
Although more than one-third of the population has greater than 1.00 D of astigmatism, toric IOLs represent only 7% of all IOLs implanted,1 so there is definitely room for growth. In patients with high amounts of astigmatism, a toric IOL offers the only chance of achieving spectacle independence for distance. Approximately 9% of the population has more than 2.00 D of astigmatism,2 and until recently, surgeons had few options to correct significantly more than 2.00 D.
Abbott Medical Optics has introduced three new cylinder powers (Table); these single-piece acrylic IOLs are now available to correct astigmatism ranging from 1.50 to 6.00 D or up to about 4.75 D at the corneal plane. Because there are differences between the toric IOL platforms and nontoric IOLs in general in terms of index of refraction and, for example, chromophore that might be detectable to the patient, many surgeons prefer to implant the same type of lens in both eyes of a given patient whether toric or not. For those who prefer Tecnis lenses (Abbott Medical Optics), as I do, the expanded range means we can proceed with our lens of choice knowing that we will later be able to match it for the second eye, regardless of the amount of astigmatism. Other toric options, including the STAAR Toric silicone plate lens (STAAR Surgical) and the Trulign modified plate haptic lens (Baush + Lomb) can correct up to about 2.50 D of astigmatism at the corneal plane.
PERSONAL EXPERIENCE
I used the Tecnis with the highest cylinder power (ZCT600) on the first day it became available, and I have been obtaining excellent results with it since then, with about 90% of eyes having a UCVA 20/25 or better after surgery. Nearly 95% of the eyes that I have implanted with these lenses have had residual astigmatism of less than or equal to 0.50 D after cataract surgery. I have not had to explant or rotate any of the lenses.
I recently performed surgery on a 67-year-old patient who had a manifest refraction of -5.75 +5.75 × 019 with keratometry readings of 41.25 D @ 109º and 45.00 D @ 19º OD and -8.50 +7.00 × 006 with keratometry readings of 41.25 @ 94º and 45.75 D @ 004º OS. I operated on the left eye first, and I implanted a +14.50 D ZCT600 lens. For the right eye, after using the toric calculator, I used a ZCT525 +18.00 D lens. The patient had less than 0.50 D of astigmatism postoperatively and was thrilled with the results after a lifetime of correction for the significant astigmatism she had. Any eye care professional can readily imagine what an impact correcting this much cylinder can have, just like prescribing glasses or contact lenses with this much astigmatism correction for the first time.
In addition, in my experience, the Tecnis Multifocal is a very stable lens that performs well in low light, owing to the low index of refraction and high Abbe number that are characteristic of this line of lenses. These features reduce chromatic aberration and help to maintain good contrast sensitivity and quality of vision in dim light. Practically speaking, I like that the entire Tecnis line of IOLs has exactly the same A-constant; it makes choosing the appropriate IOL power easy, even for a surgeon just getting started with toric lenses, high-cylinder toric IOLs, or multifocal IOLs.
TAKING CARE OF PATIENTS
Preoperatively, I always have a signficant level of suspicion of ocular pathology when there is high cylinder. It is important to ensure that the astigmatism is regular, especially in the central cornea, and to look carefully for corneal disease and ocular surface problems that could be contributing to or masquerading as high astigmatism. I prefer to use an advanced topography or anterior segment tomography device such as the Orbscan (Bausch + Lomb), Pentacam Comprehensive Eye Scanner (Oculus Surgical), or Visante (Carl Zeiss Meditec) to carefully evaluate the cornea.
I also take extra care with preoperative marking and intraoperative alignment. There is a 3.3% loss of effect of the toric IOL power for each degree of cyclorotation of the lens.3 At lower levels of astigmatism, being off axis may reduce the correction but still leave the patient with satisfactory visual acuity. That is not likely to be the case with a 10º rotational error in a patient with 4.00 D of astigmatism.
The rewards of correcting high cylinder are well worth a little extra effort. Postoperatively, these patients are some of the happiest in my practice.
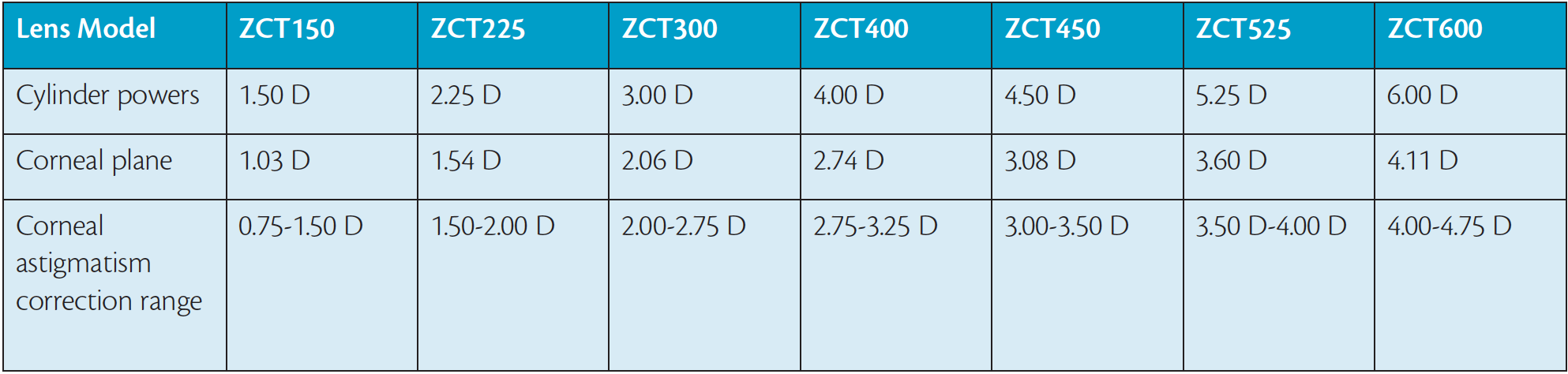
Table. The range of cylinder powers now available in the Tecnis Toric IOL. The ZCT450, 525, and 600 models are new to the market.
START SIMPLY
Intraoperative aberrometry and surgical guidance systems such as the ORA System and Verion (both from Alcon), the TrueVision 3D Visualization and Guidance System (TrueVision Systems), Cassini Total Corneal Astigmatism (i-Optics), or Callisto Eye (Carl Zeiss Meditec) are certainly useful for refining toric IOL outcomes, but not having access to these devices should not be considered a barrier to the implantation of toric IOLs. Just a few simple steps can ensure successful outcomes:
- Be consistent. It is a good idea to measure astigmatism using several different methods, but surgeons should choose a primary method for determining the magnitude and axis of astigmatism and consistently use that method to personalize nomograms and lens constants. I rely on my Atlas 9000 topographer (Carl Zeiss Meditec) for the axis but use the keratometry readings from my optical biometry device (I have a Lenstar [Haag-Streit] in one office and an IOLMaster [Carl Zeiss Meditec] in another) for the magnitude of astigmatism.
- Use the toric calculator. Each manufacturer offers an online calculator for its toric lenses. I use www.tecnistoriccalc.com to calculate the optimal IOL cylinder value based on axial length and personalized A-constants. This calculator will soon incorporate an algorithm for posterior corneal astigmatism, eliminating the need for me to also check the Barrett calculator on the American Society of Cataract and Refractive Surgery’s website.
- Mark preoperatively with the patient sitting up. Ask the patient to look off in the distance over your shoulder to minimize cyclorotation. I like to mark the eye at 3, 6, and 9 o’clock with a fine-tipped marking pen on a dry cornea if I am not using the ORA System.
- Use an axial marker to mark the exact axis of astigmatism on the table, after draping but before instilling any drops. An old radial keratotomy or limbal relaxing incision marker will suffice, or an inexpensive tool for this purpose can be purchased such as a Mendez Degree Gauge. Simply align the corneal marker with the 90º/180º (6, 3- and 9-o’clock) marks, and then find the exact axis of astigmatism. Mark the axis and intended incision location. Then, after phacoemulsification, simply rotate the IOL in the bag to align it with the corneal axis marks.
- Perform careful surgery. Overly aggressive cortical cleanup is not necessary in general for toric IOLs, but be sure to remove all the cortical material and viscoelastic by irrigating and aspirating behind the lens if necessary. Try to leave the eye at physiologic pressure rather than overfill it. Check that wounds are watertight, and inspect incisions and IOL placement one last time at the end of surgery.
CONCLUSION
The tools and steps needed to achieve excellent results with high-cylinder toric lenses are minimal. Although there are relatively few patients who fall into the high ranges of astigmatism, the rewards of offering them toric correction at the time of cataract surgery are great.
1. Market Scope. Comprehensive Report on Global IOL Market. 2013.
2. Ostri C, Falck L, Boberg Ans G, Kessel L. The need for toric intraocular lens implantation in public ophthalmology departments. Acta Ophthalmol 2015;93:e396-397.
3. Rho CR, Joo CK. Effects of steep meridian incision on corneal astigmatism in phacoemulsification cataract surgery. J Cataract Refract Surg. 2012;38(4):666-671.
Francis S. Mah, MD
• director of cornea and external diseases and codirector of refractive surgery at the Scripps Clinic Torrey Pines in La Jolla, California
• (858) 554-7996; mah.francis@scrippshealth.org.
• financial disclosure: consultant to Abbott Medical Optics, Alcon, and Bausch + Lomb


