CASE PRESENTATION
A healthy 45-year-old woman with myopic astigmatism presented for a refractive surgery evaluation. The patient’s BCVA was 20/20 OU with a manifest refraction of -4.50 -0.25 x 105º OD and -4.25 -0.50 x 50º OS. Preoperative topography and tomography were within normal limits. There were no signs of corneal thinning or ectasia. Epithelial thickness maps were within normal limits overall, and central corneal thickness was 529 µm OD and 522 µm OS (Figures 1 and 2). Mild dryness and punctate keratopathy were evident in the right eye.
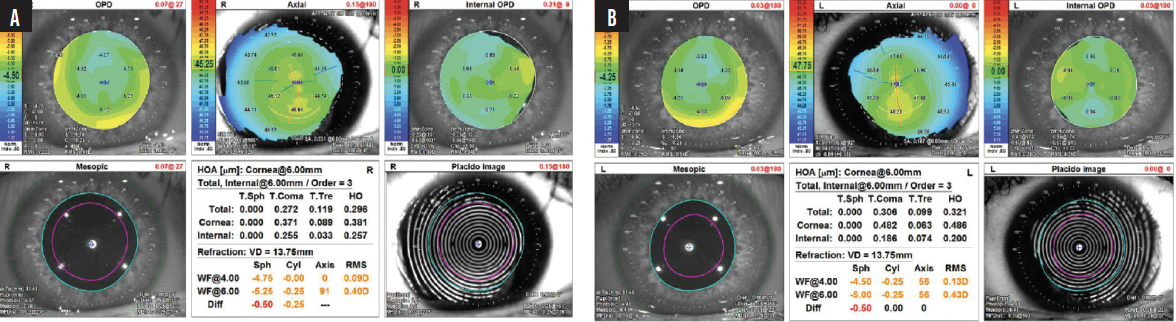
Figure 1. Preoperative topography of the right (A) and left (B) eyes show a normal corneal contour. The patient has myopic astigmatism with a low magnitude of preoperative higher-order aberrations.
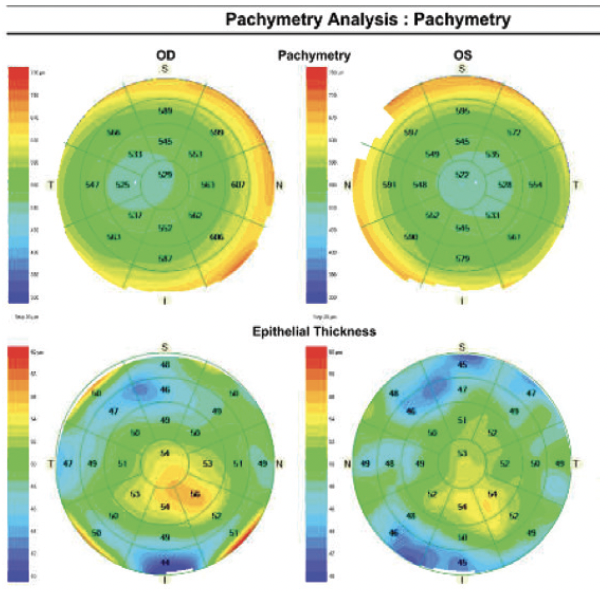
Figure 2. Preoperative epithelial pachymetry and thickness maps show normal corneal thickness in each eye. There are foci of epithelial hyperplasia in both eyes.
After a discussion of the surgical options and their risks and benefits, the patient decided to proceed with SMILE in both eyes. A distance target was selected for the dominant right eye. Given her age, -0.50 D was targeted in the nondominant left eye to preserve some near vision. She was instructed to start a regimen of artificial tears and lubricating ointment at night in each eye to address mild dry eye disease.
Surgery was uncomplicated aside from the development of a partial epithelial defect in the right eye during massage of the SMILE cap with a Weck-Cel sponge (BVI Medical) to ensure strong adherence of the cap to the underlying stroma. The defect extended from above the superior incision into the central cornea. A bandage contact lens was placed to help the epithelium heal overnight. The left eye had no frank epithelial disruption, but the epithelium was noted to be slightly loose intraoperatively.
One day after surgery, the patient’s UCVA was 20/50 OD and 20/20 OS. Several epithelial clusters were observed in the right eye, and the surface of the central cornea was irregular. The interface, however, was clear (Figure 3). The epithelium and SMILE cap of the left eye were clear.
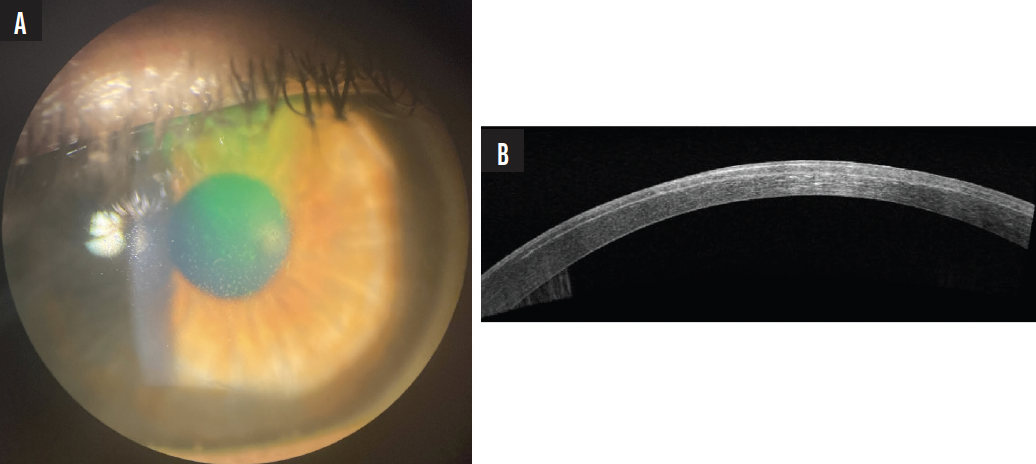
Figure 3. A slit-lamp photograph of the right eye 1 day after SMILE shows epithelial clusters in the central cornea (A). AS-OCT shows epithelial hyperreflectivity but a clear interface (B).
The patient underwent a limited superficial keratectomy (SK) on postoperative day 1 to remove all irregular epithelium from the central visual axis in the right eye. At the 3-day and 1-week visits, an improvement in the epithelial surface and some epithelial hyperplasia were noted; the latter was attributed to slow epithelial healing (Figure 4). The bandage contact lens was removed at week 1. Her UCVA was 20/50 OD at both visits.
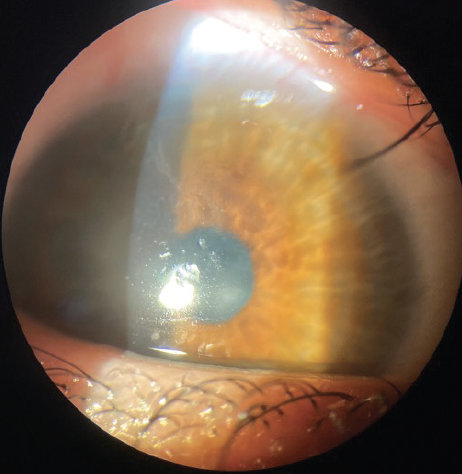
Figure 4. A slit-lamp photograph of the right eye taken 1 week after SK demonstrates irregular epithelial healing.
The patient returned 2.5 weeks after the keratectomy procedure with a distinct superonasal island of epithelial cells in the SMILE cap interface and overlying epithelial thickening in the right eye (Figure 5). Her UCVA was 20/40 OD. A refraction of +2.25 -3.25 x 51º failed to improve her visual acuity. Topography showed distinctive corneal flattening from the abnormal interface opacities in the superonasal area, and hyperreflectivity was observed in this area on anterior segment OCT (AS-OCT).
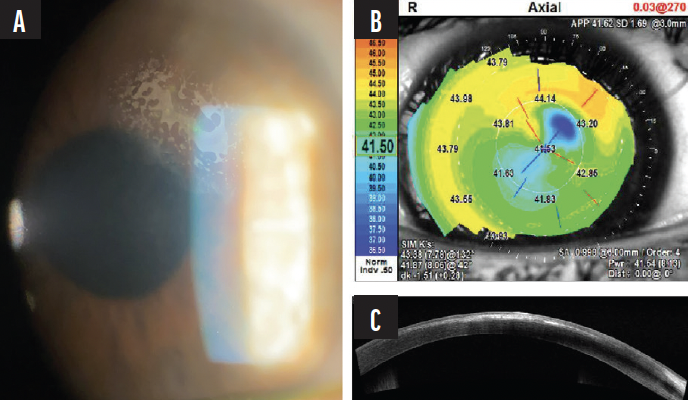
Figure 5. A slit-lamp photograph of the right eye 2.5 weeks after SMILE and a limited SK shows a distinct superonasal island of epithelial cells in the SMILE cap interface and overlying epithelial thickening (A). AS-OCT confirms abnormal hyperreflective opacities in the interface and hyperreflectivity of the thickened, overlying epithelium (B). Topography demonstrates flattening in the location of the irregular superonasal corneal opacities (C).
What do you believe occurred in this case? What are the patient’s options for visual rehabilitation, and how would you proceed?
—Case prepared by Nandini Venkateswaran, MD

JOHN F. DOANE, MD, FACS
SMILE interface epithelial ingrowth almost universally leads to a significant decrease in quality and quantity of vision. Removal of the ingrowth can produce a dramatic and quick improvement in vision. Patients may not notice epithelial ingrowth into a LASIK interface or flap whereas those who develop epithelial ingrowth after SMILE typically report symptoms within 1 to 4 days after surgery (Figure 6).
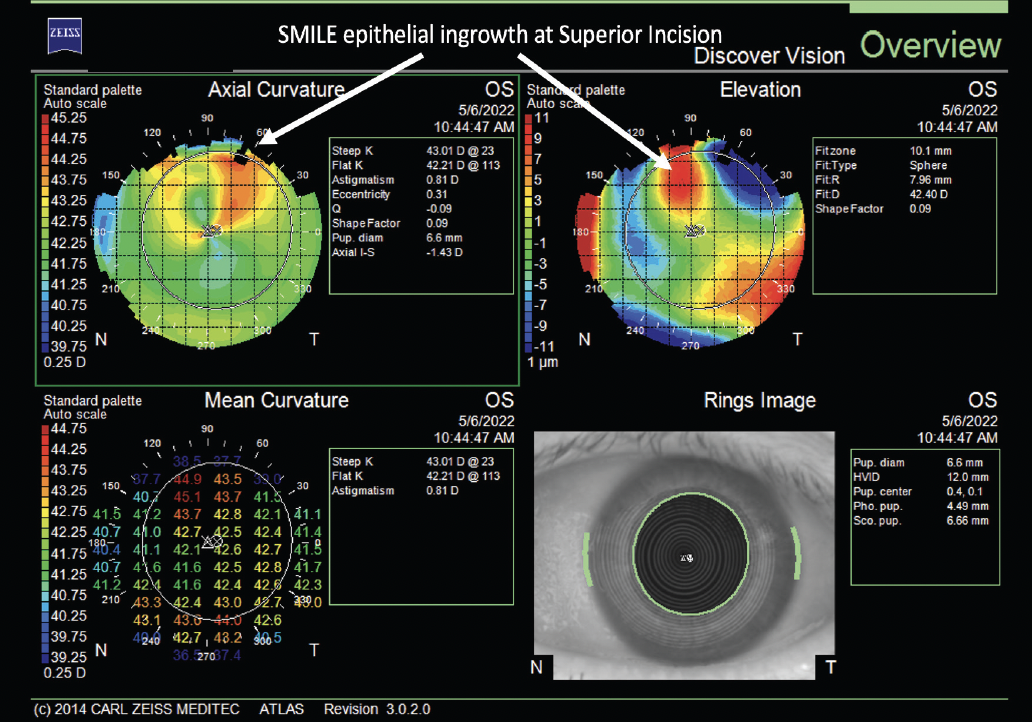
Figure 6. Typical presentation of epithelial ingrowth at the superior SMILE incision. The appearance in the axial curvature map (top left) resembles the crab claw indicative of pellucid marginal degeneration but in miniature. The red spot seen on the elevation map (top right) shows where epithelial ingrowth is elevating the SMILE flap.
Courtesy of John F. Doane, MD, FACS
Based on the case description, it appears that epithelial adherence was not strong in either eye. This and a frank epithelial abrasion were risk factors for interface epithelial ingrowth.
The interface epithelial cells can be removed completely at the slit lamp. Visualization here is better than under a laser in situations like this, but either will work. The epithelial sheet can be freed with the tip of a Slade LASIK cannula and flushed out with balanced salt solution irrigation under direct observation. The patient should be observed. Ideally, the epithelial layer will heal to provide a smooth optical surface. If not, an SK with or without anterior stromal puncture may be considered. The need for the latter intervention should be evident within 4 to 8 weeks.

WILLIAM F. WILEY, MD
Epithelial cells within the LASIK or SMILE interface pose a challenge, but I find the situation rarely occurs after primary procedures. Ingrowth is seen most often after a LASIK enhancement. After SMILE, epithelial cells seldom present as ingrowth but occasionally form a nest or island secondary to a retained piece of epithelium that was deposited during the primary procedure. Risk factors include the presence of a small epithelial defect near the edge of the SMILE incision and the inadvertent pushing of a piece of epithelium into the pocket during lenticule dissection. Anything pushed into the pocket may become trapped there.
Given that the interface appeared clean on postoperative day 1, a retained piece of epithelium might not have been an inciting factor in the current case. Perhaps the incision opened just enough during the SK for true epithelial ingrowth (vs a nest of retained epithelial cells) to occur.
Regardless of the etiology, I would wash the pocket carefully to remove all the epithelial cells and confirm that the incision is watertight (ie, no large gap or gutter). The incision could be sutured to help prevent recurrent ingrowth. After epithelial removal, the area would be monitored closely for 3 to 4 days. If epithelial cells are again observed in the area, treatment of the interface with an Nd:YAG laser would be considered before proliferation of the cells renders the option ineffective.

WHAT I DID: NANDINI VENKATESWARAN, MD
I suspect the patient had subclinical anterior basement membrane dystrophy that revealed itself during the SMILE procedure. In retrospect, the preoperative examination of the epithelial thickness maps showed mild hyperplasia in the right eye, which might have hinted at anterior basement membrane dystrophy. The epithelium was fragile and sloughed off easily after the interface of the VisuMax laser (Carl Zeiss Meditec) touched the corneal surface during surgery. This initiated a cascade of poor epithelial healing.
The right eye’s appearance on postoperative day 1 was suggestive of irregular epithelial healing. At 2.5 weeks, the epithelial surface continued to be irregular, and epithelial cells had proliferated into the SMILE cap interface. It is possible that some epithelial cells were introduced into the interface during lenticule dissection and proliferated during the following 2 to 3 weeks. Alternatively, a small fistula for epithelial cell migration might have been created after the SK was performed on postoperative day 1. Additional stromal puncture or diamond burr polishing at the time of the SK might have assisted with epithelial healing.
Epithelial opacities were detected in the SMILE cap interface, and the patient was taken back to the laser suite. The superior incision was reopened with a Sinskey hook. A Malosa spatula (BVI Medical) was used in a circumferential fashion to liberate the epithelial nests from the underside of the cap (watch the video below). Care was taken to avoid pushing the epithelial cells farther into the interface. A LASIK flap lifter with a hinged tip was used to scrape the underside of the cap similarly to how Descemet membrane would be stripped during an endothelial keratoplasty. A thick sheet of epithelium was then gently removed in one piece through the main incision with jeweler’s forceps. If I had been unable to remove the epithelium in the manner described, my backup plan was to extend the superior incision and reflect the SMILE cap to expose the area of epithelial cell growth better.
A cannula with balanced salt solution was used to irrigate the interface. ReSure Sealant (Ocular Therapeutix) was administered to close the superior incision and prevent epithelial cells from entering the interface. Another option would have been to close the incision with 10-0 nylon sutures. A 16-mm bandage contact lens (Kontur Kontact Lens) was placed, and collagen punctal plugs were inserted in the upper and lower puncta. The patient was instructed to lubricate the eye generously, administer topical steroid and antibiotic drops for 2 weeks, and wear moisture goggles at night.
The bandage contact lens and ReSure Sealant were removed 1 week after the procedure. Two weeks after epithelial removal, the patient’s UCVA was 20/20 OD. There was no residual interface haze or scarring, and the patient was pleased with her outcome (Figure 7). The fellow eye remained stable.
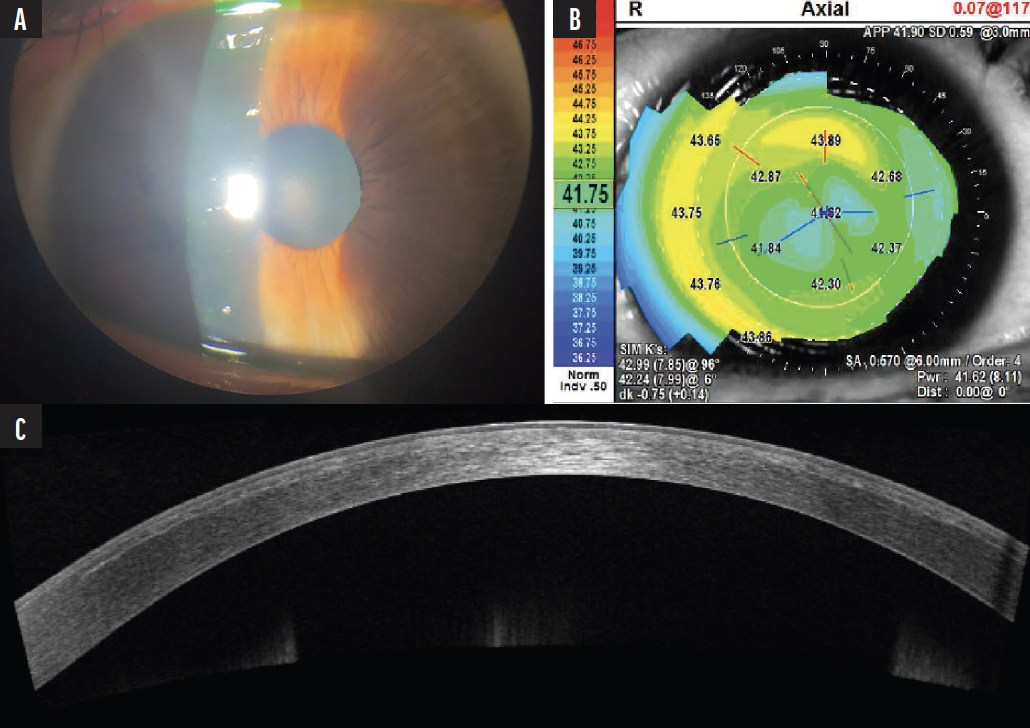
Figure 7. A slit-lamp photograph of the right eye 2 weeks after the interface washout procedure. There is no residual corneal haze (A). Topography has normalized and shows central flattening consistent with a myopic treatment (B). AS-OCT shows resolution of epithelial and interface irregularities (C). The patient’s UCVA returned to 20/20 OD.
Courtesy of Nandini Venkateswaran, MD




