

The preoperative examination of patients scheduled for corneal cross-linking (CXL) is extremely important, because the data points generated (eg, refraction, UCVA, BCVA, topography/tomography) are used for comparison at every future examination. With this in mind, it is worth taking a closer look at how to maximize the accuracy of baseline readings.
PREVALENCE OF KERATOCONUS
Keratoconus is an asymmetric, bilateral, frequently progressive corneal disease, and it is more common than eye care providers once thought. In 1998, Rabinowitz reported a disease prevalence of approximately 1:2,000.1 More recent data suggest an even higher incidence of keratoconus.
AT A GLANCE
- Keratoconus is an asymmetric, bilateral, frequently progressive corneal disease, and it is more common than eye care providers once thought.
- The preoperative examination of patients scheduled for corneal cross-linking is extremely important, because the data points generated are used as a point of comparison for every future examination.
Godefrooij and colleagues performed an epidemiological study based on a total of 4.4 million patients from the Netherlands.2 The investigators determined that the annual incidence of keratoconus was 1:7,500 in the relevant age category (13.3 cases per 100,000; 95% confidence interval [CI], 11.6-15.2) and the estimated prevalence of keratoconus in the general population was 1:375 (265 cases per 100,000; 95% CI, 260-270). These values are five- to tenfold higher than previously reported in population studies. Patients’ mean age at diagnosis was 28.3 years, and 60.6% of the individuals diagnosed were male.
Why the uptick in prevalence and incidence over the past 40 years? Technology! Early on, keratoconus screening involved only retinoscopes, keratometers, and rudimentary Placido disk imagers. Today, clinicians have access to more advanced and sensitive diagnostic equipment that can image and analyze corneal elevation values not only of the anterior surface of the cornea but also of the posterior cornea. Devices with Scheimpflug cameras, optical coherence tomography (OCT), and high-frequency ultrasound can assess the cornea, allowing early detection of this all-too-common disease.
DIAGNOSTIC CHALLENGES
Although advanced keratoconus can produce slit-lamp findings such as corneal striae or apical scarring, the examination can appear completely normal in patients with early, mild, and sometimes even moderate disease. Moreover, many patients with early keratoconus have a normal central corneal thickness. The most effective way to make the diagnosis is to perform corneal imaging, typically topography, tomography, or both. Additional technologies can be used that are designed to measure the epithelial thickness profile; they include corneal OCT (RTVue-100 [Optovue] and Cirrus HD-OCT [Carl Zeiss Meditec]) and high-frequency ultrasound of the cornea (ArcScan Insight 100; ArcScan; Figure 1).
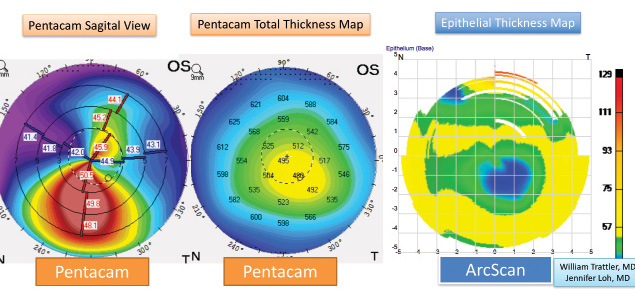
Figure 1. A patient with keratoconus on tomography exhibits inferior corneal steepening. High-frequency ultrasound using the ArcScan demonstrates epithelial thinning over the apex of the cone.
LENS WEAR
To resolve corneal warpage, patients should discontinue wearing their contact lenses prior to their preoperative evaluation. For scleral lenses and soft contact lenses, this “holiday” should be for 3 days, but a longer period will help ensure that the best images are captured on topography and tomography during the final preoperative exam. Patients who wear toric soft contact lenses are typically advised to take a holiday of a week, whereas patients with rigid gas permeable lenses should discontinue their use for 1 week per decade of wear.
Contact lens wear can increase patients’ risk of dry eye disease and blepharitis. Because ocular surface disease (OSD) can influence preoperative measurements, it is important for eye care providers to identify and treat preexisting dry eye disease and then bring patients back for their final preoperative visit prior to the CXL procedure (Figure 2).
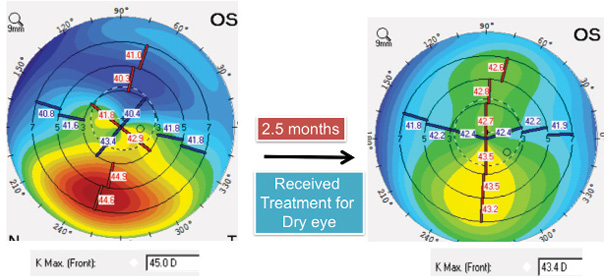
Figure 2. In this patient with OSD, an evaluation with the Pentacam (Oculus Optikgeräte) appears suspicious for keratoconus (left). After treatment of the OSD, imaging with the device is repeated, and the scan reveals only very early keratoconus in the patient’s left eye (right).
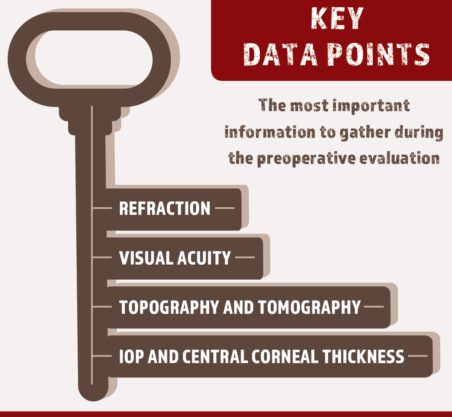
KEY DATA POINTS
During the preoperative exam, some of the most important data points to gather are
- visual acuity (corrected and uncorrected)
- refraction
- accurate topographic and tomographic measurements
- IOP and corneal thickness measurements
Patients would be expected to have stable or improved vision, refractions, and corneal shape at each visit occurring 3 months or longer after the CXL procedure. If there is a trend of worsening vision, and if there are findings of increased corneal steepening, the patient may require repeat CXL. The risk of needing a second CXL procedure is approximately 3%.3 (For more on managing patients with disease progression after CXL, see Dr. Hatch’s article).
CONCLUSION
The early diagnosis of keratoconus allows patients to undergo CXL before they suffer significant vision loss. CXL can also halt the progression of recurrent keratoconus in patients with corneal transplants and that associated with conditions such as pellucid marginal degeneration and post-LASIK ectasia.
The International Keratoconus Academy of Eye Care Professionals (www.keratoconusacademy.com) recommends that clinicians use modern technology such as Scheimpflug photography and OCT to identify patients with progressive corneal ectatic disease and subsequently treat appropriate candidates with CXL to halt progression as soon as possible. Happily, data from CXL studies have revealed that many patients who undergo the procedure can experience an improvement in UCVA and BCVA.4
The opinions in this article are the authors’ and not those of the US government.
1. Rabinowitz YS. Keratoconus. Surv Ophthalmol. 1998;42(4):297-319.
2. Godefrooij DA, de Wit GA, Uiterwaal CS, et al. Age-specific incidence and prevalence of keratoconus: a nationwide registration study. Am J Ophthalmol. 2017;175:169-172.
3. Antoun J, Slim E, El Hachem R, et al. Rate of corneal collagen crosslinking redo in private practice: risk factors and safety. J Ophthalmol. 2015;2015:690961.
4. Hersh PS, Stulting RD, Muller D, et al; United States Crosslinking Study Group. United States multicenter clinical trial of corneal collagen crosslinking for keratoconus treatment [published online ahead of print May 7, 2017]. Ophthalmology. doi:10.1016/j.ophtha.2017.03.052.




