
We all have patients in our practices who might benefit from laser vision correction (LVC) but who are difficult to treat because of irregular astigmatism, aberrated corneas, or complications from prior surgery. In some cases, we could approach these patients with a topography-guided treatment, but my preference is a wavefront-guided treatment that has the potential to correct both the surface irregularities and the refractive error.
AT A GLANCE
• The iDesign advanced wavefront aberrometer may be able to capture and treat more highly aberrated eyes in addition to performing well in routine cases. The device collects more data points and can capture a smaller pupil and a wider dynamic range than its predecessor.
• Recently, the author treated four patients with complex eyes using iDesign-guided surface treatments (off label) and achieved excellent results.
• Advanced aberrometry has advantages beyond complex eyes, and it is particularly accurate at measuring and treating astigmatism.
The iDesign advanced wavefront aberrometer (Abbott) may be able to capture and treat these more highly aberrated eyes in addition to performing well in routine cases. The device collects more data points and can capture a smaller pupil and a wider dynamic range than its predecessor, the WaveScan (Abbott). The former also incorporates multiple measurements into a single device. Recently, I treated four patients with complex eyes using iDesign-guided surface treatments. I should note that surface treatments and retreatments are off label with many of the modern-day laser systems, including the iDesign.
COMPLEX EYES
Case No. 1
The eye had undergone PRK 6 months previously to correct very high astigmatism. Pre-enhancement, the patient’s refraction was -2.50 +2.25 × 054, correctible only to 20/40-. The total higher-order aberration root mean square (RMS) error was 0.68 µm. I treated this eye based on an iDesign wavefront refraction of -2.28 +1.96 × 61. Three months after the enhancement, the UCVA was 20/25, and the manifest refraction was +0.50 D sphere. This eye also had mild amblyopia that will limit the patient’s vision to some degree.
Case No. 2
The patient was an unhappy 78-year-old man who had undergone cataract surgery and an Nd:YAG capsulotomy elsewhere. Although the IOL was well centered, and the patient’s visual acuity corrected to nearly 20/20, there was a fibrotic scar—possibly from wound burn—and what appeared to be an unusually anterior entry, causing irregular astigmatism that can be seen on wavefront and topographic maps (Figure 1). The patient also had mild epithelial basement membrane dystrophy. Because of the scar and irregular astigmatism, the patient was experiencing a large amount of ghosting and shadowing. Prior to laser enhancement, the manifest refraction was -1.50 +2.00 × 160. I performed a phototherapeutic keratectomy (PTK) based on an iDesign wavefront measurement of -1.55 +1.51 × 164. Three months later, the UCVA was 20/20, and the patient was very happy with the improvement in quality of vision.
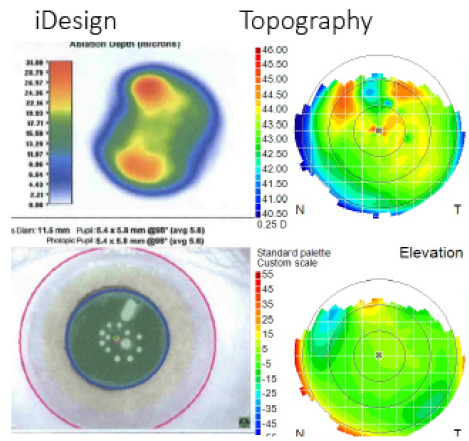
Figure 1. The surgeon performed iDesign-guided PTK on an eye with irregular astigmatism and corneal scarring after cataract surgery.
Case No. 3
A 56-year-old woman had undergone a deep anterior lamellar keratoplasty several years previously, following a bout of Acanthamoeba keratitis. She had a deep anterior lamellar keratoplasty with some anterior scarring, and the graft was 9 mm in diameter, and she had significant irregular astigmatism. She subsequently underwent cataract surgery and an Nd:YAG capsulotomy. At this point, her refraction was -5.00 +3.0 × 003 and, with a 0.75 µm RMS error, corrected to 20/40-. I performed an iDesign-guided PTK. Just 1 month postoperatively, she had an UCVA of 20/30. She had some refractive astigmatism, but that will likely improve as the epithelium, which was still a little rough, continues to heal.
Case No. 4
A 63-year-old man had a history of LASIK using a small optical zone and subsequent IOL implantation with astigmatic keratotomy incisions and an Nd:YAG capsulotomy. The cornea was highly oblate (Figure 2), and the small optical zone, the edges of the capsulorhexis, and the Nd:YAG capsulotomy made it more difficult for me to capture a wide-zone aberrometry measurement with the WaveScan. Having an aberrometer that could capture the pupil at 4 mm made it possible for me to perform a PRK enhancement in this eye to treat the iDesign wavefront measurement summarized by -1.92 +1.89 × 98 (with an RMS error of 0.8 µm ). Four months postoperatively, the patient’s UCVA was 20/20, and he had some mild dry eye disease.
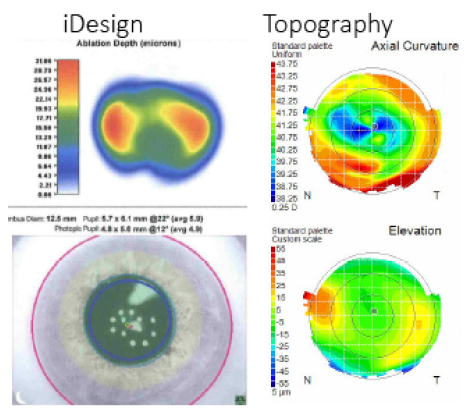
Figure 2. In an oblate cornea with a small optical zone and a history of several surgical procedures, having an aberrometer that could capture a measurement at 4 mm made it possible for the surgeon to perform a PRK enhancement.
Summary
All of these patients desired improved functional vision with and without correction. In each case, irregular astigmatism and other corneal issues would have made it difficult to capture a wavefront measurement with earlier aberrometers and impossible to use a conventional procedure. In these complex scenarios, I would not expect a perfect match between the manifest and wavefront refractions or a perfect outcome, yet the iDesign allowed me to plan and execute a treatment that greatly improved the patients’ quality of vision and UCVA.
ROUTINE CASES BENEFIT, TOO
Advanced aberrometry has advantages beyond complex eyes. The iDesign is particularly accurate at measuring and treating astigmatism, producing even better results than have been obtained in the past. In a large European analysis of more than 10,000 myopic eyes treated with the device, for example, 96.6% of eyes were within 0.50 D of emmetropia postoperatively, with 82% seeing 20/16 monocularly without glasses.1
Consistently obtaining results like these can certainly help a refractive surgery practice build word-of-mouth referrals. My colleagues’ and my practice has seen approximately a 5% increase in LVC procedures annually for the past 8 years. I credit that growth to a combination of persistence in the LVC market, greater LVC use for enhancements after refractive cataract surgery, and the use of the most advanced technology possible. The ability to treat a wider range of more highly aberrated eyes like those described herein is an added benefit.
1. Schallhorn S. Initial experience with an advanced wavefront guided system (iDesign). Presented at: ESCRS; May 2015; Barcelona, Spain.




