
Ensuring the health of the ocular surface before moving a patient to the OR is fundamental to achieving an optimal surgical outcome. In the context of cataract and refractive surgery patients, each procedure yields a cutdown of the corneal nerves—although the mechanisms for achieving this are distinct. There is debate over whether mechanical or laser-based incisions are more damaging, but both procedures introduce the possibility of inducing neurotrophic dry eye.
AT A GLANCE
• Ensuring the health of the ocular surface before performing any surgery is key to achieving optimal visual outcomes.
• A unhealthy ocular surface negatively affects preoperative measurements, because about 75% of the eye’s refractive power occurs at the ocular surface.
• The author recommends examining the lid margins and expressing the lid margins of the meibomian glands.
Ensuring that the ocular surface is healthy before cataract or refractive surgery also reduces the possibility of inaccurate biometry and keratometry. Because about 75% of the eye’s refractive power occurs at the ocular surface, any abnormalities increase the possibility that readings will be incorrect and that, as a result, the IOL power or laser ablation pattern may be incorrect.
Another consideration with regard to the ocular surface is that lingering postoperative dry eye disease (DED) or meibomian gland dysfunction (MGD) portends slower healing. One could argue that the delayed recovery of visual ability is more consequential for patients undergoing surgery specifically for refractive purposes, yet other categories of patients, for example, those undergoing procedures to fix a corneal structural defect (eg, corneal collagen cross-linking [CXL] or keratoplasty), require equal consideration of the health of the ocular surface preoperatively.
CONSEQUENCES OF DELAYED HEALING
The first 3 to 5 postsurgical days are crucial for a successful outcome after keratoplasty. During the early postoperative period, the epithelial layer heals over the transplant while the surgical abrasion resolves. Thus, the risk of rejection and infection are highest during this period.1
For the patient with untreated DED or MGD, however, that healing period is potentially extended, so the risk of rejection or infection is higher. Any patient undergoing a keratoplasty procedure who has aqueous deficiency has to be treated with some modality to improve tear production, whether it be cyclosporine ophthalmic solution 0.05% (Restasis; Allergan), punctal plugs, or the frequent use of artificial tears before the transplant. In patients with MGD, the need for proper treatment preoperatively may be more pressing, because affected meibomian glands can act as a reservoir for microbes, which can heighten the risk of infection.
With respect to CXL, the ultraviolet light used during the procedure can affect the ocular surface of an eye with untreated DED. In this scenario, there is a risk of causing discomfort during and after the procedure as well as the potential to slow healing and extend the time it takes for the topography to normalize, especially if epithelium-off CXL is performed.
DIRECTED TESTING
My protocol for evaluating surgical candidates’ ocular surfaces does not change too much based on the procedure planned. In my colleagues’ and my practice, we start most patients with the Standard Patient Evaluation of Eye Dryness (SPEED) questionnaire, and our technicians can evaluate the results to determine if an additional workup is warranted. If the SPEED questionnaire is suggestive of DED and/or MGD, then the patient will be moved directly to analysis with the LipiView Ocular Surface Interferometer (TearScience), regardless of the surgical indication. In particular, the system’s Dynamic Meibomian Imaging is important for identifying gland morphology. In our experience, anything more than 50% blockage indicates a need to delay surgery and initiate treatment.
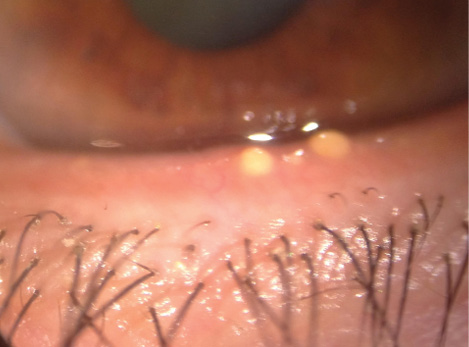
Figure 1. Severe inspissation of the meibomian glands was discovered with frank obstruction of several glands.
For patients undergoing cataract and refractive surgeries, we have found the InflammaDry test (Rapid Pathogen Screening), which tests for the presence and activity of matrix metallopeptidase 9, to be important, because it gives us a sense of the level of inflammation present at the ocular surface. Another point-of-care test, tear osmolarity testing (TearLab), has been shown to be effective in identifying patients with a higher likelihood of an unexpected refractive error resulting from inaccurate biometry.2 Topographic mapping may also provide clues to the status of the ocular surface with dropout regions or irregular mires on Placido disc images. Managing patients’ expectations through education is especially important for individuals receiving premium lens implants.
During the examination portion of the ocular surface assessment, it is important to look at the lid margins. Something I do now that I did not do earlier in my career is to express the lid margin of the meibomian glands. I am looking for an olive oil consistency as an indication of properly functioning glands; anything else, and I am directed to investigate for potential MGD. For example, “soapsuds” or the presence of oil globules in the tear film as well as inspissated meibomian glands are pathognomonic of MGD.
Less high-tech diagnostics also play an important role in the workup. We use vital dye staining (lissamine green) and a tear meniscus evaluation as the basis for understanding the nature of the tear film. Overall, these diagnostic modalities add to the clinical impression; I am not sure if one in particular is more important than the next.
CASE EXAMPLES
No. 1
MGD is extremely important to identify and treat prior to cataract surgery or corneal transplantation. Left untreated, it increases the risk that microbial agents will enter the eye during surgery, thus creating a heightened chance of endophthalmitis.
A 52-year-old man was scheduled for corneal transplantation due to advanced keratoconus. During the preoperative evaluation, severe inspissation of meibomian glands was discovered with frank obstruction of several glands (Figure 1). A LipiFlow treatment was performed, and the patient was scheduled for a deep anterior lamellar keratoplasty 4 weeks later. A postoperative photograph shows a stable keratoplasty and much improved appearance of the lower eyelid with no signs of meibomian gland inspissation 6 months after the Lipiflow treatment (Figure 2).
No. 2
Evaluating the corneal surface via a review of corneal topography and biometry, in conjunction with a careful slit-lamp examination of the ocular surface prior to cataract surgery, is extremely important. If they are not treated in advance, corneal diseases such as epithelial basement membrane dystrophy and Salzmann nodules can have an impact on cataract surgery outcomes A 72-year-old woman with a decreased visual acuity of 20/80 OS presented for cataract surgery. The slit-lamp examination showed a peripheral Salzmann nodule (Figure 3), and corneal topography revealed significant irregular astigmatism with a normal topography and a clear cornea in the right eye. Biometry showed an average keratometry value of 42.87 D. The nodule was removed using a superficial keratectomy; after 6 weeks, the corneal surface normalized, and the cornea appeared clear. The corneal topography normalized, and repeat biometry showed an average keratometry value of 44.75 D. This led to the selection of an IOL power that was 4.00 D higher than originally planned.
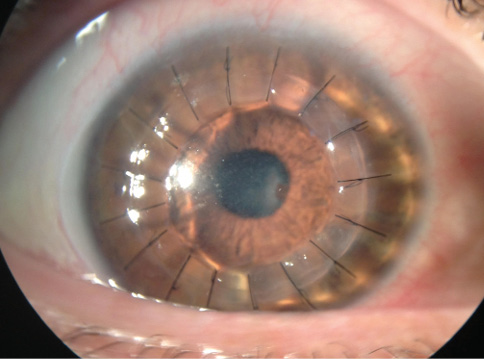
Figure 2. Postoperatively, the keratoplasty was stable, and the appearance of the lower eyelid had improved, with no signs of meibomian gland inspissation 6 months after the LipiFlow treatment of the eye shown in Figure 1.
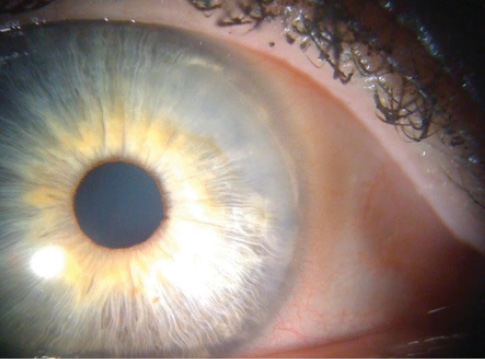
Figure 3. A slit-lamp examination showed a peripheral Salzmann nodule.
Without removal of the nodule prior to the cataract surgery, the patient would have experienced a hyperopic surprise with irregular astigmatism, leading to an unsatisfactory visual outcome.
CONCLUSION
The ocular surface’s health is one of the most important factors in the success of surgery and a positive visual outcome. Whether the patient is undergoing cataract surgery or a corneal transplant, the surgeon has to look at the ocular surface to understand how it may affect outcomes and then initiate aggressive treatment to optimize the surface prior to surgery. Identifying problems beforehand means not having to do as much explaining afterward.
1. Sugar J, Montoya M, Dontchev M, et al. Donor risk factors for graft failure in the cornea donor study. Cornea. 2009;28:981-985.
2. Epitropoulos A, Matossian C, Berdy G, et al. Effect of tear osmolarity on repeatability of keratometry for cataract surgery planning. J Cataract Refract Surg. 2015;41(8):1672-1677.
W. Barry Lee, MD
• partner at Eye Consultants of Atlanta
• comedical director of the Georgia Eye Bank, Atlanta
• lee0003@aol.com
• financial disclosure: member of the speakers’ bureaus for Allergan and Bausch + Lomb; consultant to Shire


