Optic capture is the gold standard for lens implantation in an eye with a ruptured capsule. When there is no possibility of anterior, posterior, or membrane capture, surgeons must choose anterior chamber IOLs (ACIOLs), iris fixation (sutured or enclavated), or scleral fixation (sutured or glue-assisted scleral tunnel). No definitive data to date indicate the superiority of one strategy over the others. An individualized algorithm is based on patient demographics and ocular anatomy. For complicated cataract surgery, the time elapsed and the surgeon’s comfort are additional factors.
AT A GLANCE
• No definitive data to date indicate the overall superiority of a single fixation strategy.
• A backup lens should be available for every cataract procedure.
• To address bag-lens subluxation, the author favors an ab externo, scleral, sutured lasso technique.
• Her preferred approach to secondary IOLs without capsular support is now glue-assisted sutureless scleral tunnel fixation.
PLAN B NEEDED
I believe a backup lens should be available for every cataract procedure. No one-piece IOL should ever be placed in the sulcus.1 If this lens is optic captured, the dioptric power need not be adjusted. Sulcus implantation without fixation requires capsular support and an IOL that is appropriate for the sulcus. Standard three-piece bag-lens designs are too short and flexible to remain reliably centered and stable, so they require at least one iris fixation suture.
The three-piece AQ series of IOLs with Elastimide haptics located 13.5 mm apart (STAAR Surgical) comprises the only FDA-approved lenses likely to fit every sulcus, but the silicone optic challenges the surgeon’s view for any subsequent retinal procedure. Were they available in the United States, the Sulcoflex IOL (Rayner Intraocular Lenses) would be optimal, or aphakic enclavated lenses would be a choice. Kelman-style, four-point-fixation, open-looped ACIOLs must be sized (white to white plus 1 mm), requiring a spectrum of sizes to be available or preoperatively calculated and ordered. Quick to implant, they demand a large incision and a peripheral iridectomy. An Osher untuck maneuver (pulling the optic proximally with a lens manipulator) avoids iris entrapment by the distal footplate. Sizing and positioning are confirmed with intraoperative gonioscopy.
ADDRESSING BAG-LENS SUBLUXATION AND FREE LENSES
A subluxated bag-lens or free implant should be fixated rather than exchanged. Exceptions to this rule are when the implant is damaged, single piece, or the wrong power for the desired refractive outcome. Fixation avoids endothelial trauma, an open chamber with all its risks, and added vitreous traction.
Subluxation
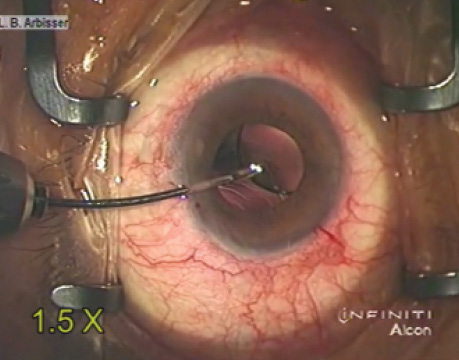
To address bag-lens subluxation, I favor an ab externo, scleral, sutured lasso technique. When facilitated by the presence of a capsular tension ring that allows fixation in any meridian, the procedure can be accomplished through small self-sealing incisions, rarely requires a vitrectomy, and liberates almost no antigenic lens material in my experience. A preoperative evaluation of the supine patient should confirm that the complex does not flip back into the midvitreous, which signals the need for an extensive vitrectomy and levitation. There are many variations on this technique, including using a snare to retrieve needleless suture ends as well as docking into a bored needle placed 3.5 mm back from the scleral spur for the loop under the bag and 1 mm behind for the one on top. I favor 7–0 Gore-Tex sutures (off-label indication; W.L. Gore & Associates), which are FDA approved for cardiovascular use (Figure). They have no history of breakage, which is valuable in all cases but which I think is critical when the suture is used in a young patient or it is placed through an islet such as a modified capsular tension ring or segment. The needle, not ideal for an ab interno pass, requires straightening for docking. It is important not to overtighten the suture. All techniques require burial of the suture knot. A Hoffman pocket spares conjunctiva.
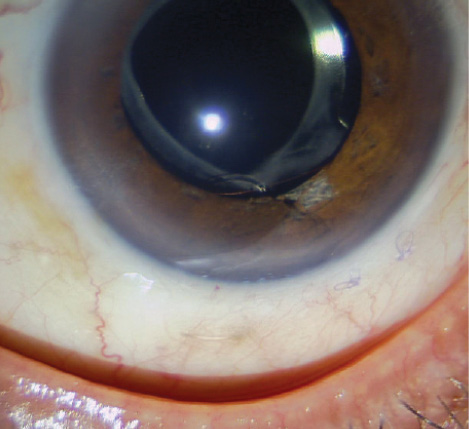
Figure. A Gore-Tex suture secures a Cionni Ring for Scleral Fixation, shown here 3 years postoperatively. The eye has been stable now for 10 years.
Free Lens
The strategy for a free subluxated lens depends on the preoperative evaluation, both undilated and dilated by gonioscopy as well as the slit-lamp examination. If aphakic vision is good and the eye is quiet, a contact lens or aphakic spectacles remain an option, but both are rarely employed. If the patient’s symptoms are ameliorated with miosis, a medical option exists.
Watch it Now
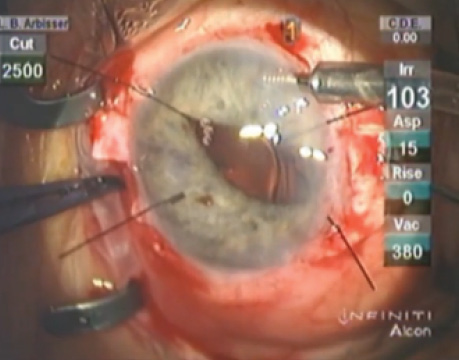
Lisa Brothers Arbisser, MD, is about to grasp the leading haptic tip with a forceps inserted through the sclerotomy to facilitate the haptic’s externalization during glueassisted scleral tunnel fixation of an IOL.
Dr. Arbisser performs iris fixation of a subluxated threepiece IOL. While performing irrigation with acetylcholine for miosis, she uses forceps to grasp the optic, elevate it above the iris plane, and capture it for iris fixation.
I recommend iris fixation if no vitreous presents and the iris architecture is normal. If vitrectomy is indicated, I perform glue-assisted scleral tunnel fixation. This technique, originated by Scharioth and elaborated on by Agarwal, negates the need for a single-piece PMMA lens inserted through a large incision with its eyelet sutured for scleral fixation. Although a cow hitch around eyelets and wide suture placement minimize tilt, tunnel fixation of a small-incision foldable lens eliminates suture erosion and breakage and leads to a quieter eye without pseudophacodonesis. A decade of experience shows value in adopting this technique.2,3
The technique requires sufficient conjunctiva covering flaps positioned with a toric marker exactly 180º apart. I find a guarded diamond blade helpful for achieving a consistent flap depth. A thorough anterior vitrectomy is necessary (through sclerotomies created with a 23-gauge microvitreoretinal blade under partial-thickness flaps) so that IOLs are not manipulated through vitreous. A handshake technique and iris hook sleeve prevent the IOL from dropping. Using microforceps, I gently handle haptics at their tip to avoid crimping and breakage. I also ensure that the haptics are sufficiently long to tuck into parallel tunnels made at the limbus with a 26-gauge needle close to opposite edges of the flaps. Carefully removing any prolapsed vitreous through the sclerotomies with the vitrector against the sclera prevents incarceration and traction. An anterior chamber maintainer (or pars plana infusion in totally vitrectomized eyes) will maintain normotension replaced with viscoelastic once the IOL is in place, leaving a dry bed for glue adhesion.
SECONDARY IOLs
My preferred approach to secondary IOLs without capsular support has changed over the years. I moved from anterior chamber implantation to two-point iris fixation finally to glue-assisted sutureless scleral tunnel fixation.
In all of these challenging scenarios, the surgeon’s attention to detail lets patients enjoy quiet eyes and excellent visual acuity.
1. Chang DF, Masket S, Miller KM, et al. Complications of sulcus placement of single-piece acrylic intraocular lenses: recommendations for backup IOL implantation following posterior capsule rupture. J Cataract Refract Surg. 2009;35(8):1445-1458.
2. Kumar DA, Agarwal A, Packiyalakshmi S, et al. Complications and visual outcomes after glued foldable intraocular lens implantation in eyes with inadequate capsules. J Cataract Refract Surg. 2013;39(8):1211-1218.
3. McKee Y, Price FW, Feng MT, et al. Implementation of the posterior chamber intraocular lens intrascleral haptic fixation technique (glued intraocular lens) in a United States practice: outcomes and insights. J Cataract Refract Surg. 2014;40(12):2099-2105.
Lisa Brothers Arbisser, MD
• emeritus position at Eye Surgeons Associates, the Iowa and Illinois Quad Cities
• adjunct associate professor, John A. Moran Eye Center, University of Utah, Salt Lake City
• (563) 343-8896; drlisa@arbisser.com
• financial interest: none acknowledged