The most critical step in laser cataract surgery, in my opinion, is the creation of the continuous capsulotomy. A well-made opening allows for accurate IOL centration relative to the pupil or scanned capsule; a repeatable effective lens position, given the uniform overlap of the capsule over the optic; and a reduced incidence of posterior capsular opacification.1 Software updates that increase laser speed and hardware upgrades like Alcon’s SoftFit patient interface have reduced the risk of an incomplete capsulotomy or tag to between zero and 3%,2,3 but the low incidence of the imperfect laser capsulotomy should not hide its importance. After all, patients undergoing laser cataract surgery are often also receiving a toric or presbyopia-correcting IOL. Their expectations are thus especially high. If an incomplete capsulotomy occurs, so does the risk of anterior capsular rents, posterior capsular tears, and vitreous loss. Mitigating these risks requires
• understanding how the laser works
• knowing what to pay attention to during docking, planning, and laser treatment to minimize the possibility that tags and discontinuities will occur
• having ways to deal with these problems once identified
LASER CAPSULOTOMY BASICS
The ASCRS Refractive Cataract Surgery Subcommittee published an excellent review of femtosecond lasers and differences between models.4 Briefly, each system uses either optical coherence tomography (OCT; LenSx Laser [Alcon], Catalys Precision Laser System [Abbott Medical Optics], and Victus [Bausch + Lomb]) or Scheimpflug imaging (Lensar Laser System [Lensar]) to create a 3-D reconstruction of the crystalline lens. The treatment plan is then overlaid, and you have the option to adjust gates that specify where the laser treatment will be applied.
AT A GLANCE
• The low incidence of the imperfect laser capsulotomy should not hide its importance. If the problem occurs, so does the risk of anterior capsular rents, posterior capsular tears, and vitreous loss.
• Routine system maintenance, special attention to alignment during docking, and the elimination of eye movements under suction all minimize the chance of encountering this complication.
• Successfully managing an incomplete capsulotomy starts with early recognition that it has occurred.
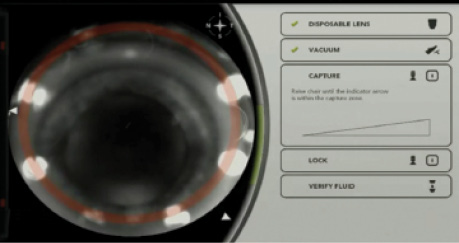
For the capsulotomy, these gates define a theoretical cylinder that is 400 to 700 µm in height and incorporates the anterior capsule (10-20 µm thick) and a safety margin to prevent tags and discontinuities. The application of a 4- to 6-µJ laser pulse causes plasma formation and produces a cavitation bubble that expands and mechanically disrupts the tissue. For the capsulotomy, spots are applied 4 to 6 µm apart in the x-y plane and 5 to 10 µm apart in the z-plane. All of this is important because the applied energy and spot spacing can be changed manually (Figure 1).
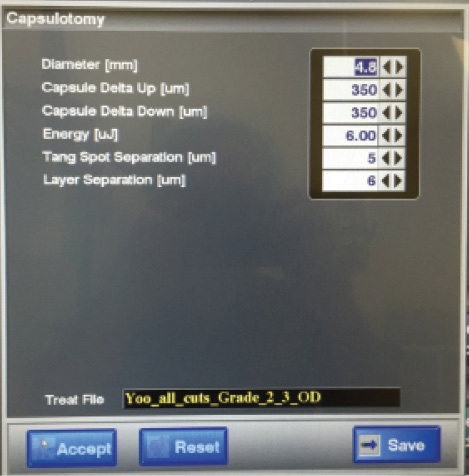
Figure 1. Capsulotomy advanced settings menu on the LenSx Laser. Energy, tangential spot separation, or layer separation values can be altered in specific situations, like hypermature cataracts, to increase the likelihood of a complete capsulotomy.
Although every laser from a single manufacturer is designed to be like every other, this is not necessarily the case. Instead, fine-tuning is required, both at the time of the system’s installation and then regularly throughout its life cycle, as the laser pump, gain medium, and amplification cavity age. Most importantly, both OCT imaging systems and laser optics require precise alignment. I myself have experience with a misaligned laser that resulted in incomplete capsulotomies in 9% of cases! If you believe you have tags or discontinuous capsulotomies in greater than 3% of cases, start by screening the system settings to optimize energy and spot spacing. If the problem persists, insist on a service call from your manufacturer to check OCT and laser system alignment.
MINIMIZING THE OCCURRENCE OF INCOMPLETE CAPSULOTOMIES
The best way to manage incomplete laser capsulotomies is to adopt practices that minimize their occurrence in the first place. It should go without saying that you should be using the latest software available for your respective laser platform (LenSx v2.3, Victus v3.2, Catalys COS v3.0, Lensar Streamline). Software upgrades have resulted in faster raster speeds, which probably reduce the incidence of aberrant spots due to micromovements by the patient. In addition, careful selection should eliminate patients who have corneal scars or even a dense arcus within the laser treatment zone.
Watch it Now
Seth M. Pantanelli, MD, MS, demonstrates several pearls for preventing and managing incomplete laser capsulotomies.
When docking, insist on perfect centration, even if multiple attempts and additional time are required. Doing so optimizes the quality of the OCT image and, more importantly, eliminates lens tilt. This problem is not always obvious and can sometimes only be detected by looking at either the axial or sagittal cut through the lens on OCT imaging. It is important to note that even small degrees of lens tilt (ie, 7.5º) are enough to tip a portion of the anterior capsule that should be ablated out of the treatment zone.
Do not take for granted that all is well with docking just because the laser system says so. Even if adequate suction is confirmed, scrutinize enface and OCT images for movement of the eye if using the Catalys or Victus, because both systems display real-time images during the planning stage. Rarely, suction will be applied such that only the conjunctiva has adhered to the interface, leaving the eye to move freely beneath it. Such movement is dangerous and will most certainly lead to incomplete capsulotomies, irregular nuclear fragmentation patterns, and corneal wounds.
Specific situations may call for manual adjustments to the laser settings. For hypermature cataracts, I usually boost the laser energy by 10% and/or increase the height of the gates above and below the anterior capsule by 50 µm.
MANAGEMENT
Managing an incomplete capsulotomy starts with recognizing that it has occurred. When the capsulotomy is being created, confirm that a full 360º ring of “champagne bubbles” appears. If an area is untreated, these bubbles will get caught under the intact anterior capsule or may not form at all. After lowering the microscope into position, check whether the capsulotomy is complete. If not, you can perform manipulation under viscoelastic to determine the type and extent of the discontinuity. Nagy and colleagues published a grading system for this purpose5:
• complete treatment pattern or free-floating (type 1)
• microadhesions (type 2)
• incomplete treatment pattern (type 3)
• complete pattern but not continuous (type 4)
For microadhesions, I find that the dimple-down technique works well. It consists of simply inserting a closed Utrata forceps into the eye and pressing down in the center of the capsulotomy/lens. The motion creates a vector inward and breaks any remaining tags.
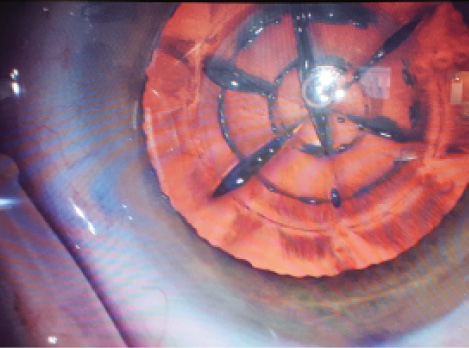
Figure 2. Type 3 laser capsulotomy in a patient with a history of prior radial keratotomy. One discontinuity is visible at 4 o’clock, a second at 6 o’clock, and a third at 7 o’clock.
For type 3 or 4 capsulotomies (Figure 2), more delicate maneuvers are required. Against the backdrop of a laser-created pattern of nuclear fragmentation, discerning the borders of the capsulotomy can be difficult. Consider staining with trypan blue, flipping the capsulotomy over to create a flap, and completing the opening as if it were a manual capsulorhexis.
CONCLUSION
Incomplete capsulotomies are a rare but important complication of laser cataract surgery. Routine system maintenance, special attention to alignment during docking, and the elimination of eye movements under suction all minimize the chance that the problem will occur. When it does happen, management is relatively straightforward as long as you recognize the discontinuity early.
1. Toto L, Mastropasqua R, Mattei PA, et al. Postoperative IOL axial movements and refractive changes after femtosecond laser-assisted cataract surgery versus conventional phacoemulsification. J Refract Surg. 2015;31(8):524-530.
2. Abell RG, Darian-Smith E, Kan JB, et al. Femtosecond laser-assisted cataract surgery versus standard phacoemulsification cataract surgery: outcomes and safety in more than 4000 cases at a single center. J Cataract Refract Surg. 2015;41(1):47-52.
3. Pantanelli SM, Diakonis VF, Al-Mohtaseb Z, Cabot F, Yesilirmak N, Kounis GA, et al. Anterior capsulotomy outcomes: a comparison between two femtosecond laser cataract surgery platforms. J Refract Surg. 2015;31(12):821-825.
4. Donaldson KE, Braga-Mele R, Cabot F, et al. Femtosecond laser-assisted cataract surgery. J Cataract Refract Surg. 2013;39(11):1753-1763.
5. Nagy ZZ, Takacs AI, Filkorn T, et al. Complications of femtosecond laser-assisted cataract surgery. J Cataract Refract Surg. 2014;40(1):20-28.
Seth M. Pantanelli, MD, MS
• assistant professor, Penn State Hershey Eye Center, Penn State Hershey Medical Center, Hershey, Pennsylvania
• (717) 531-5690; spantanelli@hmc.psu.edu; Twitter @spantanelli
• financial interest: none acknowledged