I used to be reluctant to suggest an extended depth of focus (EDOF) IOL to anyone with a compromised ocular surface. Positive outcomes with the Tecnis Symfony OptiBlue IOL (Johnson & Johnson Vision) in some patients with corneas that are less than perfect, however, prompted me to suggest this lens to the patient described in the following case presentation.
Case Presentation
A 70-year-old comedic stage performer presented for a cataract evaluation. His preoperative BCVA was 20/80 OD and 20/50 OS with glare disability reducing his visual acuity to 20/400 OD and 20/80 OS. Both corneas exhibited small branch-like deposits interspersed with clear areas in the central corneal stroma along with 2+ nuclear sclerotic and cortical cataracts. The remainder of the ocular examination was unremarkable.
The patient was diagnosed with lattice corneal dystrophy type 1, which affects the corneal stroma (Figure 1). It is one of the most common corneal dystrophies and results in the deposition of small branching patterns of a protein called amyloid in the central corneal stroma. Lattice corneal dystrophy type 1 is caused by genetic changes in the TGFBI gene and is inherited in an autosomal dominant manner. The condition often diminishes the patient’s visual acuity and, in severe cases, may necessitate corneal transplantation.
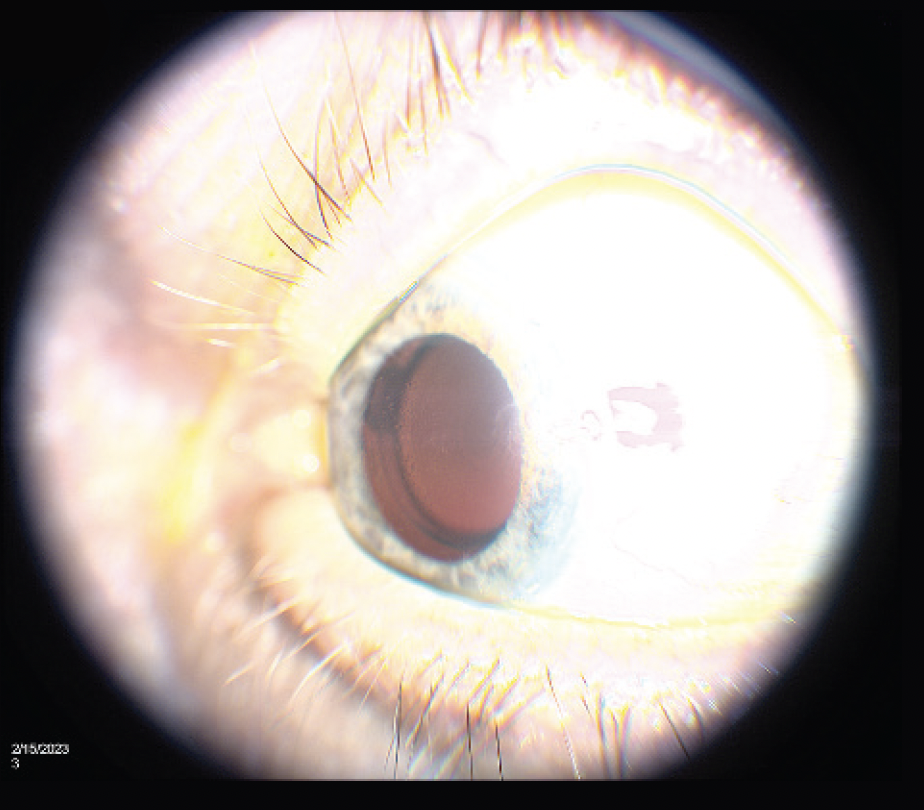
Figure 1. Slit-lamp photograph demonstrates the appearance of small central branching amyloid deposits consistent with lattice corneal dystrophy.
The patient in this case is a frequent performer on cruise ships and in Las Vegas. He complained that glare and bright stage lights had recently become more annoying. I cautioned him that the presence of corneal deposits would limit his postoperative visual outcome, but he was highly motivated to receive a multifocal IOL, which would allow him to check his set list occasionally while maintaining a view of the audience during performances.
After a thorough discussion of the risks and benefits, he opted to proceed with cataract surgery and implantation of a Tecnis Symfony OptiBlue IOL (Figure 2).
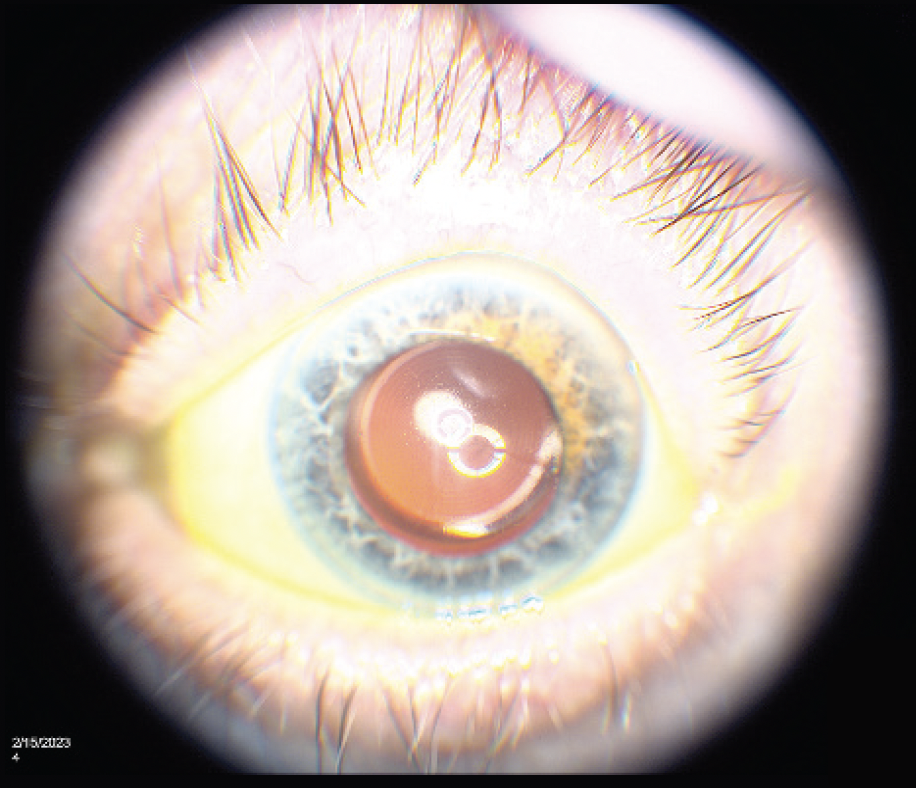
Figure 2. A Symfony OptiBlue IOL is centered in the capsular bag (B).
Surgery was successfully completed in each eye (2 weeks apart). A 5.1-mm capsulorhexis and self-sealing incisions were created. Centration of the IOL on the visual axis was verified with Purkinje images.
Outcome
Two weeks postoperatively, the patient’s UCVA was 20/30 OU, and he reported great satisfaction with his results. At the 6-week postoperative visit, his UCVA was 20/30 OU at distance and J2 at intermediate. The patient can now read books and his notes without glasses and view the audience with far less sensitivity to stage lighting.
I recommend the Symfony OptiBlue over a multifocal IOL to patients who desire excellent uncorrected distance and intermediate visual acuity and might be extra sensitive to halos.