
Preoperative soft contact lens (SCL) cessation has been part of the corneal refractive surgery protocol for decades. In the original FDA excimer laser trials conducted more than 2 decades ago, the SCL cessation period before assessment and surgery ranged from 3 days to 2 weeks. Currently, the FDA website and the United Kingdom’s Royal College of Ophthalmologists recommend cessation periods of 2 weeks and 1 day, respectively. This wide discrepancy and a lack of specific guidelines reflect the paucity of studies underlying the requirements.
Discontinuing SCL wear before testing and surgery can greatly inconvenience patients. A review of the protocol is long overdue.
THE PUBLISHED LITERATURE
Most studies of corneal changes after CL discontinuation were conducted more than 13 years ago.1-8 The studies focused primarily on changes in topography1-4 and pachymetry5,6 or dealt with rigid CLs.7,8 The few recent studies on SCL discontinuation revealed no significant changes in biometry,9 but a small study found corneal warpage in one-third of eyes that took 1 to 3 weeks to resolve.10 Lloyd-McKernan et al reported that SCL cessation 2 weeks and 1 day before corneal refractive surgery did not adversely affect refractive outcomes when compared to the control group.11
Only recently have large studies on the results of corneal refractive surgery after short-term SCL discontinuation been reported. In 2020, Shehadeh-Mashor et al published the most definitive study to date on the subject.12 The retrospective review assessed 20,000 eyes after three different periods of SCL cessation—less than 24 hours, 1 to 3 days, and more than 3 days—with a spectacle-use group serving as controls. After adjusting for baseline variables, the efficacy index after PRK was significantly lower among eyes in which the period of SCL discontinuation was less than 24 hours. No differences, however, were found in the predictability and safety indexes between eyes (Figure 1). In the LASIK group, after adjusting for baseline variables, no significant difference was found for any of the outcomes (Figure 2).
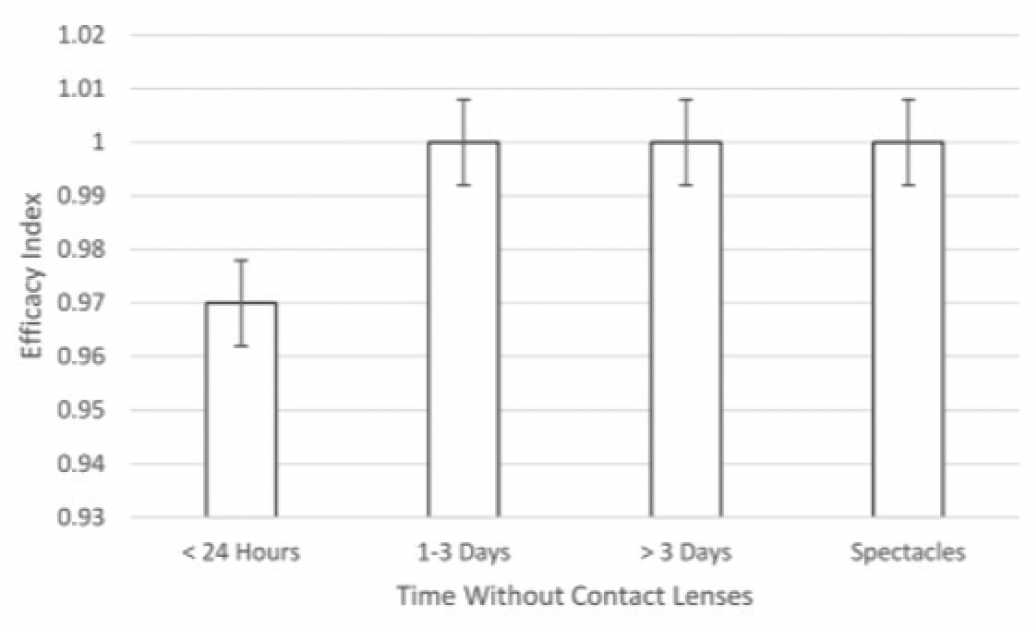
Figure 1. PRK outcomes after corneal refractive surgery.
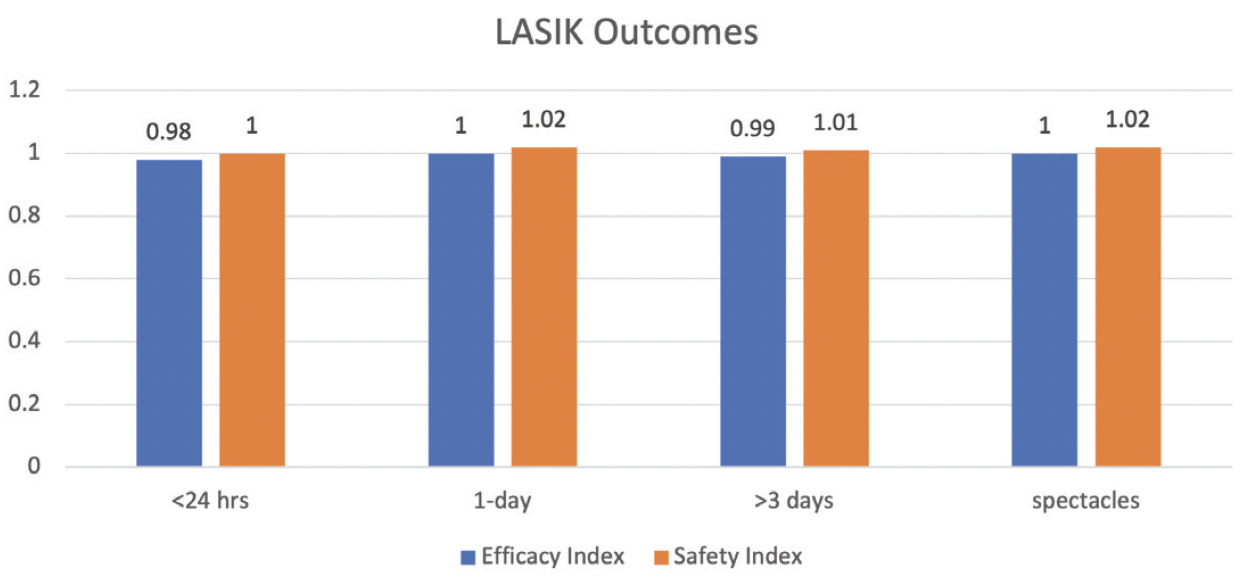
Figure 2. LASIK outcomes after corneal refractive surgery.
Figures 1 and 2 reprinted with permission from Shehadeh-Mashor R, Mimouni M, Shapira Y, Sela T, Munzer G, Kaiserman I. Duration of contact lens removal before myopic refractive surgery. Eur J Ophthalmology. 2021;31(4):16-95-1699.
A retrospective study in 2017 evaluated refractive results 1 month after LASIK in 4,133 eyes.13 The periods of SCL cessation were 1, 2, 3, 4 to 13, and greater than 14 days. No clinically significant differences in visual results, predictability, changes in BCVA, or patient satisfaction were found (Figure 3).
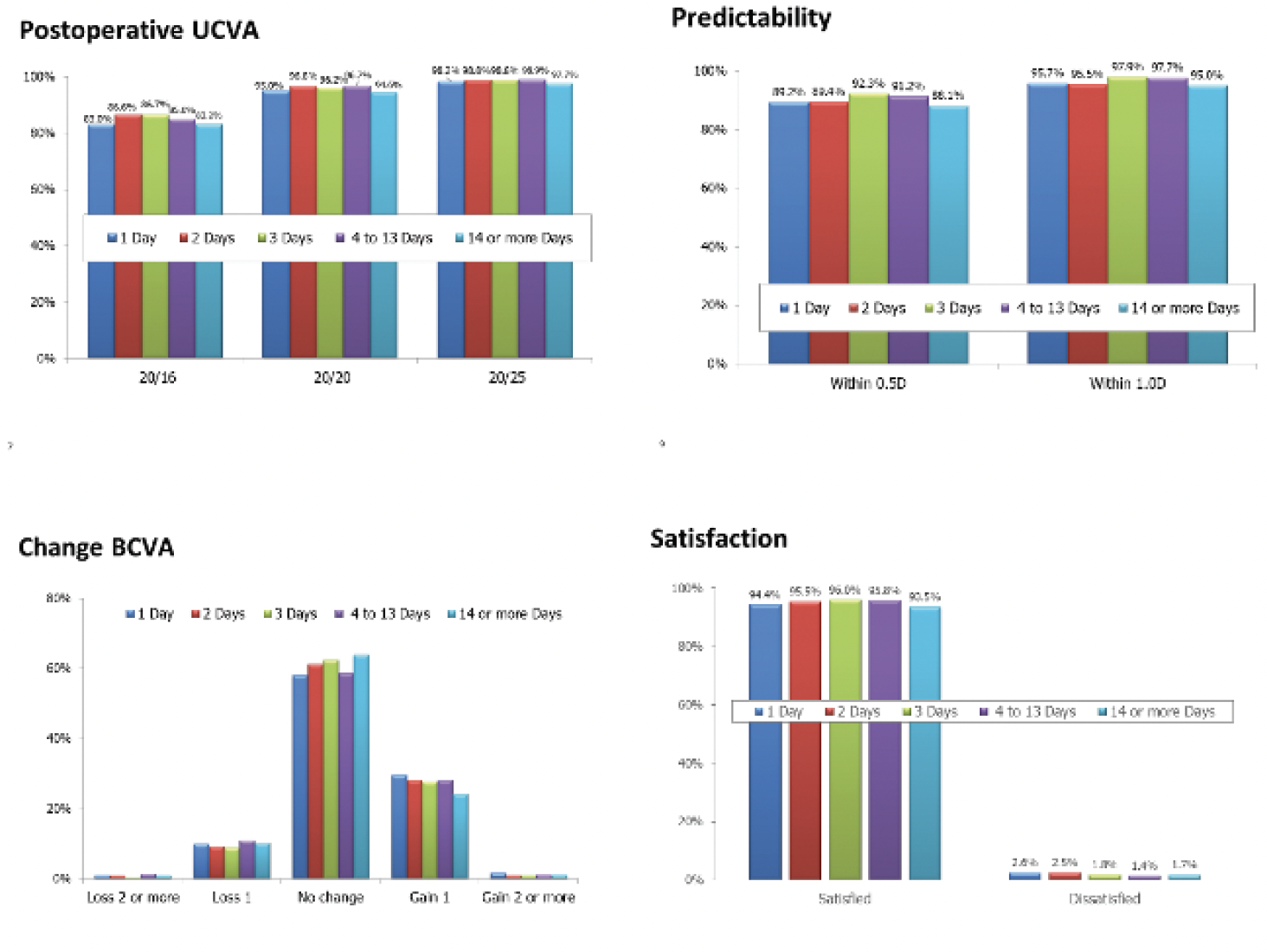
Figure 3. LASIK outcomes after corneal refractive surgery.
Courtesy of John Vukich, MD
SCL TECHNOLOGY
Advances. SCLs have undergone significant improvements during the past 25 years.14-17 Since the late 1990s, the addition of silicone to the hydrogel material has increased oxygen transmission as much as sixfold compared to the first generation of hydrogel SCLs. The introduction of silicone, however, also increased SCL stiffness and repelled water, leading to several innovations since 2013.
- Nanostructures were added to increase oxygen transmission.
- Water gradient zones were created within SCLs.
- Hydrogel channels were developed on the surface of SCLs to hold water, which has made lens wear more comfortable.
- Silicone channels were added to the core of SCLs to increase oxygen transmission.
- Hydrophilic molecules were bonded to the silicone material to allow a higher water content.
Modern SCLs are quite different from the lenses for which a discontinuation period of up to 2 weeks was required in the original FDA excimer laser trials.
Differences in design. The two large studies cited earlier12,13 did not differentiate between spherical SCLs and soft toric CLs (STCLs). Smaller studies, however, have found differences in the time required to restore corneal stability after the cessation of spherical daily use SCLs, STCLs, and extended wear SCLs. In a study by Wang et al,3 the recovery time after CL cessation for refraction, keratometry, and topography was more than two times and almost four times longer for STCLs and extended wear SCLs, respectively, compared to spherical daily wear SCLs. Ng et al also reported that extended wear SCLs were associated with the longest time to restored stability.2
REVISED RECOMMENDATIONS
A discontinuation period of 4 weeks per decade of use is still required for rigid gas permeable lenses. This can be facilitated by having patients switch to SCLs and monitoring them for corneal stability. PMMA lenses are rarely used anymore but may require an even longer period of discontinuation to achieve corneal stabilization.
Based on the large studies discussed here, a 1-day SCL cessation period should be adequate for LASIK, but more than 24 hours may be appropriate for PRK.12 The smaller studies discussed suggest that a longer period of discontinuation may be required for STCLs if there are signs of refractive instability, corneal warpage, or corneal irregularity on topography or tomography.
The 1-day SCL discontinuation period is acceptable only if the refraction and ocular examination during the initial assessment and on the procedure day are normal. A period of 7 days or longer and a reevaluation may be necessary if there is an inconsistency or instability in the refractions compared to previous measurements or other testing, reduced BCVA, topographic changes or abnormalities, or ocular pathology.
1. Budak K, Hamed AM, Friedman NJ, Koch DD. Preoperative screening of contact lens wearers before refractive surgery. J Cataract Refract Surg. 1999;25(8):1080-1086.
2. Ng LT, Lee EM, Nguyen AL. Preoperative assessment of corneal and refractive stability in soft contact lens wearing photorefractive candidates. Optom Vis Sci. 2007;84(5):401-409.
3. Wang X, McCulley JP, Bowman RW, Cavanagh HD. Time to resolution of contact lens-induced corneal warpage prior to refractive surgery. CLAO J. 2002;28(4):169-171.
4. Hashemi H, Firoozabadi MR, Mehravaran S, Gorouhi F. Corneal stability after discontinued soft contact lens wear. Cont Lens Anterior Eye. 2008;31(3):122-125.
5. Nourouzi H, Rajavi J, Okhovatpour MA. Time to resolution of corneal edema after long-term contact lens wear. Am J Ophthalmol. 2006;142(4):671-673.
6. Yeniad B, Yiğit B, Işsever H, Közer Bilgin L. Effects of contact lenses on corneal thickness and corneal curvature during usage. Eye Contact Lens. 2003;29(4):223-229.
7. Tsai PS, Dowidar A, Naseri A, McLeod SD. Predicting time to refractive stability after discontinuation of rigid contact lens wear before refractive surgery. J Cataract Refract Surg. 2004;30(11):2290-2294.
8. Perlman EM, Reinert SE. Factors influencing the need for enhancement after laser in situ keratomileusis. J Refract Surg. 2004;20(6):783-789.
9. Goudie C, Tatham A, Davies R, Sifton A, Wright M. The effect of the timing of the cessation of contact lens use on the results of biometry. Eye (Lond). 2018;32(6):1048-1054.
10. Rayess Y, Arej N, Abdel Massih Y, Antoun J, Waked N. Influence of soft contact lens material on corneal warpage: prevalence and time to resolution. Can J Ophthalmol. 2018;53(2):135-138.
11. Lloyd-McKernan A, Simo Mannion L, O’Dwyer V. The effect of previous soft contact lens wear on corneal refractive surgery outcomes. Cont Lens Anterior Eye. 2017;40(5):301-310.
12. Shehadeh-Mashor R, Mimouni M, Shapira Y, Sela T, Munzer G, Kaiserman I. Duration of contact lens removal before myopic refractive surgery. Eur J Ophthalmology. 2021;31(4):16-95-1699.
13. Vukich JA, Schallhorn S. Time out of SCL before initial consultation. Paper presented at: Hawaiian Eye 2017; January 14–20, 2017; Koloa, Hawaii.
14. Nicolson PC, Vogt J. Soft contact lens polymers: an evolution. Biomaterials. 2001;22(24):3273-3283.
15. Stapleton F, Stretton S, Papas E, Skotnitsky C, Sweeney DF. Silicone hydrogel contact lenses and the ocular surface. Ocul Surf. 2006;4(1):24-43.
16. Mutlu Z, Shams Es-Haghi S, Cakmak M. Recent trends in advanced contact lenses. Adv Healthc Mater. 2019;8(10):e1801390.
17. Gurnani B, Kaur K. Contact Lenses. 2022. In: StatPearls [Internet]. StatPearls Publishing; 2023.




