





SMILE with the VisuMax (Carl Zeiss Meditec) is gaining popularity as a laser vision correction technique. Despite the procedure’s high accuracy, some cases require additional refractive enhancement. As the technique gains wider acceptance, the need for such enhancements is likely to increase as well.
In Europe, Circle software (Carl Zeiss Meditec) enables the conversion of a SMILE cap into a LASIK flap and provides four distinct patterns for this purpose (Figure 1). This software is not yet available in the United States. In the United States, prevalent methods for enhancing SMILE include PRK; thick-flap LASIK, which incorporates the SMILE plane; and thin-flap LASIK, which is performed above the SMILE plane. Each of these techniques, although effective, presents its own set of limitations (see the accompanying sidebar).
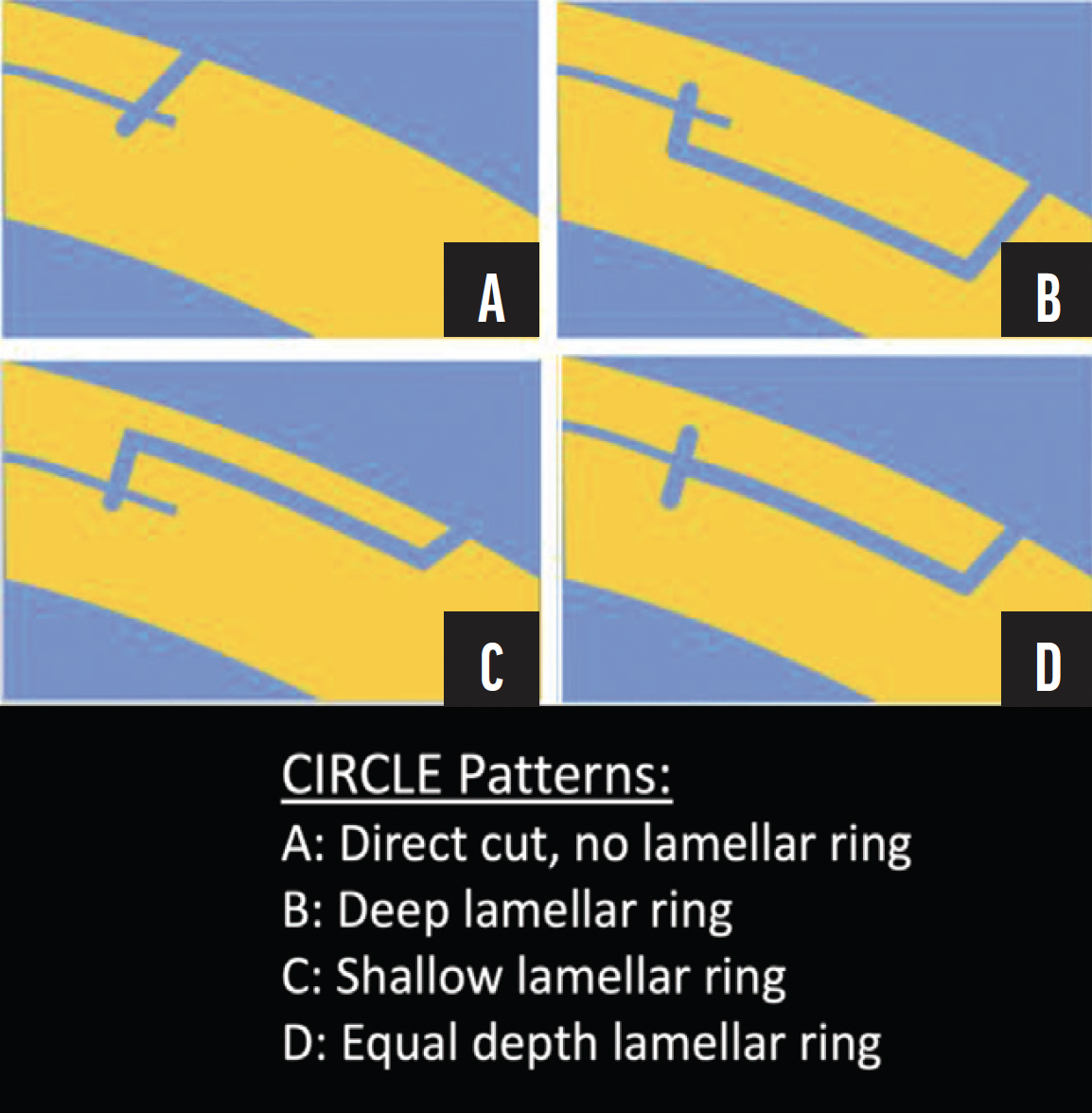
Figure 1. Circle software patterns for cap-to-flap enhancement with the VisuMax.
Source: Chansue E, Tanehsakdi M, Swasdibutra S, McAlinden C. Safety and efficacy of VisuMax® circle patterns for flap creation and enhancement following small incision lenticule extraction. Eye Vis (Lond). 2015;2:21. Figure 2. Licensed under [CC BY 4.0](http://creativecommons.org/licenses/by/4.0/).
In our practice, in the United States, SMILE has accounted for 61% of all laser vision correction procedures in the year 2022. In the absence of Circle software, we have adopted the cap-to-flap or pseudo-Circle technique as our primary strategy for SMILE enhancement (watch a video of the technique below). This approach is considered off-label in the United States.
CAP-TO-FLAP ENHANCEMENT STRATEGY
There are two primary approaches to cap-to-flap enhancement. The first approach involves creating a LASIK flap with a 7-mm diameter, detailed by John F. Doane, MD, in the accompanying video (watch below). This technique involves a small-diameter side cut that joins the sub-cap plane. Although effective, this method demands precise centration and may be associated with increased aberrations and an insufficient bed size for hyperopic and astigmatic enhancements.
Our preferred cap-to-flap technique involves the creation of a large-diameter LASIK flap, requiring the formation of a lamellar ring that intersects with the primary lenticule or sub-cap plane. Once this intersection is established, the treatment is temporarily paused. To prepare for what we term the ghost treatment, either the suction hose is kinked, or the suction port is manually occluded. The laser is not docked on the cornea during this phase, hence the name. Suction is then reactivated, and treatment resumes. The treatment is paused again with 4 to 5 seconds remaining, just before the side cut is completed. The cornea is recentered and redocked, followed by the final seconds of treatment to complete the side cut. This newly created LASIK flap can then be lifted using standard techniques.
One notable difference between the cap-to-flap technique and the Circle software is the absence of the vertical junction cut. This is the vertical, intrastromal portion designed to ensure seamless communication between the SMILE cap and the LASIK flap. Although this absence may result in slightly incongruous planes and tissue slivers, these can be carefully managed during the procedure and have not proven to be visually significant in our experience (watch a related video below).
We have employed this technique for several years with excellent results. We conducted a retrospective analysis of enhancement data over the past 3 years, enabling comparison of outcomes among various enhancement methods, including cap-to-flap, relift, PRK-enhanced LASIK, and PRK-enhanced SMILE.1
OPTIONS FOR SMILE ENHANCEMENT
THICK-FLAP LASIK
- Visual recovery. Rapid
- Flap thickness. Greater than 120 µm (inclusive of SMILE plane)
- Biomechanical impact. Significant, with a consequential reduction in residual stromal bed
- Optical zone interface. Dual femtosecond laser interface across the central optical zone
THIN-FLAP LASIK
- Visual recovery. Rapid
- Flap thickness. Less than 120 µm (above SMILE plane)
- Flap characteristics. Thinner and more friable
- Optical zone interface. Dual femtosecond laser interface, which may predispose the eye to inadvertent plane communication after excimer laser ablation. This can result in a central hole (in cases of myopic enhancement) or a free stromal wafer (in cases of hyperopic enhancement)
PRK
- Visual recovery. Slower
- Procedure. Surface ablation of SMILE cap
- Efficacy. Effective but with potential for unpredictable epithelial healing and an elevated risk of patient discomfort
RE-SMILE
- Technique. Specialized yet challenging, involving sub-cap lenticule extraction that utilizes the existing SMILE interface
- Research status. Requires further investigation for protocol standardization
CAP-TO-FLAP
- Visual recovery. Rapid
- Procedure. Conversion of the SMILE cap into a LASIK flap; the previous SMILE plane becomes the new LASIK bed
- Biomechanical impact. Reduced compared to thick-flap LASIK
- Optical zone interface. Single femtosecond laser interface, allowing for intentional and precise communication of interfaces, thus mitigating the risks associated with thin-flap LASIK
REFRACTIVE OUTCOMES
The study included patients who had previously undergone myopic LASIK or SMILE and later required enhancement. Its aim was to evaluate the cap-to-flap technique’s efficacy in addressing residual refractive errors following myopic SMILE. The study spanned the years 2020 to 2022 and employed various statistical tests to compare pre- and postoperative variables across different enhancement groups (detailed in the sidebar).
Key findings. The study found that the cap-to-flap technique achieved superior UCVA compared to flap relift, particularly in the 1- to 2-week postoperative period. These differences, however, were not statistically significant at 1 day and 1 to 3 months (Figure 2). Cap-to-flap consistently outperformed PRK-enhanced LASIK and PRK-enhanced SMILE across all measured time points.

Figure 2. Patients' UCVA on postoperative day 1 (A), weeks 1 to 2 (B), and months 1 to 3 (C).
In terms of postoperative refraction, cap-to-flap demonstrated superior outcomes in terms of both sphere and absolute mean refractive spherical equivalent (MRSE). The difference in Cylinder between groups was not statistically significant (Figure 3). All patients in the cap-to-flap group achieved an absolute MRSE of 0.25 D or less.
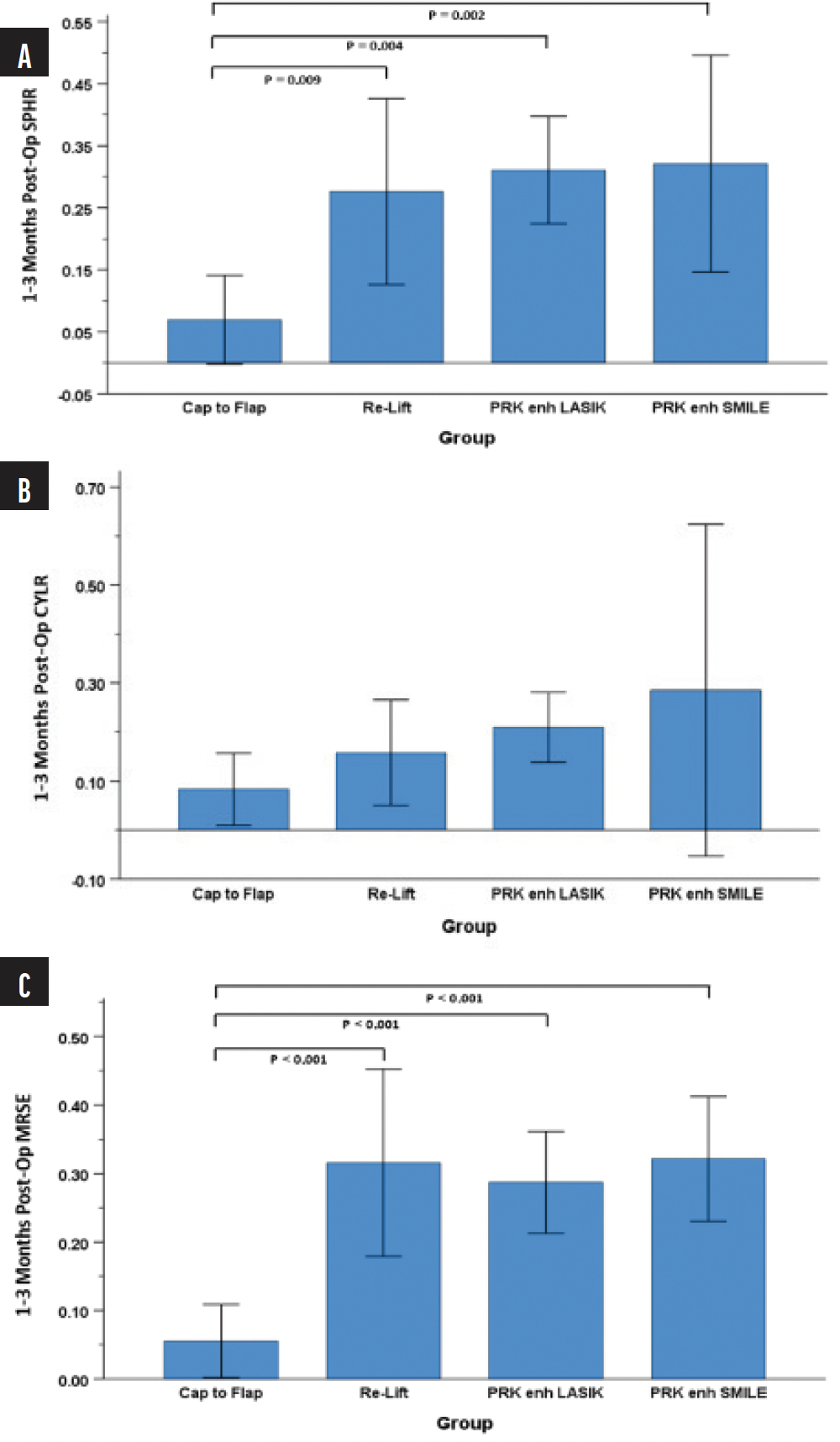
Figure 3. Mean absolute sphere (A), cylinder (B), and MRSE (C) at the 1- to 3-month postoperative interval.
Practical implications. The cap-to-flap technique stood out as a highly effective option for SMILE enhancement. It not only offered superior visual outcomes but also promised a quicker and more predictable recovery. For these reasons, it has become our go-to method for SMILE enhancement.
ADDITIONAL INSIGHTS
Cap-to-flap is a reliable and effective method of SMILE enhancement. It is associated with a lower risk of epithelial ingrowth than other methods of SMILE enhancement, and its performance and safety profile closely align with those of primary LASIK.
1. DeCourcey M, MD; Wiley WF, MD, ABO; Bafna S, MD; Jee KJ, MD; Hura A, MD; Augustine JM, OD. Analysis of Refractive Outcomes in SMILE Converted to LASIK (“Cap to Flap”) Enhancements. Paper presented at: 2023 ASCRS Annual Meeting; May 5-8, 2023; San Diego, CA.




