Fluidics technologies for cataract surgery are always improving to better meet the primary goals of chamber stability and consistency. I’ve recently begun using some new components of the CENTURION Vision System (Alcon), including the ACTIVE SENTRY Handpiece (Alcon), which has a built-in pressure sensor that allows it to work with the system’s ACTIVE FLUIDICS technology (Alcon), enhancing stability automatically throughout surgery. Also improving the safety of surgery is the new INTREPID Hybrid Tip (Alcon), which breaks up even dense nuclei and helps reduce the risk of capsular tears.
Employing Automated Pressure Control
When I began using the ACTIVE SENTRY Handpiece, I thought I would feel something different during the procedure. Instead, I found that the technology senses intraocular pressure (IOP), triggers precise adjustments to the fluidics, and maintains the target IOP throughout surgery without any noticeable difference to my surgical experience. I’m performing cataract surgery as I have always done, reaping the benefits of ACTIVE SENTRY without making any adjustments to my procedure.
Occasionally, I can detect where there has been a postocclusion surge event when ACTIVE SENTRY would trigger an adjustment, but it’s rare. After surgery, the system displays the number of times that the sensor triggered a change, which could be anywhere from 0 to possibly as high as 15 or more.
The standout benefit of surge mitigation is that it makes my procedures safer. It ensures that the anterior chamber is more stable with less IOP fluctuation and less change in fluid volume during surgery. With the ACTIVE SENTRY Handpiece, I get the advantages of a safer procedure without the need to change my approach.
The only significant change I’ve made to my procedure was to lower my IOP to a much more physiologic level. Because I like higher vacuum levels, I’ve always needed a higher IOP to maintain chamber stability. But with the ACTIVE SENTRY Handpiece, I’ve noticed the chamber is stable even in those postocclusion surge events, and therefore I’ve been able to lower my target IOP during surgery. In past cases where I would set a target IOP of 75 mm Hg to maintain a consistent fluid volume in the eye at high vacuum levels, I now set a target IOP of 55 to 60 mm Hg and still maintain the same chamber stability. As I gain experience, perhaps my IOP will drift lower.
The Added Safety of Polymer Hybrid Tips
Further adding to the safety of my cataract procedures, I have begun using the INTREPID Hybrid Tip with the ACTIVE SENTRY Handpiece. The polymer construction ensures that no metal comes in contact with the capsular bag, thus reducing the risk of tears. The first time I used a Hybrid Tip, I thought it would not penetrate dense nuclei as well as a metal tip, but I was very impressed with its ability to penetrate. Now I’m comfortable using a Hybrid Tip on virtually all nuclei except the densest ones.
Surgery with the Hybrid Tip is the same as standard tips, so the transition is completely seamless. In all of my standard cases up to 3+ nuclei, I don’t feel there is any difference in the time required compared to standard CENTURION Vision System settings and tips. I’d say that, in cases with dense nuclei, the ACTIVE SENTRY Handpiece and Hybrid Tip slightly increase the time to perform the procedure, but I feel the better safety profile of these two technologies outweighs any slight decrease in efficiency. With denser nuclei, we are more likely to encounter complications, and I’m happy to take a few extra seconds to avoid them.
The Right Technologies for Complex Cases
As I mentioned, I use the ACTIVE SENTRY Handpiece and Hybrid Tip for just about all of my cases. In addition, there are several complex cases where I feel the abilities of these two technologies to maintain a stable chamber and protect the capsular bag are particularly beneficial.
First, when patients have a floppy iris or a small pupil with more potential volatility, a stable chamber makes the iris less floppy and reduces the likelihood that the pupil will continue to constrict during the procedure. I am also less likely to damage the iris with the Hybrid Tip during those procedures.
Second, in cases with extremely dense nuclei, we tend to get more occlusion with a greater potential for postocclusion surge. Those cases take longer as we spend more time in quadrant removal compared to standard cases. And the more time we spend performing quadrant removal, the more likely we are to encounter complications such as posterior capsule rupture. By making postocclusion surge less significant, ACTIVE SENTRY can improve safety in these cases.
Finally, in postfemtosecond laser cases where the nucleus has been softened significantly, there is potential for significant fluctuations in the anterior chamber. The nuclei tend to be softer, so I’m able to vacuum them while using little ultrasound. As the vacuum builds, without a lot of ultrasound, there is greater opportunity for postocclusion surge, and the ACTIVE SENTRY controls those surges.
Added Safety Is Paramount
The ACTIVE SENTRY Handpiece increases the safety of cataract procedures by mitigating postocclusion surge events. The pressure sensors in the ACTIVE SENTRY Handpiece enable the system to respond to the drop in IOP much faster than sensors in the machine, triggering an adjustment in the volume of fluid in the anterior chamber. As a result, my patients’ IOP does not drop as significantly during the phacoemulsification portion of the procedure.
I compare the combination of ACTIVE SENTRY and ACTIVE FLUIDICS technology to the automatic braking systems available in cars today. When the vehicle detects an obstacle or disruptive event in its surroundings, such as a truck stopping short in front of you, the automatic braking technology responds faster than you could to stop your car before a collision occurs.
That’s the ACTIVE SENTRY role. It detects surge events and rapidly mitigates them by changing the intraocular environment. It helps to prevent a more disruptive event that might occur if I needed to react and make the adjustment. When we add the advantages of using the Hybrid Tip’s rounded polymer edge for effective sculpting and quadrant removal that protects intraocular tissues, the CENTURION has made major strides in advancing the safety of cataract surgery.
Case: Femtosecond Capsulotomy and Toric Lens Implantation
A 74-year-old patient with a 2+ to 3+ cataract was scheduled for cataract surgery and implantation of a toric lens. After the patient underwent both a capsulotomy and lens fragmentation with the LenSx femtosecond laser (Alcon), I made laser incisions all the way out at the limbus and was able to open them very easily. At that point, we had a free-floating capsulotomy.
Removing the nucleus with ACTIVE SENTRY and the INTREPID Hybrid Tip: I used the INTREPID Hybrid Tip with the rounded polymer tip that protects the posterior and anterior capsules. I began sculpting, removed a lot of the nucleus with very little ultrasound—which is our goal when we’ve done a laser procedure—and presoftened the nucleus. The tip allowed me to manipulate and rotate the nucleus during the procedure very efficiently, and it moved smoothly through the almost 3+ nucleus (Figure 1).
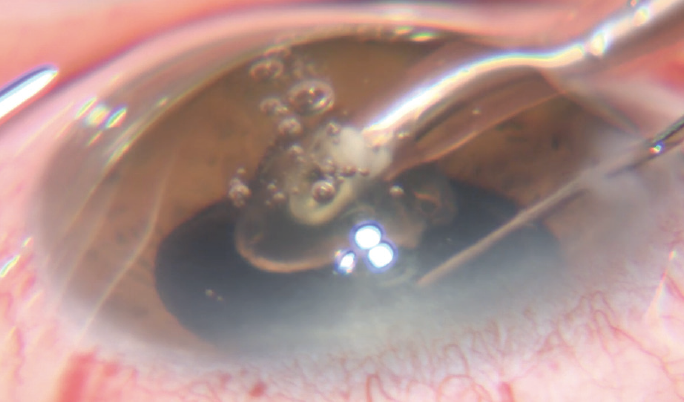
Figure 1. The rounded polymer INTREPID Hybrid Tip moved smoothly through the almost 3+ nucleus, making removal easy with very little ultrasound while protecting the capsule. The new ACTIVE SENTRY Handpiece allowed me to use the highest vacuum settings while maintaining an IOP of about 60 mm Hg.
I began quadrant removal using very little ultrasound as I vacuumed each quadrant. I applied ultrasound when necessary, but what I love about CENTURION Vision System and ACTIVE FLUIDICS, along with the new ACTIVE SENTRY Handpiece, is that I can utilize a higher vacuum than I did with prior technologies, yet still maintain a very stable anterior chamber. It allows me to perform more of the procedure under aspiration and less under phaco.
High vacuum, IOP consistent at 60 mm Hg: While removing the quadrants during this procedure, my vacuum setting was 700+, which is the maximum on the machine, but the anterior chamber remained very stable. The sensor in the ACTIVE SENTRY Handpiece quickly detected the postocclusion surge, instantly triggering mitigation through ACTIVE FLUIDICS. While removing the last quadrant, I saw hardly any movement in the iris or the posterior capsule, even with a vacuum of 700.
Looking at the metrics from this case, I saw that the ACTIVE SENTRY Handpiece had a total of 10 actuations. That represents the number of times that the handpiece detected a postocclusion surge event and made adjustments to ensure that there was minimal fluid loss and the chamber remained stable. The CDE was only 0.93 for an almost 3+ nucleus density.
Cortex removal and polishing with a polymer I/A tip: Next, I moved to the polymer I/A tip, which also has the same polymer material as the Hybrid Tip for better safety design. This I/A tip makes cataract surgery a complete polymer-tip procedure, so there are no sharp, metallic objects in the eye at any point during surgery from the phaco machine perspective.
The I/A tip comes in both rounded and angled profiles. Using the curved polymer I/A tip, which I really like for laser cases, I removed the peripheral cortex and even some of the subincisional cortex without difficulty in a consistent, controlled manner (Figure 2). I had no worries about sharp, metallic instruments in the eye that could harm the capsule. As I polished the posterior capsule very gently with the curved I/A tip, I was able to remove all the material quite easily.
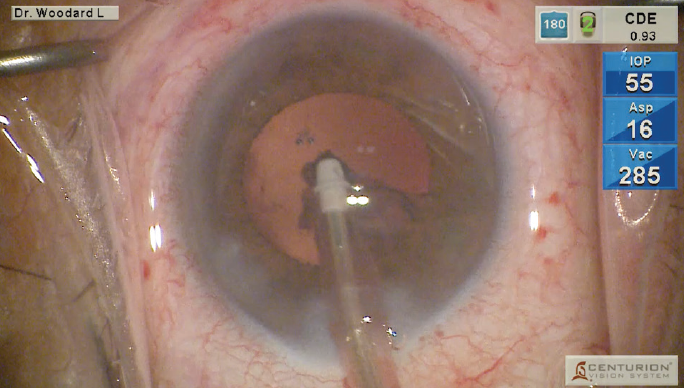
Figure 2. Using the curved polymer I/A tip, I removed the peripheral cortex and some of the subincisional cortex without difficulty in a consistent, controlled manner and very gently polished the posterior capsule.
Implanting the toric lens: Because this was a toric case, I filled the eye with sodium hyaluronate (PROVISC; Alcon) in preparation for taking ORA SYSTEM (Alcon) technology measurements. I like to fill the eye until I see viscoelastic coming out of the incision, because that usually indicates that we have adequate IOP. I used a Barraquer tonometer to confirm that the patient’s IOP was in the correct range (55 to 60).
Using the ORA SYSTEM measurements, I selected the 20.0 diopter lens. The options were the SN6AT4 (Alcon) lens, which would leave us with approximately 0.1 diopters of against-the-rule astigmatism, or the SN6AT5 (Alcon), which would leave us with almost 0.4 diopters of with-the-rule astigmatism. I could either flip the axis and leave the patient almost 0.4 diopters or leave him with 0.1 diopters in the same axis. Generally, I like to leave the least residual astigmatism possible, so I selected the SN6AT4 in this case to leave the patient with only 0.1 diopters of residual astigmatism on his current axis.
I placed the IOL using the AutoSert device, which allows me to deliver the IOL into the eye in an automated manner using the flip pedal on the CENTURION machine. I can use a one-handed technique, holding the eye stable with the other hand as I insert the lens. It utilizes the same D-cartridge that I would ordinarily use and delivers it into the eye in a very controlled manner.
NRR (no rotation recommended) appeared on the ORA machine, so I anticipated that the lens would deliver exactly what we were expecting. Getting NRR with minimal residual astigmatism gives me a lot of confidence in the IOL selection and placement on the correct axis to deliver the expected outcomes. Finally, I removed the residual viscoelastic. The case was very successful, relying on the latest technologies to ensure the patient had excellent visual outcomes.




