Ocular surface squamous neoplasia (OSSN) is associated with a broad spectrum of clinical presentations, including conjunctival intraepithelial neoplasia, a non-invasive slow-growing tumor from a single cell origin; corneal epithelial dysplasia, or neoplasia, in which corneal epithelial islands are the dominant feature; and squamous cell carcinoma, in which a malignant lesion has gained invasive potential.1,2 Development of OSSN is multifactorial, involving a mix of environmental factors in a suspectable host.1 In epidemiologic surveys, OSSN is found more prevalent in geographic areas closer to the equator,3 suggesting a role for UV light exposure. Indeed, it has been found to most commonly occur in Caucasian men aged 60 to 70 years living close to the equator.4 Clinically, lesions are primarily found in the interpalpebral fissure where sun exposure is direct.1 OSSN is the only type of cancer with a comparable response to surgical or medical treatment.5 The decision is based on tumor location, extension, and patient preference.6 When treating extensive lesions, the preferred option is chemotherapy, as it treats the whole ocular surface and has a lower risk of limbal stem cell deficiency (LSCD) compared to extensive resections of tissue. We present a case of a patient who had a diffuse corneal OSSN with poor response to topical chemotherapy and developed severe LSCD after tumor excision with cryotherapy.
Presentation
This is a case of a 60-year-old male patient with a diffuse OSSN of the left eye. Medical history included a history of anal warts, sun exposure as a child, and hypertension. For the OSSN, he was treated with two cycles of Interferon eyedrops, two cycles of 5-Fluorouracil eyedrops, and two cycles of Mitomycin C topical chemotherapy without improvement. Due to high out-of-pocket costs and the development of epitheliopathy after 7 months of treatment, he decided to abandon chemotherapy and start Aloe Vera eyedrops, which improved his condition, and chemo reduced the lesion. He then underwent a 6-clock-hour tumor excision, which successfully removed the tumor but resulted in the development of limbal stem cell deficiency (Figure 1).
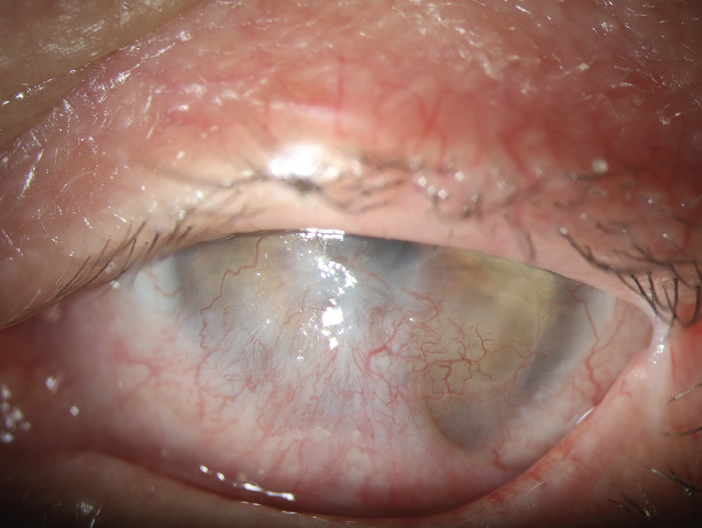
Figure 1. Severe limbal stem cell deficiency in the left eye of a 60-year-old patient.
Treatment
After consultation with the patient, he underwent ocular surface reconstruction and simple limbal epithelial transplantation (SLET). Before this procedure, the patient’s best corrected visual acuity (BCVA) was counting fingers at 2 feet; 3 months after the procedure, BCVA was 20/40 (Figure 2). A scleral lens will be considered in the future due to severe dry eye and residual corneal irregularity.
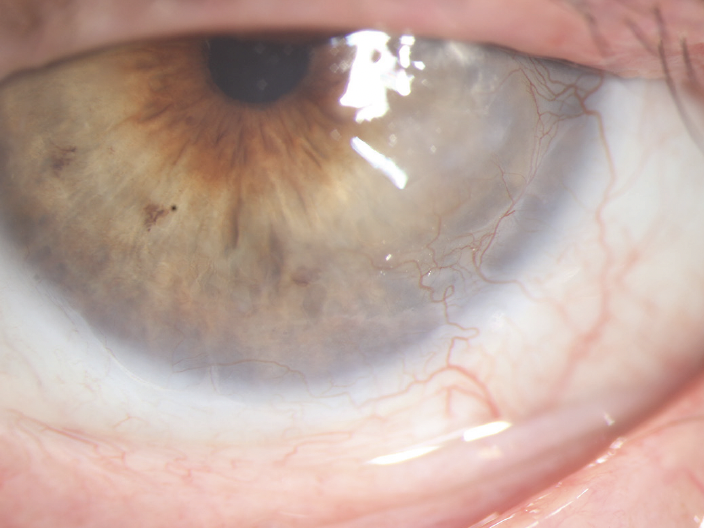
Figure 2. Slit-lamp photography of the left eye, 3 months after SLET.
Summary
First described in 2012 as a technique to treat limbal stem cell deficiency,7 SLET involves harvesting healthy limbal cells from a healthy eye for autologous transplantation.8 SLET may have several advantages relative to other techniques for limbal transplantation.9,10,11 For example, it is a one-stage procedure requiring no particular setup, thus making it cost-effective.7 SLET requires a smaller donor graft than other limbal stem cell transplantation techniques. Although initially explicitly described for unilateral 360° stem cell deficiency, it has also been successfully used in partial limbal stem cell deficiency. This is an excellent visual and anatomical rehabilitation option for patients with LSCD.
Learning points
- Various treatment options for OSSN range from antineoplastics to homeopathic medicine.
- The best option for diffuse OSSN is medical chemotherapy, as wide margins are difficult to identify, but while it is usually successful, it doesn’t always work.
- Surgery is another modality that is often successful but doesn’t always work and can cause LSCD.
- PRGF membrane is an alternative to minimize corneal scarring in the ocular surface with imminent LSCD.
- Simple limbal epithelial transplantation is an excellent option for ocular surface reconstruction in cases of unilateral LSCD.
1. Krachmer JH, Mannis MJ, Holland EJ. Cornea: Fundamentals, diagnosis and management. 2005.
2. Reidy JJ, Bouchard CS, Florakis GJ, et al. Basic and Clinical Science Course, 2011-2012. 2011:226-233.
3. Karp CL, Scott IU, Chang TS, Pflugfelder SC. Conjunctival Intraepithelial Neoplasia: A Possible Marker for Human Immunodeficiency Virus Infection? Arch Ophthalmol. 1996;114:257-261.
4. Basti S, Macsai MS. Ocular surface squamous neoplasia: a review. Cornea. 2003;22:687-704.
5. Nanji AA, Moon CS, Galor A, et al. Surgical versus medical treatment of ocular surface squamous neoplasia: a comparison of recurrences and complications. Ophthalmology. 2014;121(5):994-1000.
6. Mercado CL, Pole C, Wong J, Batlle JF, Roque F, Shaikh N, Murillo JC, Galor A, Karp CL. Surgical versus medical treatment for ocular surface squamous neoplasia: A quality of life comparison. Ocul Surf. 2019;17(1):60-63.
7.Sangwan VS, Basu S, MacNeil S, Balasubramanian D. Simple limbal epithelial transplantation (SLET): a novel surgical technique for the treatment of unilateral limbal stem cell deficiency. Br J Ophthalmol. 2012;96(7):931-4.
8. Moshirfar M, Thomson AC, Ronquillo Y. Limbal Epithelial Transplant. [Updated 2023 Jul 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560557/
9. Kenyon KR, Tseng SC. Limbal autograft transplantation for ocular surface disorders. Ophthalmology. 1989;96:709e22.
10. Daya SM, Ilari FA. Living related conjunctival limbal allograft for the treatment of stem cell deficiency. Ophthalmology. 2001;108:126-33.
11. Pellegrini G, Traverso CE, Franzi AT, et al. Long-term restoration of damaged corneal surfaces with autologous cultivated corneal epithelium. Lancet. 1997;349:990e3.



