
Significant residual refractive error can cause patient dissatisfaction. Avoiding residual ametropia after cataract surgery has therefore become a primary goal for most cataract surgeons. Irregular corneas are a barrier to achieving optimal visual outcomes. This article discusses how to manage three common causes of lumps and bumps on the corneal surface.
NO. 1: PTERYGIUM
This fibrovascular growth that invades the corneal stroma often causes flattening of the cornea in the horizontal meridian and overall flattening of keratometry (K) values. Once a pterygium has been excised, mean K values usually increase, producing a myopic shift. This is especially likely if the pterygium extends more than 2 mm into the cornea.1
Reasons to remove a pterygium before cataract surgery include recent progression, encroachment on the visual axis, and induced astigmatism that limits the patient’s BCVA. Any patient who desires a premium IOL should undergo pterygium surgery before cataract surgery, even if the pterygium is relatively small and particularly if it could be progressive.
Once healed, the cornea is reassessed to determine the most appropriate type of IOL. Unfortunately, significant corneal irregularity may remain after excision, particularly if the pterygium was deeply invasive. Alternatively, a toric IOL may no longer be necessary because the patient’s astigmatism resolved after the pterygium was excised.
Proper techniques must be used to remove a pterygium to avoid recurrence. Meticulous dissection and placing a conjunctival autograft can help minimize recurrence rates.2
NO. 2: EBMD
Epithelial basement membrane dystrophy (EBMD), also referred to as anterior basement membrane dystrophy and map-dot-fingerprint dystrophy, is relatively common. Slit-lamp findings include microcysts (dots), faint irregular lines that resemble coastlines on a map, and groups of wispy parallel lines that look like fingerprints. Signs are often subtle and easily overlooked, particularly in an eye with a mature cataract and diminished red reflex. Patients may experience ghosting of images from astigmatism or recurrent corneal erosions. Many individuals, however, are asymptomatic. It may not be possible to distinguish visual symptoms due to EBMD from those caused by cataracts.
EBMD is often apparent on preoperative imaging. When it is, such as the following example, it consistent K measurements may be difficult to obtain (Figure 1).
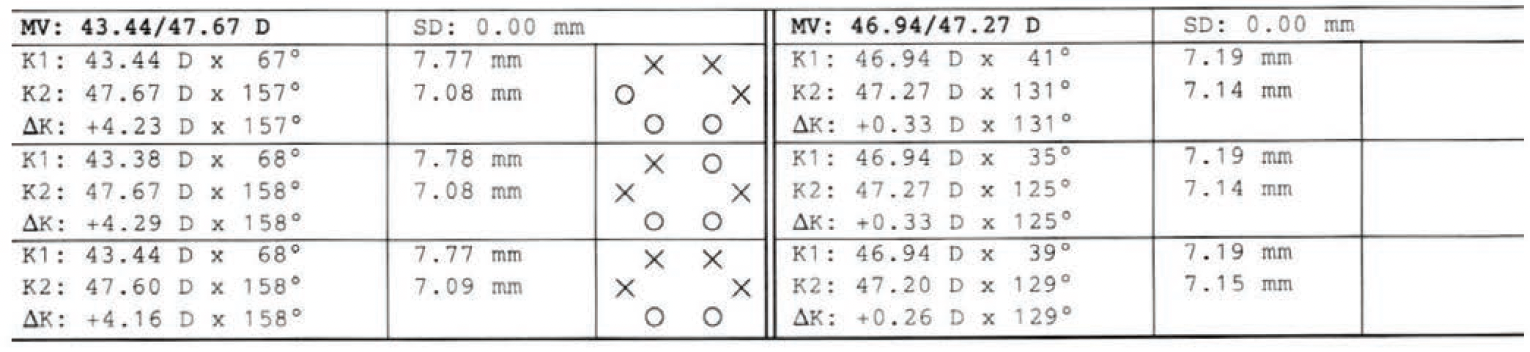
Figure 1. Unilateral high astigmatism and inconsistent K measurements can signal the presence of EBMD.
An 80-year-old woman underwent phaco cataract extraction with monofocal IOL implantation in her right eye. One week postoperatively, her BCVA was 20/40 OD with an autorefraction of -3.75 +6.50 x 163º. At this point, the surgeon noticed EBMD findings and referred the patient to me for a corneal evaluation. A review of her records revealed inconsistent K readings, high unilateral astigmatism on optical biometry, and widely variable refractions at separate visits, albeit not on the day of her initial cataract evaluation (+0.25 +1.25 x 155º OD), which is likely why the surgeon had not suspected corneal pathology other than dry eye. On careful examination, central and peripheral EBMD findings were evident in the right and left eyes, respectively.
I offered the patient a superficial keratectomy with diamond burr polishing in the right eye. I explained that she would likely experience a refractive shift after treatment.3 She elected to proceed.
Three months after the procedure, refraction revealed a significant reduction of astigmatism and a myopic shift (-2.25 +0.50 x 015º OD). The patient’s BCVA did not improve, presumably at least in part owing to the presence of subepithelial haze. Her subjective quality of vision improved, however, and she was much happier with her vision.
The case example illustrates how important it is to be vigilant for EBMD when planning cataract surgery and to suspect the condition if K values and refractions are inconsistent.
As with pterygium surgery, the treatment of EBMD leads to changes in K values that have a significant impact on IOL power calculations.3 Usually, there is a myopic shift, but the direction and amount of the refractive shift in each case is unpredictable.4 EBMD treatment may consist of superficial keratectomy with or without diamond burr polishing or phototherapeutic keratectomy. Similar results are obtained with either procedure.3,4
Focal steepening with irregular astigmatism on corneal topography can be indicative of EBMD (Figure 2). Had the aforementioned patient been interested in a toric or presbyopia-correcting IOL, topography would have been ordered.

Figure 2. An example of focal steepening and irregular astigmatism associated with EBMD.
This case also illustrates how preoperative imaging can help optimize visual outcomes in all patients, not just those opting for a premium IOL.
NO. 3: NODULAR AND SUBEPITHELIAL DEGENERATION
Salzmann nodular degeneration (SND) is characterized by the presence of focal subepithelial fibrosis. Like EBMD, SND can induce irregular astigmatism and significantly affect biometry measurements.3
Peripheral hypertrophic subepithelial degeneration (PHSD) is a histopathologically similar condition. It presents as bilateral peripheral lesions that may be flatter than typical SND. Fine neovascularization is typically present. PHSD can induce progressive hyperopia in addition to irregular astigmatism (Figure 3).5

Figure 3. PHSD appears as an annular, peripheral, subepithelial, mildly raised, translucent opacity, often with areas of fine peripheral vascularization.
The removal of SND and PHSD lesions is warranted to reduce significant irregular astigmatism or treat progressive hyperopia associated with PHSD. The overlying epithelium is removed, and the lesions are peeled. SND and PHSD can recur, which must be considered when choosing an IOL and counseling patients.
CONCLUSION
Corneal lumps and bumps are one cause of irregular astigmatism, and they can decrease patient satisfaction after cataract surgery. Generally, pterygium, EBMD, SND, and PHSD should be treated at least 2 to 3 months before patients undergo biometry measurements for cataract surgery. Corneal topography can help determine the visual significance of a lesion, but there is no clear cutoff.
Superficial and phototherapeutic keratectomy are relatively low-risk procedures, but both can trigger a persistent epithelial defect or recurrent corneal erosion syndrome. Thus, it may be better to leave EBMD of questionable visual significance alone in someone with a history of poor wound healing, for example.
Irregular astigmatism and other symptoms generally improve significantly after the treatment of pterygium, SND, EBMD, and PHSD. There can, however, be residual or recurrent corneal irregularity or haze that may limit vision. Setting realistic patient expectations is critical.
1. Kim SW, Park S, Im CY, Seo KY, Kim EK. Prediction of mean corneal power change after pterygium excision. Cornea. 2014;33(2):148-153.
2. Janson BJ, Sikder S. Surgical management of pterygium. Ocul Surf. 2014;12(2):112-119.
3. Goerlitz-Jessen MF, Gupta PK, Kim T. Impact of epithelial basement membrane dystrophy and Salzmann nodular degeneration on biometry measurements. J Cataract Refract Surg. 2019;45(8):1119-1123.
4. Itty S, Hamilton SS, Baratz KH, Diehl NN, Maguire LJ. Outcomes of epithelial debridement for anterior basement membrane dystrophy. Am J Ophthalmol. 2007;144(2):217-221.
5. Raber IM, Eagle RC Jr. Peripheral hypertrophic subepithelial corneal degeneration. Cornea. 2022;41(2):183-191.




