The first time I walked as a freshman deep into the stacks of my university’s library, I was struck by the thought of how much I didn’t know. It is a thought that has recurred to me many times since, and it can be humbling. The intellectually curious side of me, however, embraces that there is always so much more for people of any age to learn. That truth is certainly evident in the ophthalmic literature.
This article highlights nine studies that caught my attention this year, but there’s more. Just as Ringo Starr gets by with a little help from his friends, I am fortunate that several editorial board members of CRST and CRST Europe accepted my invitation to share their thoughts on important research published in 2019. I hope you enjoy catching up on some of this year’s scientific highlights.
CATARACT SURGERY
Grzybowski et al analyzed the peer-reviewed literature to determine if a follow-up visit 1 day after cataract surgery is necessary. They concluded that this visit could be eliminated after uneventful surgery by experienced ophthalmologists when the patient has no risk factors such as posterior synechiae or chronic or recurrent uveitis. If this visit is eliminated, the researchers recommended prescribing a potent postoperative topical steroid, and they suggested that administering a combination of IOP-lowering medications after cataract surgery might be advisable in patients with glaucoma.1 If follow-up visits on postoperative day 1 could be safely eliminated for a sizable proportion of the patient population, the health care cost savings could be significant.


Lisa Brothers Arbisser, MD; and John A. Hovanesian, MD
Haripriya A, Chang DF, Ravindran RD. Endophthalmitis reduction with intracameral moxifloxacin in eyes with and without surgical complications: results from 2 million consecutive cataract surgeries. J Cataract Refract Surg. 2019;45(9):1226-1233.
Although it is a clinical retrospective study, it unarguably should suffice to change the practice of all cataract surgeons. I have used intracameral moxifloxacin routinely since 2007, but a very small percentage of US ophthalmologists have adopted this important practice, which can decrease vision-threatening endophthalmitis up to sevenfold. This big data article is so convincing I don’t think any prospective multicenter trial—which will be a long time coming—could be significantly more valid. Would that the FDA could approve the $1 Aurolab version (good for several cases) or that the profession would demand another cost-effective version of intracameral moxifloxacin.—L.B.A.
This study examined a staggering 2 million patients operated on at the Aravind network of hospitals in India. The article shows the value of intracameral antibiotics for preventing endophthalmitis after cataract surgery. The benefit of this drug was particularly notable in patients with ruptured posterior capsules. This article underscores the conflict in the United States between practicing good medicine and following FDA regulations.—J.A.H.
MYOPIA
In 2010, an estimated 27% of the world’s population was myopic, and 2.8% of them had high myopia. Those figures are expected to increase dramatically by 2050. Myopia is also the leading cause of visual impairment in children.2 It is therefore no surprise that public health officials, physicians, academicians, and members of industry are working hard to understand and address the problem.

P. Dee G. Stephenson, MD, FACS
Tyson SL, Bafna S, Gira JP, et al; Dextenza Study Group. Multicenter randomized phase 3 study of a sustained-release intracanalicular dexamethasone insert for treatment of ocular inflammation and pain after cataract surgery. J Cataract Refract Surg. 2019;45(2):204-212.
This large, well-designed study evaluated a novel mechanism of steroid delivery that removes the issues of compliance and self-administration of the most complex postoperative topical eye drop. This study also included pooled data from all three phase 3 trials, giving a sense of the safety and efficacy of this sustained-release intracanalicular dexamethasone insert (Dextenza, Ocular Therapeutix). I can get excited about any research focused on innovative technology that puts control back in the hands of surgeons.
The use of atropine has been a major area of research. In January, investigators published the results of the Low-Concentration Atropine for Myopia Progression (LAMP) study. This randomized, double-masked, placebo-controlled trial evaluated the safety and efficacy of 0.05%, 0.025%, and 0.01% atropine eye drops to control myopia. All concentrations were well tolerated, and they reduced myopia progression with a concentration-dependent response.3

Arthur B. Cummings, MB ChB, FCS(SA), MMed(Ophth), FRCS(Edin)
Zheleznyak L, Butler SC, Cox IG, et al. First-in-human laser-induced refractive index change (LIRIC) treatment of the cornea. Invest Ophthalmol Vis Sci. 2019;60(9):5079.
This is possibly a new paradigm in corneal, contact lens, and IOL optics without shape change or thickness changes. The potential is enormous in my opinion.
Fan L, Xiong L, Zhang B, Wang Z. Longitudinal and regional non-uniform remodeling of corneal epithelium after topography-guided FS-LASIK. J Refract Surg. 2019;35(2):88-95.
Corneal epithelial maps are now an integral part of a keratorefractive surgery workup. This article demonstrates how uniform the epithelium is after topography-guided laser vision correction, resulting in a smooth stromal contour, and hence, minimal epithelial masking is required.
In April, the AAO reported that orthokeratology may be effective at slowing myopia progression in children and adolescents and that the effect may be greater when treatment is initiated in children who are 6 to 8 years of age. Safety, of course, remains a major concern because overnight contact lens wear has been associated with potentially blinding microbial keratitis.4
As research in this area continues, more will be revealed about the roles of environmental factors and potential treatments for slowing or halting the progression of myopia. Already some physicians have begun using a new calculator for monitoring myopia in their patients that is available from the Brien Holden Vision Institute in Australia (bit.ly/33rx4Xp).

Richard Tipperman, MD
Astigmatic correction with implantation of a light adjustable vs monofocal lens: a single site analysis of a randomized controlled trial. Int J Ophthalmol. 2019;12(7):1101-1107.
Being able to target exact postoperative refractions would be a game-changer for ophthalmology. This study focuses on the Light Adjustable Lens (RxLAL, RxSight), but I am even more excited about the Perfect Lens system under investigation, which uses a femtosecond laser to adjust the refractive index of an acrylic IOL in vivo.
EPIDEMIOLOGY
The Chinese American Eye Study included 4,582 patients who were 50 years of age or older. Researchers sought to identify risk factors for vision impairment in this population and found that age and a self-reported history of ocular disease were most strongly associated with vision loss. Limited education, low acculturation, and a self-reported history of diabetes were additional risk factors.5 The results of this study could facilitate the development of targeted screening and educational programs to reduce the burden of vision impairment in this population.

Jorge L. Alió,MD, PhD, FEBOphth
Wang L, Spektor T, de Souza RG, Koch DD. Evaluation of total keratometry and its accuracy for intraocular lens power calculation in eyes after corneal refractive surgery. J Cataract Refract Surg. 2019;45(10):1416-1421.
This study showed that standard formulas such as the Haigis, when the total keratometry value is included, are comparable to more advanced formulas like the Barrett True-K for IOL power calculations in eyes that previously underwent corneal refractive surgery. Using the total keratometry value of the anterior corneal surface obtained from a universal device such as the IOLMaster (Carl Zeiss Meditec) improves the accuracy of the Haigis formula in these difficult cases.
Sánchez-González JM, López-Izquierdo I, Gargallo-Martínez B, De-Hita-Cantalejo C, Bautista-Llamas MJ. Bandage contact lens use after photorefractive keratectomy. J Cataract Refract Surg. 2019;45(8):1183-1190.
Postoperative pain is the main factor limiting the use of PRK. In this study, a specific type of contact lens material, senofilcon A, was associated with lower pain scores and faster re-epithelialization. This meta-analysis and systematic review offer an important pearl to refractive surgeons about which lens to use to promote recovery after PRK.
GLAUCOMA
Research into and the development of microinvasive glaucoma surgery (MIGS) continue at a rapid pace, and the HORIZON Study was an important addition to the literature in 2019. This prospective, multicenter, single-masked, randomized controlled trial (RCT) compared outcomes at 2 years in eyes that received the Hydrus Microstent (Ivantis) at the time of cataract surgery to those of eyes that underwent cataract surgery alone. Also noteworthy was the size of this RCT of a MIGS device (> 550 eyes) and its incorporation of a medication washout, which allowed investigators to make a direct determination of the amount of IOP reduction that could be attributed to the MIGS device alone.6
Published in 2012, the SLT/Med Study compared the outcomes of selective laser trabeculoplasty (SLT) to those of medical therapy in patients with open-angle glaucoma (OAG) or ocular hypertension (OHT). The researchers found that both groups had achieved a similar decrease in IOP after 1 year but that more treatment steps were required to maintain the target IOP in the medication group.7 Although this prospective RCT provided evidence supporting SLT as a safe and effective option for initial therapy for patients with OAG or OHT, medication remains the conventional first line of treatment for patients newly diagnosed with OAG or OHT, and SLT is rarely used as primary therapy for these individuals. Will a publication by the investigators for the Laser in Glaucoma and Ocular Hypertension (LiGHT) Trial this year change the status quo? This hospital-based prospective RCT compared SLT and medical therapy in terms of health-related quality of life, cost, cost-effectiveness, clinical effectiveness, and safety. Based on the results, the researchers argued that SLT should be offered as first-line treatment for patients with OAG or OHT.8

Noel Alpins,AM, FRANZCO, FRCOphth, FACS
Wallerstein A, Gauvin M, Qi SR, Bashour M, Cohen M. Primary topography-guided LASIK: treating manifest refractive astigmatism versus topography-measured anterior corneal astigmatism. J Refract Surg. 2019;35(1):15-23.
This is an insightful examination of the topographically driven paradigms of laser vision correction. The investigators found that the outcomes of topography-modified refraction, commonly referred to as TMR, were inferior to those of the control group when larger axis differences were present. As a result, the study was terminated after 369 eyes had been treated on the anterior corneal axis instead of the refractive axis (control group, 905 eyes).
Complementing this research was the Steroids After Laser Trabeculoplasty (SALT) Trial. In this double-masked, randomized, placebo-controlled, dual-center, multisurgeon study, investigators sought to determine whether the short-term use of topical NSAID or steroid therapy affected the efficacy of SLT. The results indicate it did. At 12 weeks, the reduction in IOP was statistically significantly greater in eyes that were treated with topical steroid or NSAID drops.9

Soosan Jacob,MS, FRCS, DNB
Jarade E, Issa M, Chanbour W, Warhekar P. Biologic stromal ring to manage stromal melting after intrastromal corneal ring segment implantation. J Cataract Refract Surg. 2019;45(9):1222-1225.
This study by Jarade et al and my work with colleagues1 on corneal allogenic intrastromal ring segments are showing that switching to biologic tissue is a viable method for avoiding and, if required, treating various complications associated with synthetic intrastromal corneal ring segments, including corneal melt, necrosis, infection, migration, extrusion, intrusion, and neovascularization (Figure).
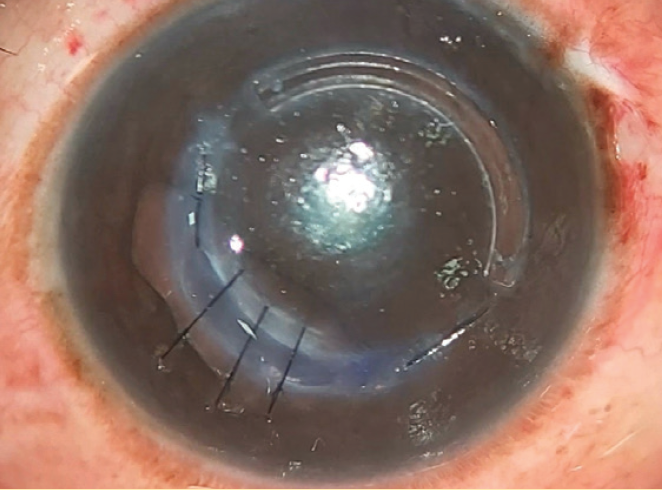
Figure. Dr. Jacob replaced a synthetic intrastromal corneal ring segment with a corneal allogenic intrastromal ring segment.
1. Jacob S, Patel SR, Agarwal A, Ramalingam A, Saijimol AI, Raj JM. Corneal allogenic intrastromal ring segments (CAIRS) combined with corneal cross-linking for keratoconus. J Refract Surg. 2018;34(5):296-303.
CORNEAL AND REFRACTIVE SURGERY
The results of a small retrospective study suggested that combining transepithelial phototherapeutic keratectomy and CXL may be an effective long-term treatment strategy for patients with pellucid marginal degeneration. Investigators evaluated patients’ visual acuities, refractions, topographic keratometry readings, pachymetry readings, and aberrations for 3 years after treatment.10
As screening methods and diagnostic technologies continue to advance, corneal and refractive surgeons are becoming increasingly adept at diagnosing PMD. New options for treating a therefore growing pool of patients with PMD would be welcome.

William I. Bond, MD
Hogarty DT, Hogarty JP, Hewitt AW. Smartphone use in ophthalmology: what is their place in clinical practice [published online ahead of print September 18, 2019]? Surv Ophthalmol. doi:10.1016/j.survophthal.2019.09.001.
This is an article of much relevance to ophthalmology practices. It clearly discusses offices’ use of apps for patient care. The use of physician extenders in an ethical and patient-centered manner is a crucial topic in a challenging economic time.
HEALTH CARE
Investigators reported evidence of racial bias in a commercial algorithm that is widely used by the US health care system to identify and assist patients with complex health needs. The researchers stated that bias was introduced because the algorithm uses the cost of health care as a proxy for the need for health care. They found that health care spending was less for black patients than for white patients with similar medical conditions, leading the algorithm to the false conclusion that the black patients were healthier than the white patients.11
As the use of big data grows in medicine generally and in ophthalmology specifically, it will become increasingly important to ensure that the algorithms developed are reducing rather than increasing health care disparities and improving rather than worsening patients’ access to health care.
1. Grzybowski A, Kanclerz P. Do we need day-1 postoperative follow-up after cataract surgery? Graefes Arch Clin Exp Ophthalmol. 2019;257(5):855-861.
2. Fricke TR, Jong M, Naidoo KS, et al. Global prevalence of visual impairment associated with myopic macular degeneration and temporal trends from 2000 through 2050: systematic review, meta-analysis and modelling. Br J Ophthalmol. 2018;102(7):855-862.
3. Yam JC, Jiang Y, Tang SM, et al. Low-Concentration Atropine for Myopia Progression (LAMP) Study: a randomized, double-blinded, placebo-controlled trial of 0.05%, 0.025%, and 0.01% atropine eye drops in myopia control. Ophthalmology. 2019;126(1):113-124.
4. VanderVeen DK, Kraker RT, Pineles SL, et al. Use of orthokeratology for the prevention of myopic progression in children: a report by the American Academy of Ophthalmology. Ophthalmology. 2019;126(4):623-636.
5. Burkemper B, Torres M, Jiang M, McKean-Cowdin R, Varma R. Factors associated with visual impairment in Chinese American adults: The Chinese American Eye Study. Ophthalmic Epidemiol. 2019;26(5):329-335.
6. Samuelson TW, Chang DF, Marquis R, et al; HORIZON Investigators. A Schlemm canal microstent for intraocular pressure reduction in primary open-angle glaucoma and cataract: The HORIZON Study. Ophthalmology. 2019;126(1):29-37.
7. Katz LJ, Steinmann WC, Kabir A, Molineaux J, Wizov SS, Marcellino G; SLT/Med Study Group. Selective laser trabeculoplasty versus medical therapy as initial treatment of glaucoma: a prospective, randomized trial. J Glaucoma. 2012;21(7):460-468.
8. Gazzard G, Konstantakopoulou E, Garway-Heath D, et al; LiGHT Trial Study Group. Selective laser trabeculoplasty versus eye drops for the first-line treatment of ocular hypertension and glaucoma (LiGHT): a multicentre randomised controlled trial. Lancet. 2019;393(10180):1505-1516.
9. Groth SL, Albeiruti E, Nunez M, et al. SALT Trial: steroids after laser trabeculoplasty: impact of short-term anti-inflammatory treatment on selective laser trabeculoplasty efficacy. Ophthalmology. 2019;126(11):1511-1516.
10. Cagil N, Sarac O, Yesilirmak N, Caglayan M, Uysal BS, Tanriverdi B. Transepithelial phototherapeutic keratectomy followed by corneal collagen crosslinking for the treatment of pellucid marginal degeneration: long-term results. Cornea. 2019;38(8):980-985.
11. Obermeyer Z, Powers B, Vogeli C, Mullainathan S. Dissecting racial bias in an algorithm used to manage the health of populations. Science. 2019;366(6464):447-453.