The rotational stability of a toric IOL is crucial to a successful outcome. For the best visual acuity results, the IOL should be placed and remain within 5º of the axis of astigmatism. Postoperative IOL misalignment is commonly due to errors in preoperative biometry and marking—important topics that are not addressed in this article. Assuming the surgeon places the IOL correctly, why is there any rotation at all?
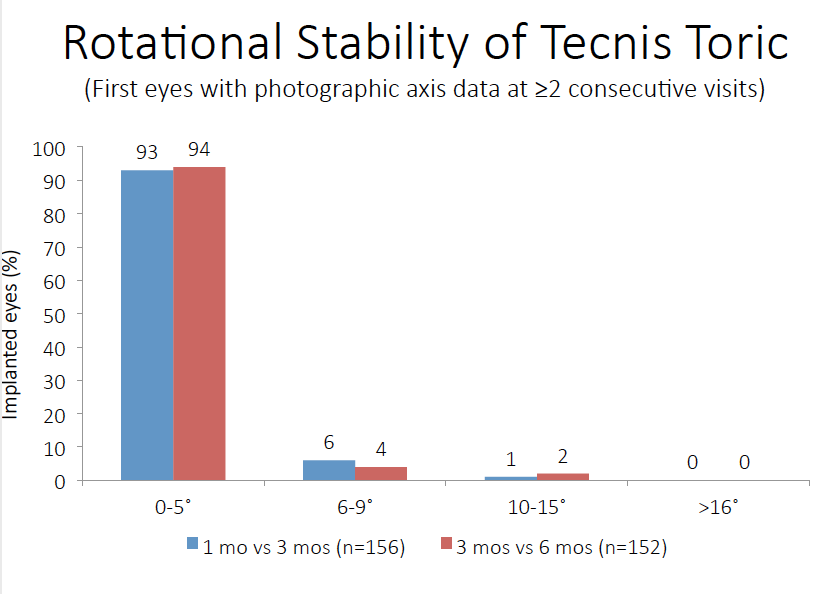
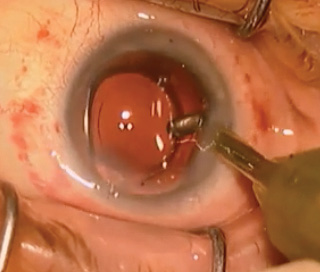
Figure. Excellent stability has been reported for the Tecnis Toric IOL. Surgeons can further maximize stability by following the techniques described in this article.
The exact mechanism for toric lens rotation is not well understood. The lens is confined within the bag where there is no bulk fluid flow or other internal force vectors after surgery. Rotation is therefore likely due to external forces applied to the eye. If an eye were hypotonous, forceful blinking, eye rubbing, or the pressure of a dropper bottle could transmit a force to the IOL. Compressing a hypotonous eye is therefore likely the primary mechanism for toric IOL rotation. Gross deformation of the globe could cause a shift in the IOL’s position.
After implanting more than 300 Tecnis Toric IOLs (Abbott), I have only had to reposition one. This is due in part to the excellent stability of the lens itself. In clinical trials, it had a mean axial change of just 2.74º between baseline and 6 months. More than 90% of the lenses rotated 5º or less between visits 3 months apart (Figure). Good surgical technique is key. Here are four steps for ensuring that a toric IOL is properly aligned for optimal results.
Be Meticulous About Wound Construction
Whether using a femtosecond laser or a blade, construct a triplanar incision that will seal well at the end of the case. It should be nearly square and long enough for good wound closure.
Create a Well-Centered Capsulotomy
A full 360º of capsular overlap may help to limit asymmetric capsular forces on the IOL postoperatively.
Position the IOL Correctly in a Clean Capsule
IOL implantation should be done with a cohesive viscoelastic for easy and complete removal at the end of the case. As the lens unfolds, I rotate it in the bag several times and perform aspiration behind the IOL. This process helps to clear out retained viscoelastic and cortical debris. It also ensures that the haptics are fully deployed into the capsular fornix. Once the haptics have unfolded completely, I center the IOL by having the patient fixate on a coaxial light source. Then, I align the marks on the IOL with the corneal axial marks on the steep meridian. The IOL need not align perfectly with these axial marks. As long as it is parallel to the marks, it is more important to center the IOL well.
Ensure a Tightly Sealed Wound
I hydrate the wound to seal it and bring the eye to physiologic pressure, while being careful not to under- or hyperinflate it. With the chamber stable, I can fine-tune the lens’ position before finally rehydrating and checking the wounds and the IOL’s position one last time. When checking the wound, I dry it to find slow leaks and press on the globe to simulate an eye rub. When in doubt, I suture the wound or consider a sealant.
CONCLUSION
Postoperatively, I instruct patients not to rub their eyes. I try to minimize the dosing regimen of postoperative drops with combination products or dropless surgery. This reduces the chance that patients will rub their eyes or poke them with the bottle, which I suspect is a common occurrence.
With these steps (see Watch It Now), surgeons can be confident that their toric IOLs will remain stable to successfully correct astigmatism in refractive cataract patients.