Outdated or up-to-date?
By Erika N. Eskina, MD; Walter Sekundo, MD, PhD; and Bojan Pajic, MD, PhD, FEBO



Presbyopia remains an unsolved challenge. Reading and progressive glasses, corneal inlays, multifocal contact lenses and IOLs, extended depth of focus IOLs, small-aperture IOLs, and excimer laser ablation can alleviate or delay its symptoms. None of these methods, however, restores accommodation.1-3 Instead, patients must be willing to compromise on optical and image quality, depth of focus, and stereopsis and often wait for neural adaptation.2,4
Ideally, presbyopia correction would eliminate ametropia and restore accommodation without sacrificing binocular vision, contrast sensitivity, and stereo acuity. This article discusses progress in presbyopic laser vision correction (LVC) toward that goal.
CURRENT TECHNIQUES
The trend in both intraocular and corneal surgery is toward minimizing anisometropia while increasing depth of focus.3,5-7 After some missteps and controversy over methods and ideas, the field of ophthalmology has made tremendous advances in corneal presbyopia correction with excimer lasers. The timing is good because the number of people with presbyopia is growing. In Europe—where we practice—an estimated 338 million individuals will be presbyopic by 2029. The market is expected to exceed €13 billion.8
Most current presbyopia-correcting LVC techniques ablate the central cornea to optimize near focus, correct spherical aberration (positive or negative), and induce a minimal amount of anisometropia.9-11 A less common approach targets the dominant eye for distance. A third strategy creates a multifocal corneal surface on either one eye or both eyes (Figure 1).6
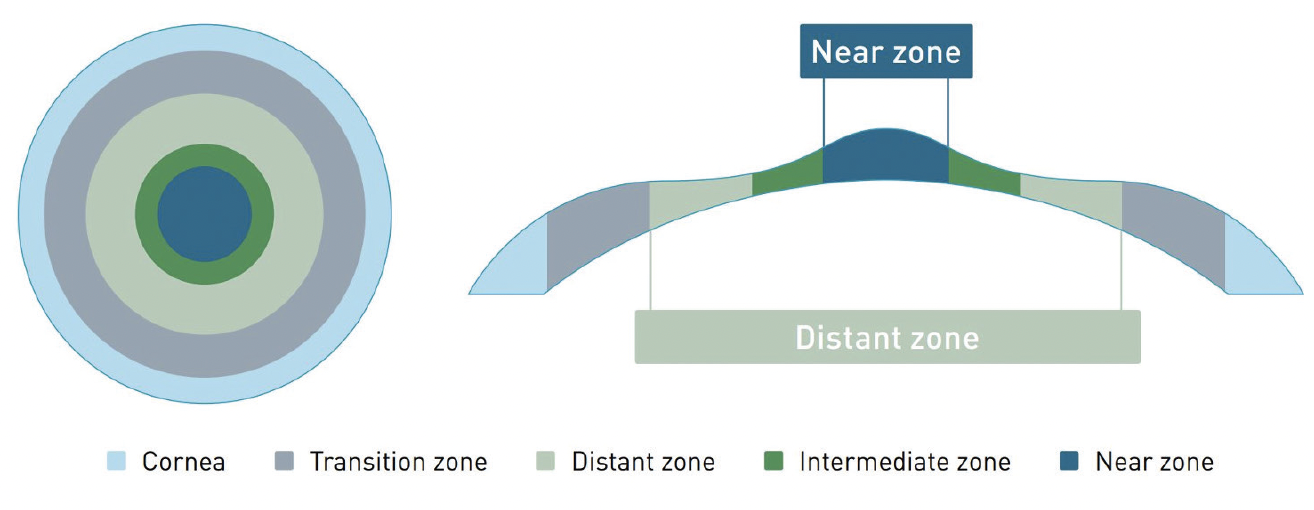
Figure 1. LVC creates a multifocal central cornea.
LVC VERSUS INTRAOCULAR SURGERY
Predictability. One advantage of presbyopic LVC is greater predictability compared to intraocular surgery.6,12 The predictability of refractive results with LVC may decrease slightly if the amount of preoperative spherical aberrations is high.12,13
Anatomy. Unlike refractive lens exchange (RLE), LVC preserves the ocular anatomy and thus whatever accommodative amplitude a patient had preoperatively. Presbyopic LVC can also be a better option for patients with axial myopia because of their increased risk of retinal detachment after RLE.14,15
Retreatment. As noted earlier, presbyopic LVC reduces binocular distance visual acuity, contrast sensitivity, and stereopsis. Additionally, a second treatment may be required to increase the effect of presbyopia correction as patients age.12,16
IOL dislocation. People who undergo lens surgery when they are 40 to 50 years of age are at greater risk of IOL dislocation than those who undergo lens surgery for age-related cataracts.17
Cataract. RLE eliminates a patient’s future need for cataract surgery. In contrast, presbyopic LVC may make future IOL power calculation and selection more difficult. Obtaining biometry measurements before LVC or performing presbyopic LASIK with a wavefront-guided excimer laser system may help address these issues.18-20
There are also long-term considerations for patients who have undergone LVC, such as the choice and accuracy of IOL calculations for cataract surgery. Variables such as corneal power, axial length, and the effective lens position of the IOL after cataract surgery affect calculations. In virgin eyes, one can obtain accurate measurements with a high degree of confidence. After refractive surgery, however, it is difficult to measure the cornea exactly, making it harder for surgeons to achieve the desired postoperative target. It should be noted that the improvement of IOL calculation formulas allows surgeons to achieve more accurate results with IOL calculations after LVC.21-25 Reinstein et al reported in 2019 that the extended focus effect was preserved in 92 eyes that underwent laser blended vision correction with aspheric IOLs. Pajic et al achieved similar results in 28 eyes in 2021.13
CUSTOMIZED LVC
Some excimer laser manufacturers offer customized approaches to presbyopic LVC. The optical results targeted for the dominant eye are tailored to the individual’s visual needs. Multifocality is created, and depth of focus is increased through the surgical induction of spherical aberrations and scope for myopic and hyperopic patients. Eyes with myopia and hyperopia, however, receive different amounts of multifocality owing to the nature of the refraction. The treatment approach is also influenced by the intended micro-monovision. Because spherical aberrations reduce contrast sensitivity, modifications must be made carefully.26
During customized presbyopic LVC, a micro-monovision strategy typically aiming for -0.75 to -1.00 D of spherical anisometropia and targeting the nondominant eye for near vision is generally used (Figure 2).6,27

Figure 2. Range of vision at all distances after treatment with PresbyMAX in the dominant and nondominant eyes.
Courtesy of Schwind eye-tech-solutions
Option No. 1: The dominant eye is targeted for distance vision with a modification of spherical aberration to minimize the impact on quality of vision.
Option No. 2: The depth of focus targeted in the dominant and nondominant eyes differs but is generally greater in the nondominant eye. This is thought to provide good spatial vision.
Option No. 3: The same depth of focus is targeted in both eyes.
Customized presbyopic LVC bears a similarity to the mix-and-match concept used in RLE, where the IOL implanted in the dominant eye provides better distance vision with a shallower depth of focus or multifocality.26,27 Any discussion of presbyopia correction should include the pinhole effect with a small-aperture IOL to increase depth of focus (Figure 3).
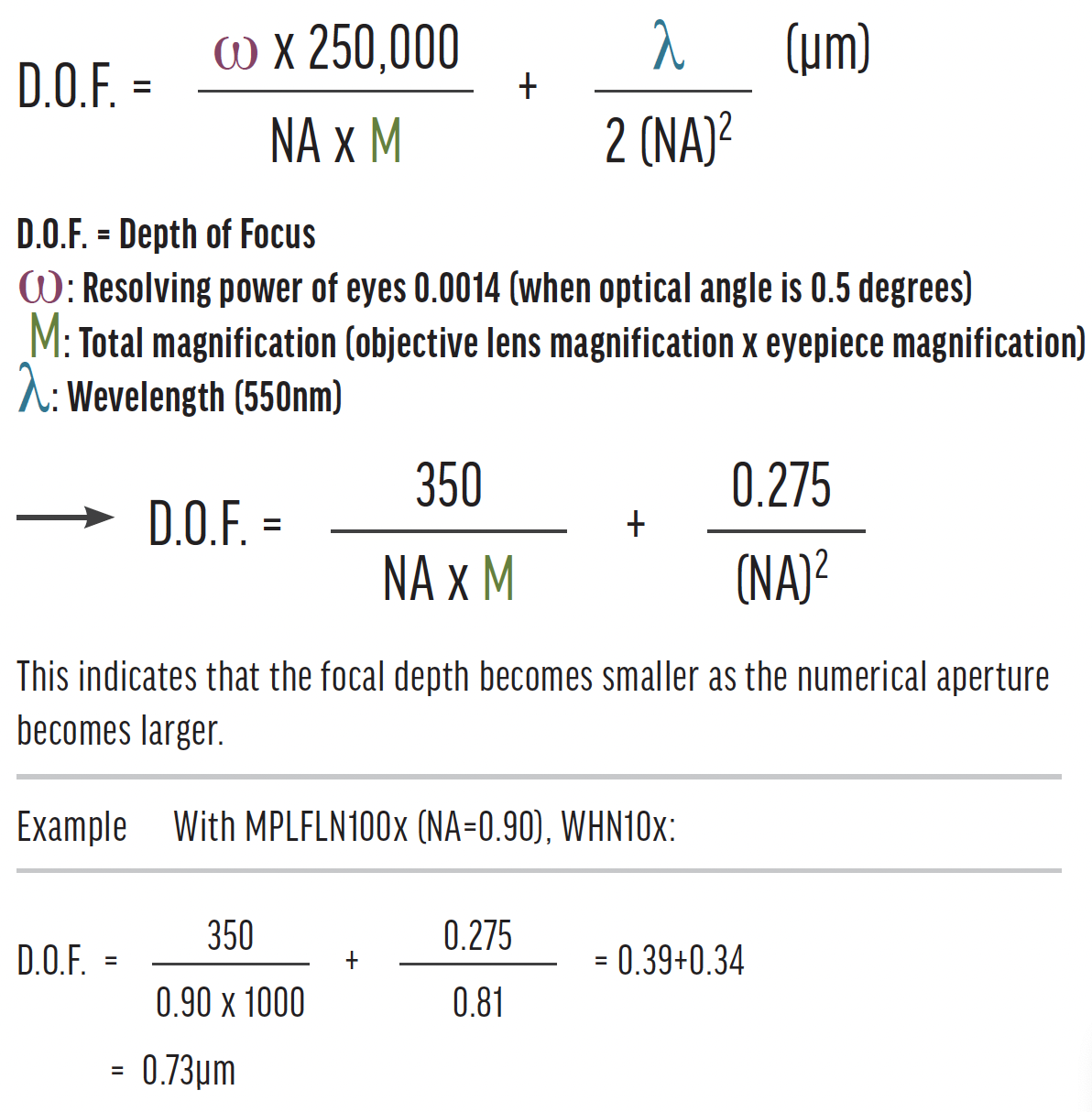
Figure 3. Max Berek’s formula for depth of focus.
CONCLUSION
Presbyopic LVC offers customized solutions for patients. The technology and techniques continue to evolve.
1. Łabuz G, Yan W, Baur ID, Khoramnia R, Auffarth GU. Comparison of five presbyopia-correcting intraocular lenses: optical-bench assessment with visual-quality simulation. J Clin Med. 2023;12(7):2523.
2. Pajic B, Massa H, Eskina EN. Presbyopiekorrektur mittels Laserchirurgie. Klein Monbl Augenheilkunde. 2017;234(9):e29-e42.
3. Reinstein DZ, Archer TJ, Gobbe M. Laser blended vision for presbyopia correction. In: Pallikaris I, Plainis S, Charman WN, eds. Presbyopia: Origins, Effects, and Treatment. Slack: 2012;22:191-197.
4. Reinstein DZ, Carp GI, Archer TJ, Gobbe M. LASIK for the correction of presbyopia in emmetropic patients using aspheric ablation profiles and a micro-monovision protocol with the Carl Zeiss Meditec MEL80 and VisuMax. J Refract Surg. 2012;28(8):531-541.
5. Russo A, Reinstein DZ, Filini O, et al. Visual and refractive outcomes following laser blended vision with non-linear aspheric micro-anisometropia (PRESBYOND) in myopic and hyperopic patients. J Refract Surg. 2022;38(5):288-297.
6. Shetty R, Brar S, Sharma M, Dadachanji Z, Lalgudi VG. PresbyLASIK: a review of PresbyMAX, Supracor, and laser blended vision: principles, planning, and outcomes. Indian J Ophthalmol. 2020;68(12):2723-2731.
7. Danzinger V, Schartmüller D, Schwarzenbacher L, et al. Clinical prospective intra-individual comparison after mix-and-match implantation of a monofocal EDOF and a diffractive trifocal IOL. Eye (Lond). Published online July 31, 2023. doi:10.1038/s41433-023-02682-x
8. Data Bridge Market Research. Global Presbyopia Market – Industry Trends and Forecast to 2029. May 2022. Accessed October 31, 2023. https://www.databridgemarketresearch.com/reports/global-presbyopia-market
9. Agarwal S, Thornell E. Early outcomes of two treatment modes of PresbyLASIK: monocular vs. micro-monovision. Clin Ophthalmol. 2022;16:3597-3606.
10. Russo A, Reinstein DZ, Filini O, et al. Visual and refractive outcomes following laser blended vision with non-linear aspheric micro-anisometropia (PRESBYOND) in myopic and hyperopic patients. J Refract Surg. 2022;38(5):288-297. Erratum in: J Refract Surg. 2022;38(7):474.
11. Saib N, Abrieu-Lacaille M, Berguiga M, Rambaud C, Froussart-Maille F, Rigal-Sastourne JC. Central PresbyLASIK for hyperopia and presbyopia using micro-monovision with the Technolas 217P platform and SUPRACOR algorithm. J Refract Surg. 2015;31(8):540-546.
12. Fu D, Aruma A, Xu Y, Han T, Xia F, Zhou XT. Refractive outcomes and optical quality of PRESBYOND laser-blended vision for presbyopia correction. Int J Ophthalmol. 2022;15(10):1671-1675.
13. Pajic B, Massa H, Baenninger PB, et al. Multifocal femto-PresbyLASIK in pseudophakic eyes. J Clin Med. 2021;10(11):2282.
14. Javaloy J, Rivera E, Montalbán R, Beltrán J, Muñoz G, Rohrweck S. Diffractive trifocal pseudophakic intraocular lenses in high myopic eyes: 2-year assessment after implantation. Graefes Arch Clin Exp Ophthalmol. 2019;257(6):1331-1339.
15. Clark A, Morlet N, Ng JQ, Preen DB, Semmens JB. Risk for retinal detachment after phacoemulsification: a whole-population study of cataract surgery outcomes. Arch Ophthalmol. 2012;130(7):882-888.
16. Kohnen T, Böhm M, Herzog M, Hemkeppler E, Petermann K, Lwowski C. Near visual acuity and patient-reported outcomes in presbyopic patients after bilateral multifocal aspheric laser in situ keratomileusis excimer laser surgery. J Cataract Refract Surg. 2020;46(7):944-952.
17. Pueringer SL, Hodge DO, Erie JC. Risk of late intraocular lens dislocation after cataract surgery, 1980-2009: a population-based study. Am J Ophthalmol. 2011;152(4):618-623.
18. Al-Khateeb G, Shajari M, Kohnen T. Intraindividual comparative analysis of the visual performance after cataract surgery with implantation of a trifocal and a bifocal intraocular lens. J Cataract Refract Surg. 2017;43(5):695-698.
19. Wang L, Hill WE, Koch DD. Evaluation of IOL power prediction methods using the American Society of Cataract and Refractive Surgeons post-keratorefractive IOL power calculator. J Cataract Refract Surg. 2010;36(9):1466-1473.
20. Ianchulev T, Hoffer KJ, Yoo SH, et al. Intraoperative refractive biometry for predicting intraocular lens power calculation after prior myopic refractive surgery. Ophthalmology. 2014;121(1):56-60.
21. Olsen T. Calculation of intraocular lens power: a review. Acta Ophthalmol Scand. 2007;85(5):472-485.
22. Aramberri J. Intraocular lens power calculation after corneal refractive surgery: double-K method. J Cataract Refract Surg. 2003;29(11):2063-2068.
23. Fram NR, Masket S, Wang L. Comparison of intraoperative aberrometry, OCT-based IOL formula, Haigis-L, and Masket formulae for IOL power calculation after laser vision correction. Ophthalmology. 2015;122(6):1096-1101.
24. Arba Mosquera S. Visual acuity and blur: an extended depth-of-focus model. Eur J Ophthalmol. Published October 5, 2022. doi:10.1177/11206721221123883
25. Uthoff D, Pölzl M, Hepper D, Holland D. A new method of cornea modulation with excimer laser for simultaneous correction of presbyopia and ametropia. Graefes Arch Clin Exp Ophthalmol. 2012;250(11):1649-1661.
26. Koo OS, Kang JW, Park JK, Kim KH. Visual performance and patient satisfaction after implantation of extended range-of-vision IOLs: bilateral implantation vs 2 different mix-and-match approaches. J Cataract Refract Surg. 2021;47(2):192-197.
27. Bilbao-Calabuig R, González-López F, Amparo F, Alvarez G, Patel SR, Llovet-Osuna F. Comparison between mix-and-match implantation of bifocal intraocular lenses and bilateral implantation of trifocal intraocular lenses. J Refract Surg. 2016;32(10):659-663.




