CASE PRESENTATION
A 51-year-old man presents for a cataract evaluation. The patient was diagnosed with human immunodeficiency virus (HIV) infection in April 2016 and has a history of profound vision loss in both eyes dating back to June 2016. The ocular history in both eyes is significant for progressive outer retinal necrosis (PORN), with varicella-zoster virus (VZV) detected by polymerase chain reaction of intraocular fluid. The patient’s history includes multiple gancyclovir intravitreal injections, retinal detachment (RD) repair with vitrectomy, endolaser treatment, retinectomy, and silicone oil in both eyes. In addition to taking oral valganciclovir 450 mg daily, a fixed combination of trimethoprim and sulfamethoxazole (Bactrim, Roche), and azithromycin, he is on oral highly active antiretroviral therapy for infectious disease. The patient’s current ocular medications include prednisolone acetate 1% four times daily and atropine 1% once daily in each eye.
Previous examinations found subretinal fluid in the inferior macula of the patient’s left eye. In October 2016, OCT imaging showed a diffusely atrophic retina in the patient’s right eye and subretinal fluid and diffuse cysts in the macula of his left eye with attached retina superiorly and retinal atrophy.

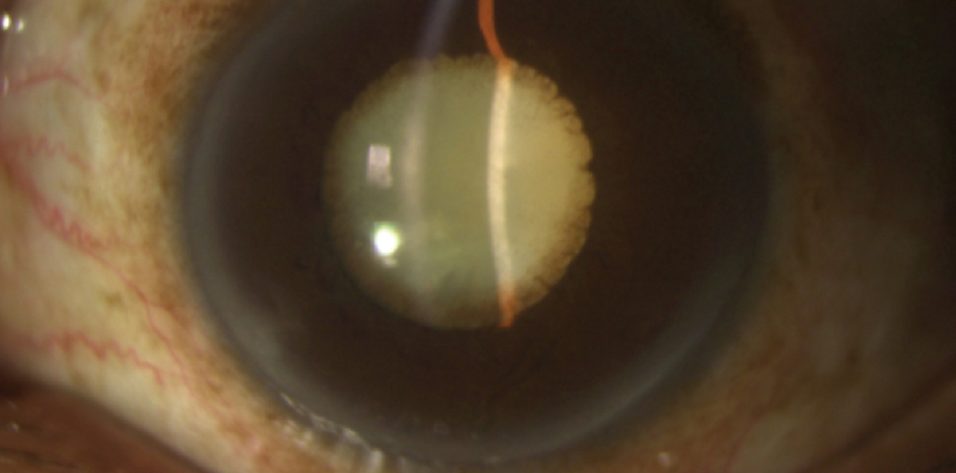
Figure 1. Exotropia in the right eye and a dense white cataract in each eye of a patient who is HIV positive and has a history of bilateral PORN.
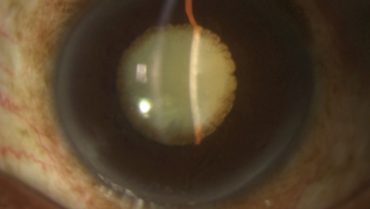
On presentation, the patient’s visual acuity is no light perception in his right eye and hand motions in his left. The IOP measures 6 mm Hg OD and 14 mm Hg OS. He has a right exotropia (Figure 1). There is a sectoral iridectomy superotemporally and iris pigment on the anterior lens capsule in the patient’s right eye (Figure 2). In his left eye, posterior synechiae are present for 360º, and there is iris bombé (Figure 3). A dense white cataract is present in each eye, and there is no view of the posterior pole.
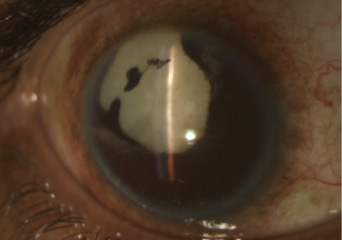
Figure 2. Sectoral iridectomy and dense white cataract in the patient’s right eye.

Figure 3. Dense white cataract with posterior synechiae and iris bombé in the patient’s left eye.
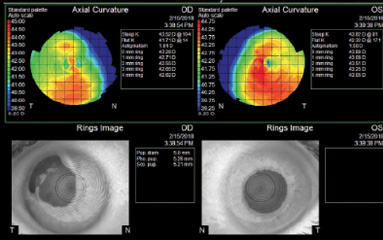
Figure 4. Topographic measurements.
Biometry is performed, but an axial measurement is possible only with immersion ultrasound in the patient’s right eye. Keratometry and topography readings are obtained for each eye (Figure 4).
What additional testing or information would you need prior to surgery? What concerns would you have with respect to the patient’s medical and/or ocular history? How would you determine the proper IOL power? Are there special intra- or postoperative concerns or considerations in this case? How would you counsel him regarding expectations?
—Case prepared by Cathleen M. McCabe, MD

RANA ALTAN-YAYCIOĞLU, MD, FEBO
Because of the patient’s history of subretinal fluid and diffuse cysts in the macula of his left eye, I would perform B-scan ultrasonography before proceeding to surgery. For an axial length measurement, the ultrasound biometry of the patient’s contralateral eye could be used. The eyes are filled with silicone oil, so adjustments for the different density of silicone oil and sound velocity should be made.
Also, corneal topography shows skewed asymmetric bow tie astigmatism in each eye. I would therefore inform the patient that he will likely have residual ametropia postoperatively and that his visual acuity may not improve with surgery.
Preoperatively, I would discuss with the patient the possible risks of surgery such as capsular rupture, intense inflammation, infection, and RD recurrence. Because he is HIV positive, he may be prone to infection, so I would start topical antibiotics prior to surgery.
Considering the presence of iris bombé, total posterior synechiae, and dense white cataract, I would use a heavy cohesive OVD to help prevent development of the Argentinean flag sign. I would use the OVD cannula to perform synechiolysis, insert iris hooks, and stain the capsule with trypan blue. After the capsulorhexis, I would proceed with standard phacoemulsification. My preference would be a three-piece hydrophobic acrylic IOL to minimize the potential for induced intraocular inflammation. Should I observe a capsular tear, I could still use this IOL, placed in the sulcus and/or with optic capture.

J.P. DUNN, MD
Given the patient’s no light perception vision, surgery is not indicated on his right eye in the absence of pain. The question is whether to perform cataract surgery on his left eye. Is there a realistic expectation that the visual acuity in his left eye can be improved? The retinal scarring, cystoid macular edema, and subretinal fluid in the patient’s left eye strongly suggest that the visual potential is very poor. It would help to know if there was a good view of the retina at some point after the RD repair and what the visual potential was at that time. Did the patient have ambulatory vision? If not, cataract surgery may not be indicated.
On the other hand, the patient’s monocular status and limited visual potential actually reduce some of the problems associated with cataract surgery in eyes with silicone oil. The most optimistic visual outcome is probably going to be 20/400 or less. Because IOL power calculations will have to be based on the axial length of the patient’s right eye and keratometry readings of his left, a postoperative refractive surprise is likely. That said, an error of 3.00 D or more will not cause anisometropia, and postoperative astigmatism is not going to be an issue. In these cases, the eyes typically have a dense posterior capsular plaque that cannot be successfully polished at the time of surgery, and subsequent Nd:YAG laser capsulotomy often fails to remove the opacity from the visual axis because of the anterior tamponade effect of the silicone oil. If the goal of surgery is a visual acuity of 20/400 or less, however, a capsulotomy may not even be necessary.
Because of the iris bombé and shallow chamber, the first intraoperative challenge will be forming a deeper chamber. In eyes without silicone oil, a limited pars plana vitrectomy can markedly deepen the anterior chamber and provide adequate working space. Intravenous hyperosmotic agents can be given to soften nonvitrectomized eyes and reduce the vitreous volume, but they will not be helpful in an oil-filled eye. In this case, it may be necessary to remove some of the oil to provide similar deepening, but, of course, this will have to be done blindly because of the white cataract, requiring collaboration with a vitreoretinal surgeon. Next, a peripheral iridectomy should be performed because synechiae may recur after surgery. Via the iridectomy, the anterior segment surgeon can perform viscodissection between the posterior iris and anterior lens capsule to break broad posterior synechiae, after which any residual pupillary membrane can be peeled through the phaco wound.
Eyes with a history of PORN and RD surgery are at increased risk of zonular disruption as a result of corticocapsular adhesions, chronic uveitis, prior intravitreal injections, and zonular damage from vitrectomy. Care should be taken to avoid overfilling the anterior chamber with an OVD, which could stretch loose zonules to the breaking point. Stretching with iris expanders or hooks will be necessary. After the anterior capsule is stained with trypan blue, a large capsulorhexis will facilitate manipulation of the cataract. The main drawback to a large capsulorhexis—IOL decentration caused by progressive centripetal fusion of the anterior and posterior capsules peripheral to the edge of the optic—is unlikely to cause visual problems in an eye such as this one.
Adequate pupillary dilation will be key in this case. Despite the availability of various devices for pupillary expansion, I prefer flexible iris hooks because they take up less space in the anterior chamber and do not interfere with visualization of the zonules if phacodonesis is noted intraoperatively or if the capsulorhexis extends peripherally. In my experience, white cataracts in eyes such as this one tend to be relatively dense, as opposed to the fluffy white cataracts seen in younger patients that are associated with increased osmotic pressure and a high risk of the Argentinean flag sign. These dense white cataracts generally do not cause the severe convexity of the anterior capsule that promotes peripheral capsulorhexis extension.
Effective capsular staining cannot be accomplished until the pupil is well dilated, so there will be OVD in the eye. Staining in such cases is best done by sweeping the trypan blue cannula gently over the capsular surface to create a potential space and then performing the same maneuver while gently injecting just a few drops of the dye. I find that this technique provides excellent capsular staining and minimizes the possibility of the dye’s extending posteriorly through an area of zonular dehiscence. Relatively dense cataracts lend themselves to sculpting and cracking, although they sometimes break apart into thin, flat sheets (like schist rock) that are tricky to aspirate. It is important to irrigate the angle and behind the iris at the end of surgery to ensure that no small lens fragments are left behind. My preference would be a three-piece IOL with a 6.5-mm optic because the pupil may remain dilated. Moreover, the stiff haptics can provide some zonular support. A silicone IOL should be avoided.
I would not recommend removing the silicone oil because there is a high risk of recurrent RD in an eye with a history of PORN. A vitreoretinal specialist should carefully examine the eye after placement of a posterior chamber IOL to see if additional oil should be injected to replace what was removed at the start of cataract surgery.

GRACE LEVY-CLARKE, MD
The spectrum of herpetic necrotizing retinopathies includes PORN and acute retinal necrosis (ARN). Both may be caused by VZV, but ARN can also be caused by herpes simplex type 1 or type 2. Typically, PORN is described in AIDS, usually advanced, with CD4+ T lymphocyte counts lower than 50 cells and other immunocompromised states. In contrast, ARN may be described in HIV negative or positive patients. In PORN, there is usually little or no inflammatory reaction, whereas in ARN there is usually prominent vitreal and/or anterior chamber inflammation.1,2
The 360º of posterior synechiae in the patient’s left eye implies previous moderate or severe anterior inflammation, which is suggestive of ARN rather than PORN. The patient’s left eye may have a somewhat better overall prognosis than his right. Specifically, the current visual acuity of no light perception in his right eye suggests retinal atrophy with photoreceptor necrosis and, thus, no recoverable vision.1
Published guidelines on long-term suppressive therapy for herpes simplex infection (ARN) in HIV patients at risk recommend valacyclovir 500 mg/famciclovir 500 mg or acyclovir 400 mg by mouth twice per day, double the patient’s current dosing. Prophylaxis for VZV (PORN) infection in HIV-infected patients has not been examined, however, and is not routinely recommended. More important, the antiretroviral regimen is key to preventing recurrence.3 Coordination of care with the patient’s infectious disease specialist will therefore be critical in this case to determine the appropriate level of perioperative antiviral and antiretroviral therapy.
In 1996, Meldrum and colleagues published a comprehensive review of the surgical nuances in cataract extraction after silicone oil repair for RD due to necrotizing retinitis. The article delineated the process and recommended a three-step modification of IOL power calculations.4 A 2018 publication by Al-Habboubi and colleagues discussed the merit of combining cataract surgery and silicone oil removal, with additional retinal procedures performed at the surgeon’s discretion. In the series, this approach restored functional vision in one-third of the cases (98 eyes), and the underlying ocular pathologies were heterogeneous.5

WHAT I DID: CATHLEEN M. MCCABE, MD
B-scan ultrasonography proved impossible in each eye. After consultation with a uveitis specialist in my area, I obtained the patient’s most recent laboratory results, including an absolute CD4+ T lymphocyte count of 554 and an HIV viral load by polymerase chain reaction testing that was detectable but too low to quantify. The patient was instructed to continue his oral antiviral medication. After he and I discussed the guarded visual outcome of surgery, he elected to proceed with cataract removal in his left eye in hopes of improving his visual acuity and to allow assessment of the health of the retina and optic nerve.
In eyes with white intumescent lenses, I prefer to make the capsulotomy with a femtosecond laser. Despite 360º of posterior synechiae and iris bombé, the pupil was large enough for me to make my usual 5-mm capsulotomy. Anterior segment OCT with the LenSx Laser (Alcon) showed the iris bombé and a thick membrane across the pupil that was indistinguishable from the anterior capsule (Figure 5). I increased the power setting on the laser and performed the capsulotomy in my usual fashion.
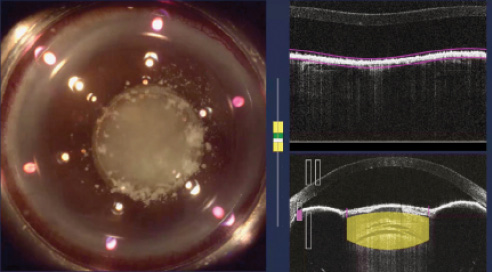
Figure 5. Anterior segment OCT during treatment with a femtosecond laser shows iris bombé, posterior synechiae, and a dense fibrotic pupillary membrane.
Upon entering the anterior chamber with a diamond blade, I observed a membrane on the anterior surface of the iris that covered the pupil. There was a 5-mm opening in this pupillary membrane. Using a dispersive OVD (Viscoat, Alcon), I released the posterior synechiae. After peeling the membrane off the surface of the anterior segment structures, I encountered an intact anterior capsule that was extremely thick, fibrotic, and resistant to tearing, even with a two-handed technique. I used intraocular scissors to create a central capsulotomy and removed the nucleus with a vertical chopping technique.
The entire capsule was thick, loose, and opacified, and it appeared to be supported only by the adhesions between the capsule and the iris. I removed the entire fibrotic, calcified capsular bag from the patient’s eye. I noted a red reflex along with silicone oil filling the posterior chamber. I decided to leave the eye aphakic in order to determine whether visual potential was sufficient to warrant a sewn-in or sulcus-fixated IOL, in which case I would attempt sulcus fixation of a three-piece IOL in the future.
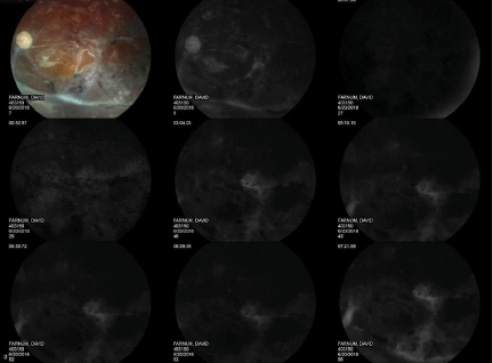
Figure 6. Color fundus photography and fluorescein angiography of the patient’s left eye after cataract extraction.
On postoperative examination, I found diffuse and profound optic nerve and retinal atrophy and diffuse retinal ischemia (Figure 6). There was preretinal fibrosis along the inferior arcade and a localized tractional RD. At postoperative week 1, the patient’s visual acuity remained hand motion, and I advised him that it was unlikely to improve, even with glasses or contact lenses. Three and a half weeks after surgery, however, his visual acuity had improved to 20/200 with a manifest refraction of 10.00 D sphere.
1. Austin RB. Progressive outer retinal necrosis syndrome: a comprehensive review of its clinical presentation, relationship to immune system status, and management. Clin Eye Vis Care. 2000;12(3-4):119-129.
2. Woo SJ, Yu HG, Chung H. A case of atypical progressive outer retinal necrosis after highly active antiretroviral therapy. Korean J Ophthalmol. 2004;18(1):65-69.
3. Clinical guidelines. US Department of Health and Human Services website. https://aidsinfo.nih.gov/guidelines. Accessed July 12, 2018.
4. Meldrum ML, Aaberg TM, Patel A, Davis J. Cataract extraction after silicone oil repair of retinal detachments due to necrotizing retinitis. Arch Ophthalmol. 1996;114(7):885-892.
5. Al-Habboubi H, Al-Zamil W, Al-Habboubi A, Khandekar R. Visual outcomes and refractive status after combined silicone oil removal/cataract surgery with intraocular lens implantation. J Ophthalmic Vis Res. 2018;13(1):17-22.