Several options for refractive correction are currently available to patients with presbyopia who have clear crystalline lenses, all aimed at enhancing depth of focus. These include laser keratorefractive surgery, such as LASIK, laser-assisted lenticule extraction, PRK, and laser epithelial keratomileusis. These procedures can provide monovision to emmetropic presbyopic individuals; typically hyperopic ablation is performed on the nondominant eye to achieve a near vision target.1 Alternatively, laser ablation is performed to create blended or multifocal corneal curvatures bilaterally. A limitation of all these procedures in phakic presbyopic patients is their inability to adapt to the refractive changes that occur with age, as the crystalline lens stiffens and its continual growth alters the eye’s refraction.
The Beaver Dam Eye Study found that phakic individuals with early presbyopia (43–59 years of age) became more hyperopic on average, those with medium presbyopia (60–69 years of age) showed little variation on average, and those with late presbyopia (≥ 70 years of age) tended to become more myopic.2 The unpredictability of the refractive shift in presbyopic patients has been documented in a number of studies.3 Generally, the shift averages less than 0.50 D, but individual variations can be substantial, leading patients to complain of blurry vision. Spectacle and contact lens wear can address the change in refraction. For patients who are intolerant of contact lenses and choose not to wear glasses, however, there is an unmet need for a minimally invasive, reversible, and repeatable corneal procedure with no adverse effects that does not induce ocular aberrations. The evolution of thermal applications to shape the cornea may provide a solution.
THERMAL SYSTEMS FOR CENTRAL CORNEAL STEEPENING
Both Holmium:YAG laser thermokeratoplasty (LTK) and conductive keratoplasty (CK) modify the corneal structure but with different methodologies. LTK involves altering the structural collagen in a perilimbal circular fashion.4 In CK, a radial array of thermal spots is placed, resulting in a circular constriction in the stroma that causes central corneal steepening.5,6 Although the FDA approved both LTK and CK in 2000 and 2002, respectively, for the temporary reduction of hyperopia, neither procedure was widely adopted for various reasons. Both can induce irregular astigmatism in a subset of cases, patients experience pain after surgery, and postoperative visual recovery times are relatively long. The effect of treatment, moreover, is temporary, and the procedures are not repeatable.
That said, CK is still performed by some ophthalmologists to improve corneal shape in keratoconic eyes.7
OPTIMAL KERATOPLASTY
The VIS Optimal Keratoplasty System (Opti-K, VIS) is a thulium fiber infrared laser–based system that has been in use for more than 10 years in Europe, the Bahamas, and limited US clinical trials. Treatment with the Opti-K is indicated for the temporary improvement of distance and near visual acuity in patients with hyperopia and presbyopia. The process involves directing 16 0.5-mm spots of thulium laser to the midperipheral cornea via a fiber optic bundle (Figure 1A). To protect the epithelium from thermal damage, a sapphire plate is applied to the epithelium. These treatment spots fade over time (Figure 1B). The procedure is repeatable and noninvasive (there are no epithelial lesions).

Figure 1. Opti-K features. Pattern of spots on the cornea. Scale: 0.5-mm intervals (A). Immediately after treatment (B). Same eye 1 week after treatment (C).
A 6-month European trial demonstrated that patients with low to moderate hyperopia and presbyopia who underwent treatment with the Opti-K System experienced an improvement in their uncorrected near visual acuity (UNVA), while their uncorrected distance visual acuity (UDVA) improved or remained the same.8
The safety and effectiveness of the Opti-K System has been studied in several US settings, including in three feasibility trials. In the first of these, hyperopic presbyopic patients received optimal keratoplasty treatments in one eye. On average, patients who underwent only one treatment had a UDVA of 20/32 at 2 years—an improvement of 2.5 lines. In a continuation of this trial, hyperopic patients were treated in only one eye and achieved 3 lines of improvement (20/15 UDVA) at 1 year (unpublished data on file with VIS, 2010 and 2016).
In a subsequent monovision feasibility trial, the nondominant eye of presbyopic patients who were emmetropic or had low hyperopia achieved a more transient improvement in UNVA. An analysis showed that, when treatment targeted near vision in a phakic presbyopic eye, the improvement resulted from both a myopic shift and an increase in negative spherical aberration (central steepening) without the induction of astigmatism or coma in the treated eye (unpublished data on file with VIS, 2021).
No treatment-related serious adverse events have been reported in any of the preliminary studies conducted within or outside the United States. Optimal keratoplasty provided a temporary (3 months–2 years or more) improvement in vision. Figure 2 provides an example of a patient who received 10 Opti-K treatments over 5 years. This temporary effect, instead of being a drawback, offers phakic presbyopic patients the opportunity to adapt to a variable refractive shift.
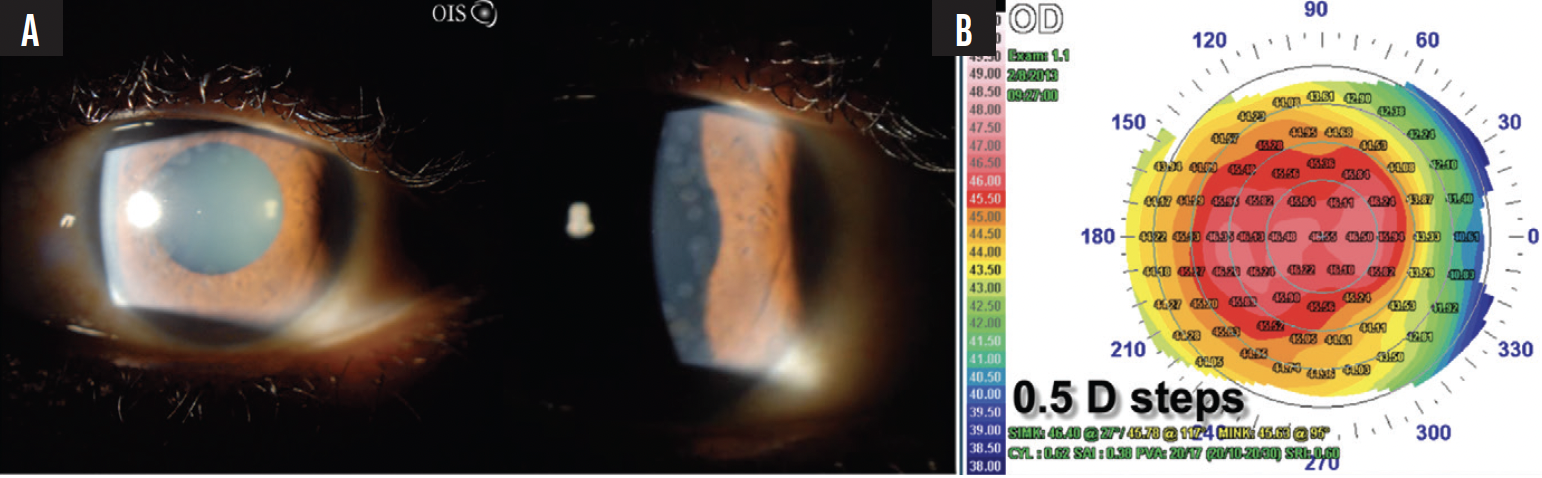
Figure 2. The eye has undergone 10 Opti-K treatments, shown with sclerotic scatter (A). High-resolution corneal topography shows the central steepening characteristic of the treatment (B).
COMPARISON OF THERMAL KERATOPLASTY SYSTEMS
Much effort and time have been devoted to developing a reliable method for steepening the cornea through the application of heat to condense stroma in a perilimbal band. As mentioned earlier, both LTK and CK received FDA approval but are not without adverse effects (Table). For instance, the induction of astigmatism and higher-order aberrations can reduce the patient’s visual acuity. Additionally, the options for retreatment are limited, and patients experience treatment regression over time.
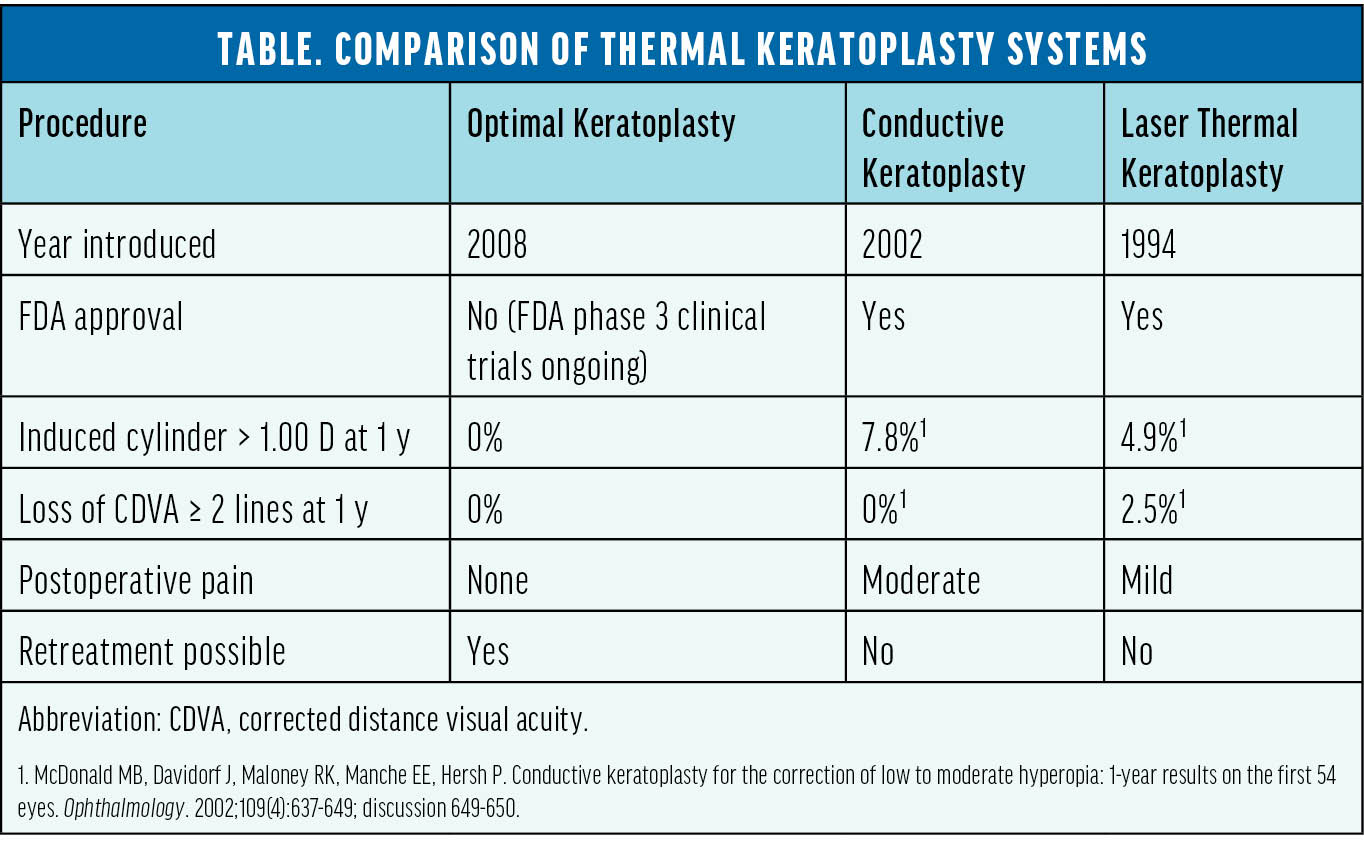
In contrast, although the effects of optical keratoplasty can also be transient, treatment can be repeated multiple times as needed. The procedure is also reversible, and it can address variations in refraction that occur in a phakic presbyopic eye as it ages.
Patients’ attitudes toward temporary ophthalmic procedures have changed since the first thermal keratoplasty procedures were developed. For example, many have embraced the injection of cosmetic neurotoxins and dermal fillers, the effects of which regress over time. Similarly, temporary procedures for the treatment of ocular surface disease such as microblepharoexfoliation and thermal pulsation therapy have also become popular. Perhaps thermal keratoplasty’s time has finally come.
1. Katz JA, Karpecki PM, Dorca A, et al. Presbyopia – a review of current treatment options and emerging therapies. Clin Ophthalmol. 2021;15:2167-2178.
2. Lee KE, Klein BE, Klein R, Wong TY. Changes in refraction over 10 years in an adult population: the Beaver Dam Eye Study. Invest Ophthalmol Vis Sci. 2002;43(8):2566-2571.
3. Grosvenor T, Skeates PD. Is there a hyperopic shift in myopic eyes during the presbyopic years? Clin Exp Optom. 1999;82(6):236-243.
4. Durrie DS, Schumer DJ, Cavanaugh TB. Holmium:YAG laser thermokeratoplasty for hyperopia. J Refract Corneal Surg. 1994;10(2 suppl):S277-280.
5. McDonald MB, Hersh PS, Manche EE, Maloney RK, Davidorf J, Sabry M; Conductive Keratoplasty United States Investigators Group. Conductive keratoplasty for the correction of low to moderate hyperopia: U.S. clinical trial 1-year results on 355 eyes. Ophthalmology. 2002;109(11):1978-1989.
6. Hersh PS. Optics of conductive keratoplasty: implications for presbyopia management. Trans Am Ophthalmol Soc. 2005;103:412-456.
7. Sinjab MM, Rubinfeld RS, Wagner K, Parsons Jnr EC, Cummings AB, Belin MW. Outcomes of conductive keratoplasty combined with corneal crosslinking in advanced ectatic corneal disease. Clin Ophthalmol. 2021;15:1317-1329.
8. Veritti D, Sarao V, Lanzetta P. Optimal keratoplasty for the correction of presbyopia and hypermetropia. J Ophthalmol. 2017;2017:7545687.