A 48-year-old man presented for artificial iris (AI) evaluation in the left eye. He had a history of penetrating keratoplasty (PKP) in both eyes for keratoconus. Six months prior to this visit, he was hit with a baseball, which resulted in dehiscence of the graft and loss of native iris and lens of the left eye. He underwent ruptured globe repair and was left aphakic and aniridic. Postoperatively, he reported severe vision loss, glare, and photophobia.
On examination, the patient’s UCVA of the left eye was count fingers at face, and pinhole 20/40; IOP measured 18 mm Hg. No relative afferent pupillary defect was detected, and confrontational visual fields were full for both eyes. External examination showed a left sensory exotropia (Figure 1). Slit-lamp examination revealed an eccentric PKP with graft failure, corneal edema, significant scarring, complete aniridia, and aphakia. Fundus examination was normal. The patient elected to proceed with treatment in the form of AI implantation/IOL implantation and PKP.

Figure 1. Preoperative photograph shows left exotropia, corneal scarring, complete aniridia, and aphakia of the left eye.
The Surgery
Intraoperatively, the fiber-containing AI implant (CustomFlex ArtificialIris; HumanOptics) was trephined to 11 mm. A single-piece polymethyl methacrylate IOL (CZ70BD; Alcon) was fixated to the posterior aspect of the artificial iris with a 9-0 polypropylene suture (Prolene; J&J MedTech). Polytetrafluoroethylene suture (Gore-Tex; Gore Medical) was threaded through the artificial iris in a horizontal mattress fashion 180° apart. A 9.5-mm scleral tunnel was created superiorly and sclerotomies were fashioned nasally and temporally. The Gore-Tex sutures were retrieved through the sclerotomies using 25-gauge MST forceps. The AI-IOL complex was inserted into the posterior chamber, and the wound was sutured. The Gore-Tex was tied, and knots were buried within the sclerotomies. The donor cornea was manually trephined to 8.75 mm, and the recipient cornea was trephined to 8.25 mm. The diseased cornea was removed and the donor tissue was sutured with 17 interrupted 10-0 nylon sutures.
At 5 months postoperatively, UCVA was 20/150, pinhole 20/40, and IOP was 12 mm Hg. The cornea was clear, and the AI-IOL complex was well-centered. Importantly, the patient’s glare, photophobia, and sensory exotropia were markedly improved. (Figure 2).
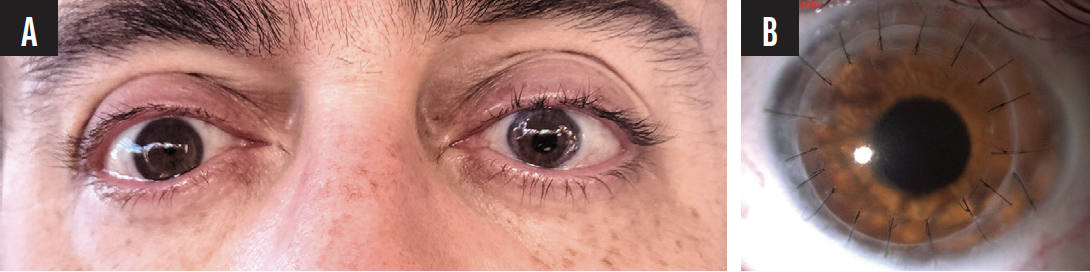
Figure 2. Postoperative photographs show resolution of the exotropia and a well-centered artificial iris in the left eye that was custom-made to match the patient’s native iris tissue in the right eye (A). Postoperative slit-lamp photo of the PKP, AI, and IOL in the left eye (B).
Discussion
The CustomFlex ArtificialIris was FDA-approved in 2018 for the treatment of large iris defects resulting from congenital aniridia, acquired defects, or other conditions associated with aniridia. A common cause of acquired iris defect is trauma; it is often associated with other sequelae such as aphakia and corneal scarring. A prospective case series that examined clinical outcomes of AI and IOL implantation combined with PKP found that the triple procedure resulted in improved corrected distance VA, cosmesis, and quality of life.1 Nevertheless, various postoperative complications were noted, the most common being iritis, secondary graft failure, and elevated IOP.
Conclusion
With careful preoperative planning, combining PKP with AI and secondary IOL implantation can be an effective technique for visual and cosmetic rehabilitation in patients with corneal pathology, aniridia, and aphakia. Patients must be monitored closely postoperatively owing to an increased risk of postoperative complications that may require medical or surgical intervention.
1. Bonnet C, Vazirnia P, Deng SX, Aldave AJ, Miller KM. Sutured Custom Foldable Silicone Artificial Iris Implantation Combined With Intraocular Lens Implantation and Penetrating Keratoplasty: Safety and Efficacy Outcomes. Cornea. 2021;40(10):1236-1247.


