinking for keratoconus: case report and review of literature. J Cataract Refract Surg. 2010;36(3):517-520.
6. Raiskup F, Hoyer A, Spoerl E. Permanent corneal haze after riboflavin-UVA-induced cross-linking in keratoconus. J Refract Surg. 2009;25(9):S824-828.
7. Godefrooij DA, Gans R, Imhof SM, Wisse RP. Nationwide reduction in the number of corneal transplantations for keratoconus following the implementation of cross-linking. Acta Ophthalmol. 2016;94(7):675-678.
8. Caporossi A, Mazzotta C, Paradiso AL, et al. Transepithelial corneal collagen crosslinking for progressive keratoconus: 24-month clinical results. J Cataract Refract Surg. 2013;39(8):1157-1163.
9. Gatzioufas Z, Raiskup F, O’Brart D, et al. Transepithelial corneal cross-linking using an enhanced riboflavin solution. J Cataract Refract Surg. 2016;32:372-377.
10. Jouve L, Borderie V, Sandali O, et al. Conventional and iontophoresis corneal cross-linking for keratoconus: efficacy and assessment by optical coherence tomography and confocal microscopy. Cornea. 2017;36(2):153-162.
11. Rubinfeld RS, Talamo J, Stulting RD. Quantitative analysis of trans-epithelial corneal riboflavin loading. Paper presented at: International CXL Congress; December 4-5, 2015; Boston, MA.
12. Stulting RD. Predicting and treating corneal ectasia. Paper presented at: ASCRS/ASOA Congress & Symposium; May 6-10, 2016; New Orleans, LA.
13. Stulting RD, Woolfson J, Trattler W, Rubinfeld RS. Corneal crosslinking without epithelial removal. Paper presented at: International CXL Congress; December 2-3, 2016; Zurich, Switzerland.