
An irregular cornea poses significant challenges for both biometry and cataract surgery. Such irregularities can be caused by scarring, prior refractive surgery, or ectasia. This article shares advice based on my experience.
PREOPERATIVE CONSIDERATIONS
Corneal epithelial mapping. In patients with keratoconus, corneal epithelial mapping that demonstrates significant remodeling and thinning over the cone provides strong evidence that the individual rubs their eyes, possibly even unconsciously during sleep. It is often easy to infer which eye makes contact with the pillow during sleep based on corneal epithelial maps. In these situations, I advise patients to wear a self-made mask that allows them to sleep comfortably while protecting the cornea. I make the recommendation regardless of the patient’s age because I have even seen significant eye rubbing destabilize the corneas in patients in their late 70s.
Total corneal power. Most IOL calculations rely on surface keratometry measurements. In an eye with an irregular cornea, the posterior corneal surface may not exhibit the classic -6.00 D of spherical power. It therefore becomes essential to consider the total corneal power.
I use the central 4.5 mm of total corneal power as measured by Scheimpflug tomography. For the IOL power calculation, I rely on the Hoffer Q formula if the axial length is less than 25 mm and the Holladay 1 formula if the axial length is 25 mm or greater. I have achieved good outcomes with this approach, even in ectatic eyes.
STAGED SURGERY
CXL followed by cataract surgery. When planning cataract surgery on an eye with significant decentralized ectasia, my first step is to address the keratoconus with CXL using the Athens protocol.1,2 My colleagues and I introduced this bimodal procedure nearly 2 decades ago,3 and many variations have since been developed (for a related article, see “CXL and Keratoconus Management,“ pg 85). In my experience, the Athens protocol can stabilize the cornea, normalize distorted corneal optics, and thereby improve the accuracy and predictability of biometry and IOL power calculations.
A staged approach may sound like a long path for patients, but I value its reliability. CXL combined with partial-refraction, topography-guided surface ablation with a therapeutic target can flatten the cornea by 3.00 to 15.00 D. Even after nearly 4,000 cases, I find it impossible to anticipate a patient’s refractive error following Athens protocol CXL. For this reason, I always perform Athens CXL before cataract surgery when needed.
Topography-guided laser ablation followed by cataract surgery. I also have experience with and recommend a staged approach for eyes with irregular corneas due to trauma, herpetic disease, infection, or prior refractive surgery. Topography-guided laser ablation has a robust ability to normalize these corneas.4,5 The procedure can improve the accuracy of keratometry readings and thus IOL power calculations. Laser treatment can also improve corneal optics.
IOL SELECTION
Toric lenses. A patient with an irregular cornea may thrive with a rigid gas permeable or scleral contact lens. If they are happy with their BCVA and wish to continue using either modality, implanting a toric IOL could complicate matters. They would have to wear spectacles that neutralize the IOL’s toricity to wear either rigid gas permeable or scleral contact lens.
Multifocal and extended depth of focus lenses. These IOLs are designed for eyes with impeccable corneal optics. For this reason, I do not recommend either to patients who have severely irregular corneas, even when CXL and/or topography-guided laser ablation is planned.
CONCLUSION
Irregular corneas once mandated lamellar or penetrating keratoplasty. Advances in the customization of corneal excimer ablation, however, have revolutionized the treatment paradigm for these eyes. Today, we can reshape a cornea that was once considered incurable without a specialized contact lens. Normalizing these corneas with a customized ablation can bring them to a state in which traditional biometry may be used to address refractive error accurately at the time of cataract surgery.
CASE STUDIES
Case No. 1
A 64-year-old man with keratoconus presented for a cataract surgery evaluation (Figure 1). An obstetrician by trade, he wore rigid gas permeable contact lenses but developed severe intolerance and expressed a strong desire to discontinue their use.

Figure 1. Placido disc reflection topography shows how the ectasia makes the corneal power irregular, presenting challenges for IOL calculation in case No. 1.
We discussed his options and decided on topography-guided phototherapeutic keratectomy (PTK) to normalize the irregular ectasia and central corneal power. I did not think CXL would be beneficial in this case because the cone was stable (Figure 2). Three months after the PTK procedure (Figure 3), cataract surgery was performed. The central 4.5-mm total corneal power was measured with Scheimpflug topography, and the Holladay 1 formula was used for the IOL calculation because the anterior chamber was deep and the axial length was greater than 25 mm. An AcrySof aspheric IOL (model T2, Alcon) was implanted at 135º.

Figure 2. The epithelium over the cone (red arrows) was not thin in case No. 1.
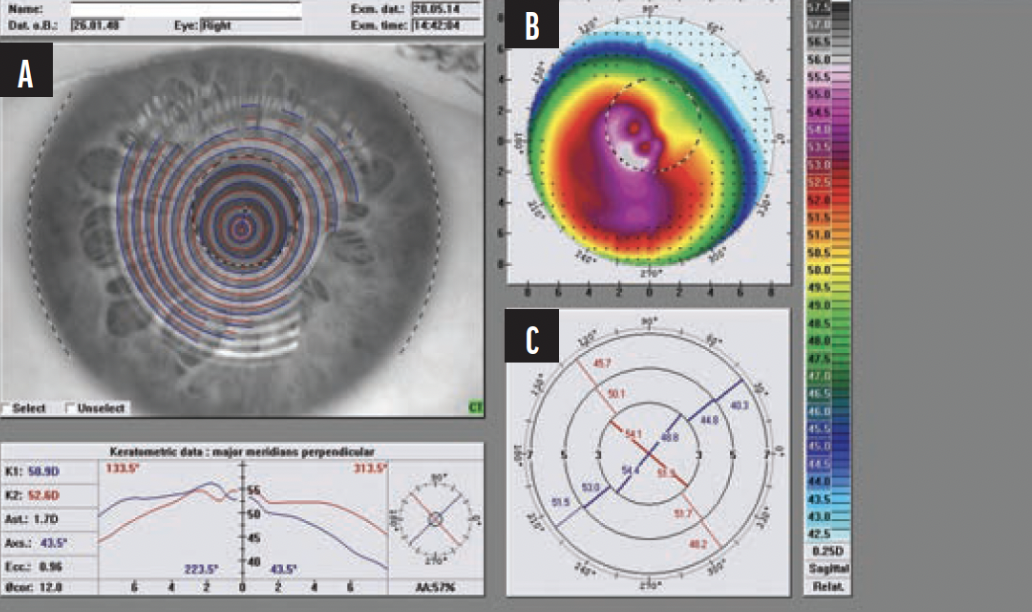
Figure 3. Preoperative (A), postoperative (B), and difference maps (C) after topography-guided phototherapeutic normalization of the central cornea in case No. 1.
Postoperatively, the patient’s uncorrected distance visual acuity (UDVA) and corrected distance visual acuity (CDVA) improved from 20/100 to 20/16 and 20/30 to 20/10, respectively. The refraction was +0.25 -0.50 x 180º.
Case No. 2
A 74-year-old woman with an old paracentral herpetic keratitis scar presented for a cataract surgery evaluation. She was intolerant of any type of contact lens and reported deteriorating vision. On examination, a nuclear sclerotic cataract was found. The scar had led to irregular corneal curvature that produced severe glare symptoms (Figure 4). Her UDVA and CDVA were 20/400 and 20/70, respectively.

Figure 4. In case No. 2, irregular corneal curvature was noted on Scheimpflug tomography (A) and Placido disc reflection tomography (B).
After a thorough discussion of options with the patient, we opted for a topography-guided PTK procedure to normalize the central corneal curvature and reduce the central corneal scar (Figures 5 and 6). Four months after surgery, her UDVA and CDVA improved to 20/100 and 20/50, respectively. Cataract surgery was then performed. The central 4.5-mm total corneal power was measured with Scheimpflug topography, targeting -0.75 D with an AcrySof toric aspheric IOL (model T4, Alcon) implanted at 60º because the other eye was emmetropic and pseudophakic.

Figure 5. Topography-guided PTK was performed in case No. 2 to reshape the corneal curvature and remove the central corneal scar.

Figure 6. Pre- and postoperative comparison of the cornea in case No. 2.
After cataract surgery, the patient’s UDVA was 20/30, her uncorrected near visual acuity was J2+, and her CDVA was 20/20 with a refraction of -0.50 - 0.50 x 155º.
1. Kanellopoulos AJ. Ten-year outcomes of progressive keratoconus management with the Athens protocol (topography-guided partial-refraction PRK combined with CXL). J Refract Surg. 2019;35(8):478-483.
2. Kanellopoulos AJ. Keratoconus management with customized photorefractive keratectomy by artificial intelligence ray-tracing optimization combined with higher fluence corneal crosslinking: the ray-tracing athens protocol. Cornea. 2021;40(9):1181-1187.
3. Krueger RR, Kanellopoulos AJ. Stability of simultaneous topography-guided photorefractive keratectomy and riboflavin/UV-A cross-linking for progressive keratoconus. J Refract Surg. 2010;26(10):S827-S832.
4. Kanellopoulos AJ. Topography-guided custom retreatments in 27 symptomatic eyes. J Refract Surg. 2005;21(5):S513-8.
5. Kanellopoulos AJ, Asimellis G. Corneal refractive power and symmetry changes following normalization of ectasias treated with partial topography-guided PTK combined with higher-fluence CXL (the Athens Protocol). J Refract Surg. 2014;30(5):342-346.




