Surgical Visualization
by Cristos Ifantides, MD, MBA

The allure of 3D visualization with systems such as the Artevo 800 (Carl Zeiss Meditec) and Ngenuity (Alcon) is growing. The technology can improve surgeon ergonomics and lends itself to patient education, but traditional nondigital microscopes remain a reasonable choice for ophthalmologists who value cost-effectiveness, visual quality, space efficiency, and a well-organized OR.
COST-EFFECTIVENESS
Purchasing a 3D visualization system can strain the budget of a clinic or hospital, especially one located in a developing region. The strain is more pronounced if multiple displays must be bought to reap the benefits of the system.
Traditional microscopes, although expensive, are a more affordable solution that does not compromise surgical outcomes. Maintaining and repairing these traditional systems, given their simpler mechanics and fewer electronic components, is also more affordable in the long run.
UNPARALLELED VISUAL QUALITY FOR THE SURGEON
A benefit attributed to 3D visualization systems is enhanced depth perception, which, in theory, aids surgery. Visual quality, however, depends on an optimal viewing angle and distance, which may not be achievable in every OR. Additionally, only one perspective is available on the display, leaving surgical assistants to guess where they are in space when entering the surgical field.
The optical systems of traditional microscopes have been refined over decades to provide crisp, clear, realistic visualization. The fidelity of what the human eye sees directly through quality oculars is unmatched. In converting optical images to electronic signals, digital systems could introduce minor distortions or delays, however imperceptible they are claimed to be.
SPACE EFFICIENCY
With their attendant computers, monitors, and additional cables, 3D systems can have a large footprint in the OR. This not only limits the movement and comfort of the surgical team but also poses a tripping hazard and spatial constraints, especially in a small OR or mobile surgical unit.
The average traditional microscope in the United States is not small, but it is smaller and more mobile than a digital system. Newer companies such as EyeMobile, moreover, are designing smaller microscopes that are mobile.
OR ARRANGEMENT
The simplicity of traditional microscopes is highly advantageous when setting up an OR. The instruments integrate seamlessly into most surgical settings. When switching between right and left eyes, the microscope can be rolled to the other side of the patient, or its arm may simply be rotated. In contrast, 3D systems require specific arrangements, connections to viewing screens, and sometimes even two 3D displays in one OR so as not to disturb other stationary equipment such as a femtosecond laser, a phaco machine, and tables.
CONCLUSION
3D visualization systems undeniably represent a leap forward in technological prowess, but the cost-effectiveness, visual quality, compact footprint, and easy integration of traditional microscopes are compelling. The developers of 3D visualization systems are aware of their shortcomings and are developing platforms that could compete successfully with traditional microscopes in the next few years.
LASIK 3D: The Next Revolution
By David Smadja, MD

Musculoskeletal disorders are a concern for ophthalmologists. In an online survey of members of the Maryland Society of Eye Physicians and Surgeons, 66% of respondents reported experiencing work-related pain.1 The use of 3D heads-up digital microscopes has been shown to decrease back and cervical pain significantly for ophthalmologists during surgery.2 The technical simplicity and short duration of laser vision correction procedures, however, have historically relegated ergonomics to an afterthought for the most part.
In assessing the impact on ergonomics and comfort, I integrated the Ngenuity Digital 3D Visualization System with the WaveLight EX500 excimer laser (both products from Alcon) during a full schedule of corneal surgeries. Replacing the laser system’s regular microscope eyepieces with the 3D camera was simple. It took only about 2 minutes to switch from one visualization system to the other (Figure 1). This article shares my observations.

Figure 1. A simple setup process enhances surgical ergonomics without compromising procedural time.
PATIENT PERSPECTIVE
The 3D visualization system’s digital image processing permitted low perioperative light exposure for patients3 without compromising illumination for me, the surgeon. This reduction in glare not only improved patient comfort but also lessened the chance of unwanted intraoperative ocular movements.
SURGEON PERSPECTIVE
The learning curve was rapid. The transition from traditional microscope eyepieces to the 3D system for laser vision correction was seamless for me. By the third procedure, I forgot I was not looking into my regular microscope eyepieces. I perceived no delay in the high-resolution camera’s transmission of real-time images to a single screen in front of me (Figure 2). I also appreciated an increase in image clarity and the depth of the surgical field.
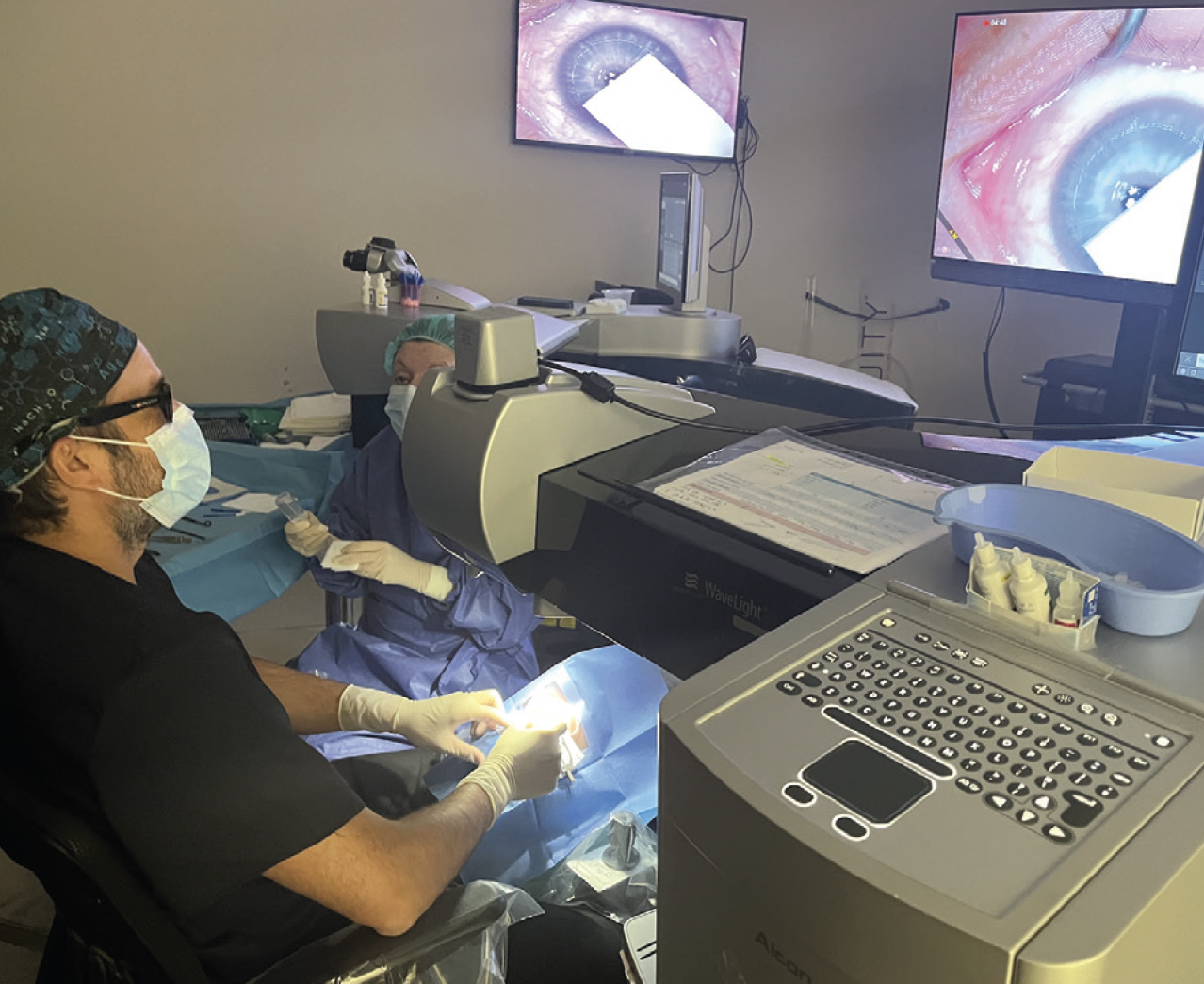
Figure 2. The high-resolution camera of the 3D system transmits detailed surgical images to the monitor, facilitating a seamless operative experience.
What made the 3D setup for LASIK a game-changer for me, however, was an immediate reduction in my neck and back discomfort during surgery. I was able to maintain a more natural posture while operating (Figure 3).
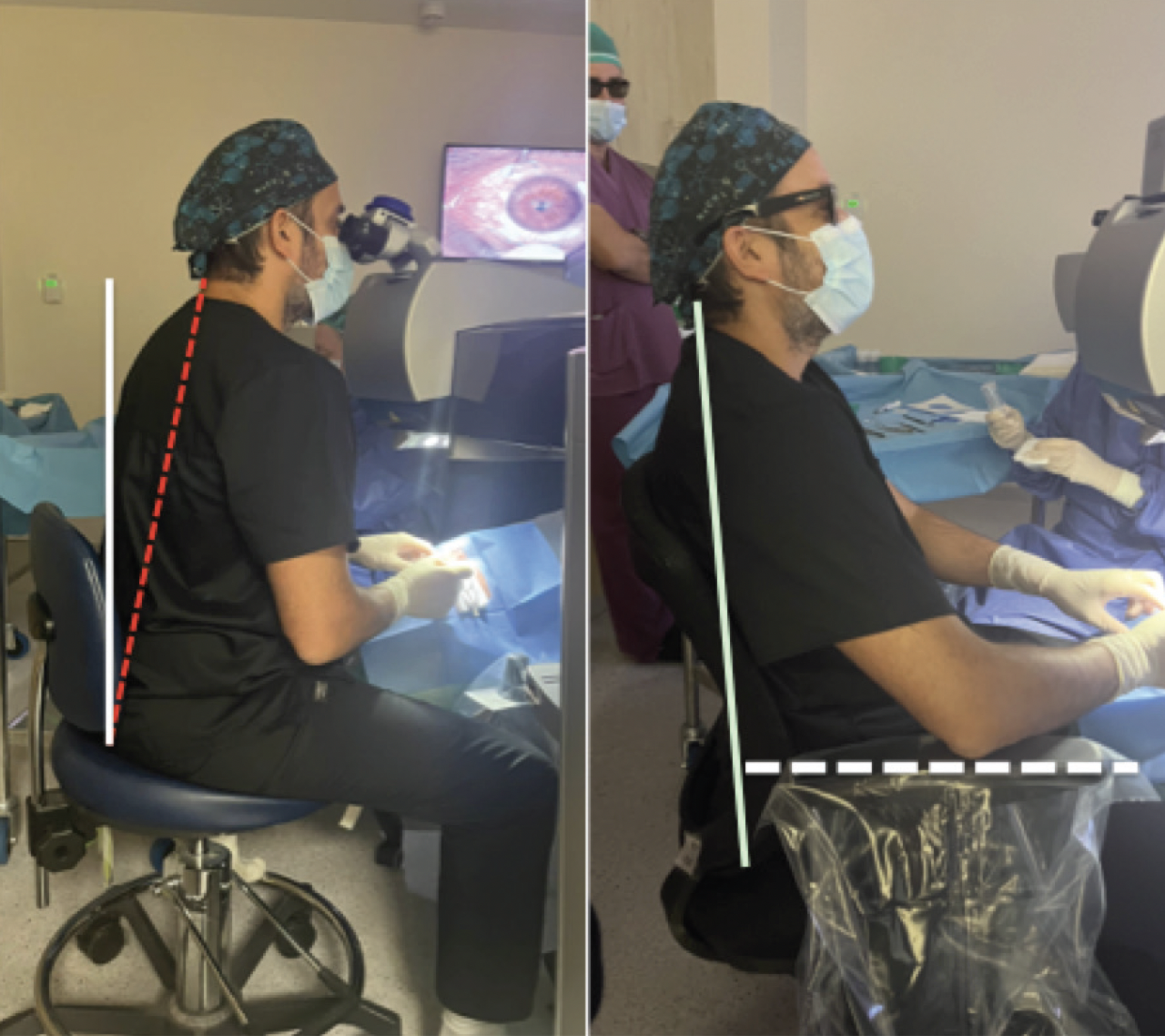
Figure 3. The surgeon operating with the 3D system, illustrating the improved posture and reduced physical strain during LASIK procedures.
CONCLUSION
The use of a 3D heads-up visualization system during LASIK is a natural step forward for surgeons and their patients. It promises immediate ergonomic advantages, with substantial benefits for surgeon health and procedural comfort.
1. Schechet SA, DeVience E, DeVience S, Shukla S, Kaleem M. Survey of musculoskeletal disorders among US ophthalmologists. Digit J Ophthalmol. 2020;26(4):36-45.
2. Cheng TC, Yahya MFN, Mohd Naffi AA, et al. Evaluation of three-dimensional heads-up ophthalmic surgery demonstration from the perspective of surgeons and postgraduate trainees. J Craniofac Surg. 2021;32(7):2285-2291.
3. Gualino V, Pierne K, Manassero A, Bruneau S, Couturier A, Tadayoni R. Comparing microscope light-associated glare and comfort between heads-up 3D digital and conventional microscopes in cataract surgery: a randomized, multicenter, single-blind, controlled trial. BMJ Open Ophthalmol. 2023;8(1): e001272.