Refractive surgery provides patients with the chance to reduce or eliminate their reliance on glasses and contact lenses. LASIK, PRK, and laser-assisted lenticule extraction (LALE), however, are not universally applicable. For example, the efficacy of LASIK for the treatment of individuals with emmetropic presbyopia and young patients with more than 3.00 D of hyperopia is limited. Attempts to induce central corneal steepening can result in epithelial hyperplasia and suboptimal results. Furthermore, patients with a short axial length and shallow anterior chamber may be poor candidates for LALE. In keratoconic eyes, the inherent weakness of the cornea combined with the removal of corneal tissue during laser procedures can aggravate the condition.
Tissue addition technology is a promising alternative to treatments such as LASIK, PRK, and LALE that remove tissue. Tissue addition strengthens the corneal structure through the addition of allograft material. The technology expands the capabilities of refractive surgery by addressing challenges such as emmetropic presbyopia and pronounced hyperopia in young patients. It opens new avenues for the treatment of keratoconus.
Technological Advances
E-beam sterilization. The sterilization process for corneal tissue has been significantly improved by e-beam sterilization. This pivotal breakthrough extends tissue preservation for up to 2 years by eradicating microbial contamination while maintaining the tissue’s structure. E-beam sterilization enhances both the logistics of transplantation and standards of safety and quality.
Excimer laser lenticule shaping. With excimer lasers, corneal lenticules can be precisely shaped to meet individual refractive needs, enhancing the success of tissue addition procedures (Figure 1).
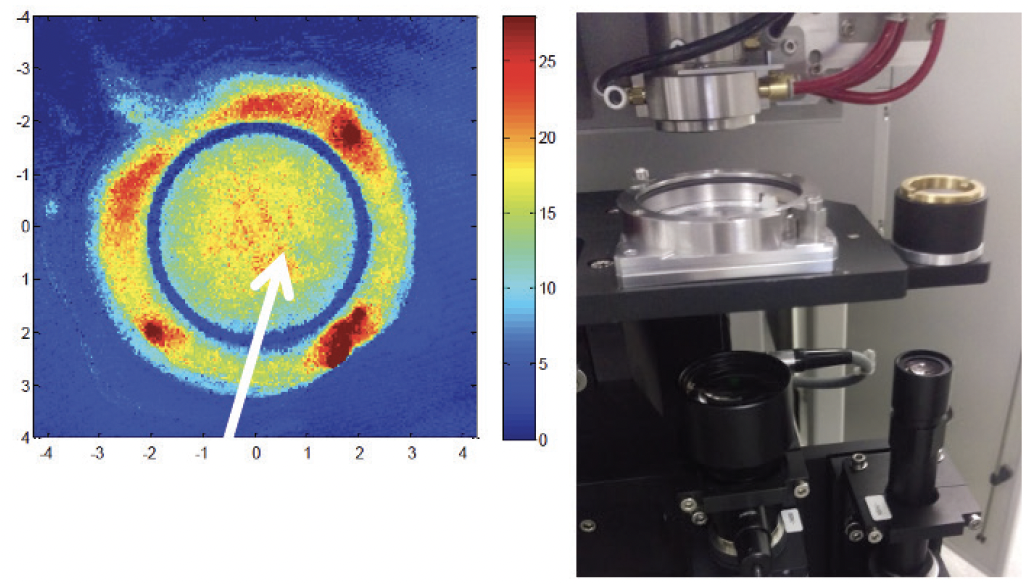
Figure 1. Topographic representation of a laser-shaped corneal lenticule (left) and the excimer laser equipment used for the procedure (right).
Innovations in lenticule use. The cryopreservation of lenticules from LALE for future use opens up new possibilities for the treatment of various corneal conditions.
OCT-enhanced lenticule fabrication. The integration of advanced OCT in lenticule production helps ensure that each is meticulously crafted to meet stringent quality criteria, tailored for its surgical purpose.
Treatment Applications
Bridging the presbyopia gap. The use of bio-analog corneal inlays integrated with allograft tissue is an innovative approach to presbyopia treatment that moves beyond traditional corneal reshaping techniques such as LASIK, PRK, and LALE. The corneal surface is reengineered to improve depth of focus and provide clear vision at various distances.
Allogeneic corneal lenticules are placed either beneath a LASIK flap or within a corneal pocket. Corneal stromal thickness is preserved—a vital advantage over conventional refractive surgeries that remove corneal tissue. The adaptability of the inlay implantation process, including the potential for adjustment or removal, aligns well with the progressive nature of presbyopia and accommodates possible cataract development.
Clinical findings to date have shown that tissue addition technology can improve patients’ near vision substantially, sometimes by an average of 5 lines in emmetropic presbyopic patients, without significantly altering their preoperative distance vision. Patients have benefitted from excellent binocular UCVA at distance, intermediate (70 cm), and near (40 cm); rapid visual recovery; and minimal postoperative discomfort.1 Their experiences are similar to after LASIK and LALE (Figure 2).
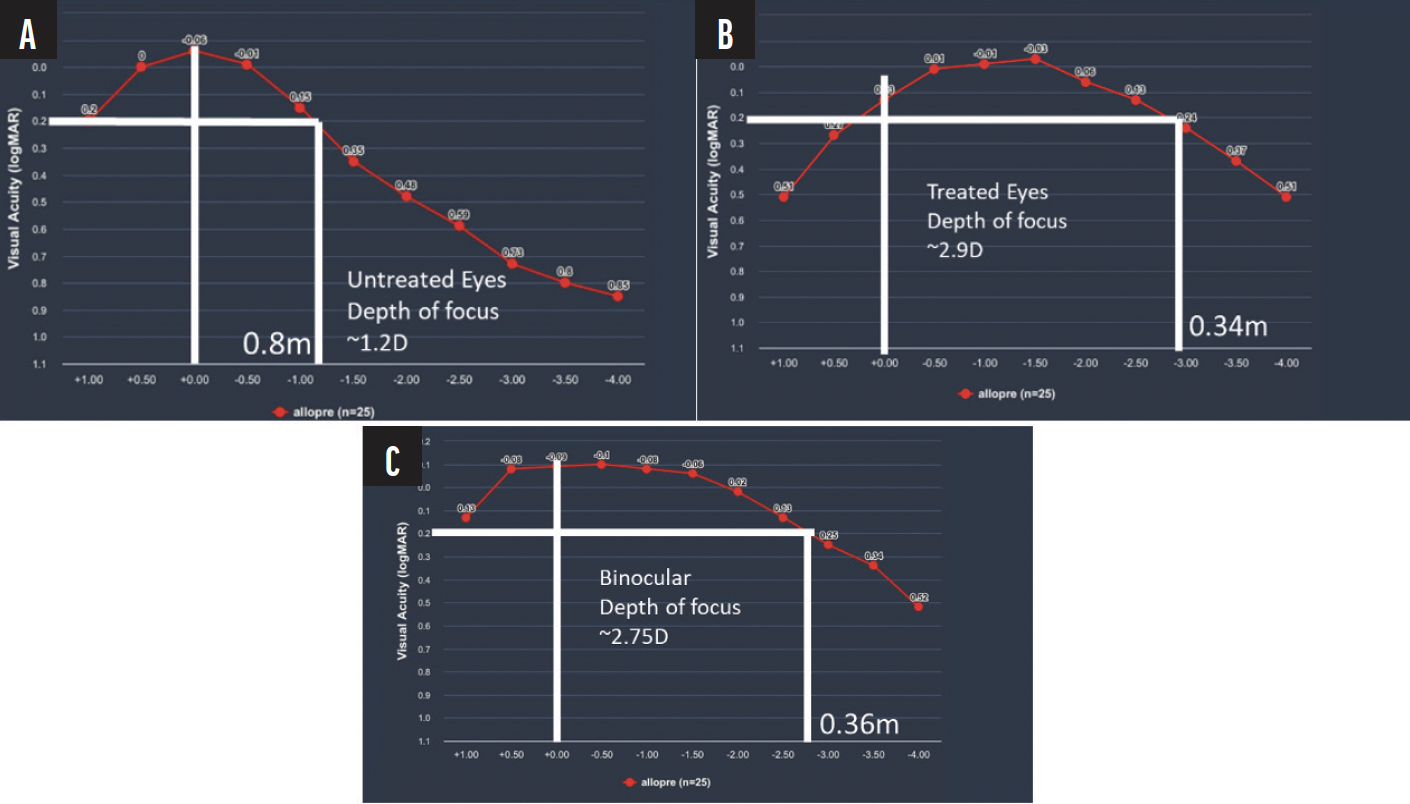
Figure 2. Defocus curves for untreated (A), treated (B), and binocular (C) vision show improvements in patients’ depth of focus and visual acuity postoperatively.
Addressing hyperopia in young adults. Corneal inlays may be a useful option for the correction of hyperopia, especially among young adults. The procedure is less invasive than traditional laser surgery. The inlays are strategically placed in the corneal stroma, either beneath a LASIK flap or into a corneal pocket. Corneal power within a 6- to 7-mm optical zone is enhanced, eliminating the need for a clinically significant transition zone. This makes the approach particularly suitable for young adults who retain a strong accommodative ability.
Preliminary research indicates that the technique improves patients’ visual acuity at near and distance with a notable degree of predictability and stability.2 The reversibility of inlay implantation allows future removal or enhancement with an excimer laser if needed. This is a crucial consideration in young adults who may be reluctant to undergo irreversible laser procedures.
A further advantage of corneal inlays over traditional tissue-removal surgeries is the former’s minimal effect on epithelial remodeling. Tissue removal can lead to unpredictable refractive outcomes or corneal irregularities due to the epithelium’s compensatory thickening or thinning. Inlays, in contrast, do not significantly alter the corneal epithelium. This limits postoperative complications and enhances the reliability of the results.
Advancing refractive surgery for keratoconus. Corneal allografts, particularly corneal allograft intrastromal ring segments (CAIRS) and precision-shaped lenticules, are an emerging treatment for keratoconus. CAIRS are implanted in the cornea to provide structural support and mitigate the conical protrusion characteristic of keratoconus (Figure 3). The method holds promise for enhancing corneal topography and patients’ visual acuity,3 and CAIRS implantation may postpone or negate their need for a corneal transplant.
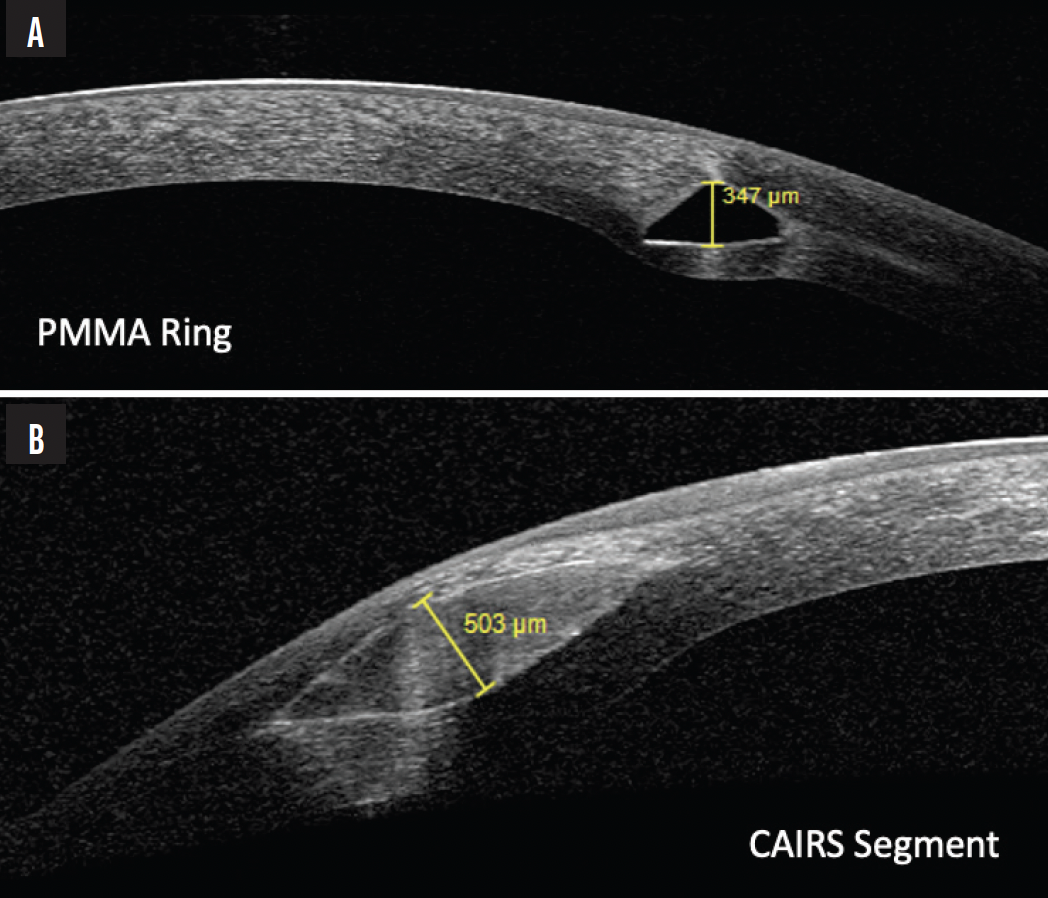
Figure 3. OCT images comparing a PMMA ring segment (A) with a thickness of 347 µm and CAIRS (B) measuring 503 µm.
Customized corneal lenticules are another therapeutic strategy. These lenticules are crafted to match each patient’s specific corneal shape. They can be used to increase corneal thickness and adjust corneal curvature to address irregular astigmatism due to keratoconus. The technique can fortify the cornea and correct the refractive anomalies inherent to the condition.
Additional Considerations
Availability of corneal tissue. The availability of corneal tissue is a major concern. The demand for complete corneas remains high, driven by traditional transplants, but the supply often falls short owing to a limited donor pool and logistical hurdles. The shortage has spurred the search for alternative sources and methods of transplantation. Human corneal donor stroma is an accessible option, especially because it can be derived from corneas that are unsuitable for full transplantation because of endothelial damage.
Maximizing donor tissue utility is another vital strategy. One donor cornea can supply stromal tissue for multiple recipients, optimizing the use of each donation for therapeutic procedures and addressing a shortfall in full donor corneas (Figure 4).
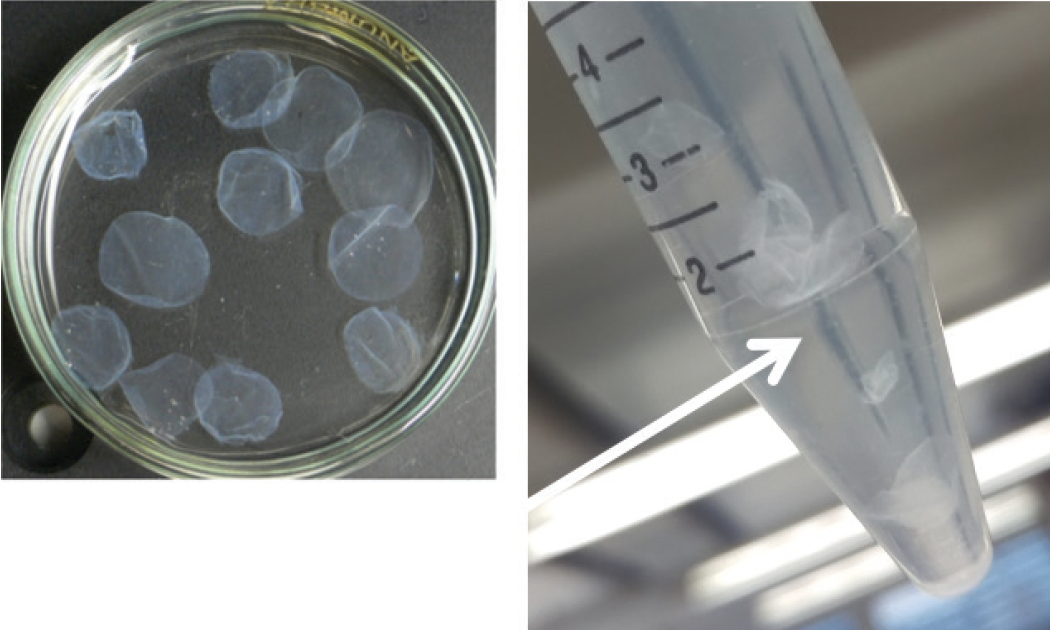
Figure 4. Corneal tissue for transplantation prepared from a single donor cornea.
Flap or pocket. Corneal lenticules are implanted either under a flap or within a pocket. Flap creation is associated with well-known risks but may offer greater biomechanical stability, and it allows for combined treatments. Pocket implantation is less invasive and may therefore reduce the incidence of postoperative dry eye disease. This approach, however, may introduce greater variability in outcomes.
Legal and regulatory considerations. The utilization of lenticules faces a complex legal and regulatory landscape for corneal transplantation. These include rigorous testing for infectious diseases and meticulous donor tracking to ensure patient safety. Although these regulations are indispensable, they pose practical challenges to the therapeutic and refractive use of corneal lenticules, potentially increasing costs and complicating their application.
Xenografts. The exploration of xenografts, such as porcine corneal tissue, is driven by misconceptions about the scarcity of stromal tissue. Although xenografts represent a potential supplement, they introduce complexities related to immunologic compatibility. Extensive processing is also required to approximate human tissue properties.
1. Nur Keskin Perk FF, Taneri S, Tanriverdi C , Haciagaoglu S, Karaca ZY, Kilic A. Increasing depth of focus with allogeneic presbyopic inlays: 3-year results. J Cataract Refract Surg. 49(10):1005-1010.
2. Tanriverdi C, Ozpinar A, Haciagaoglu S, Kilic A. Sterile excimer laser shaped allograft corneal inlay for hyperopia: one-year clinical results in 28 eyes. Curr Eye Res. 2021;46(5):630-637.
3. Haciagaoglu S, Tanriverdi C, Keskin FFN, Tran KD, Kilic A. Allograft corneal ring segment for keratoconus management: Istanbul nomogram clinical results. Eur J Ophthalmol. 2022:11206721221142995.