
Patients with ocular surface disease (OSD) are at an increased risk of complications after cataract surgery. The health of the cornea should be optimized preoperatively to increase the accuracy of biometry measurements and reduce the risk of complications such as persistent epithelial defects (PEDs), corneal haze and scarring, and perforation. This article discusses strategies for preventing and managing PEDs.
PREVENTION
Identification. The first step is to identify individuals at increased risk of PEDs before cataract surgery. There are four main etiologies of a PED.1
No. 1: Epithelial or limbal stem cell deficiency;
No. 2: Inflammatory disease (keratoconjunctivitis sicca);
No. 3: Neurotrophic disease such as herpes simplex virus (HSV), diabetes, or a history of laser eye surgery; and
No. 4: Mechanical factors (abnormal lid pathology).
Intervention. The ocular surface of patients who have OSD secondary to one of the aforementioned etiologies should be optimized before cataract surgery. Options include but are not limited to nonpreserved ocular lubricants, punctal occlusion, topical immunomodulatory agents (eg, cyclosporine), topical lymphocyte function–associated antigen 1 antagonist drugs (eg, lifitegrast), varenicline nasal spray, and autologous serum or platelet-rich plasma (PRP) eye drops.2 Patients with a history of herpes simplex virus or varicella zoster virus keratitis should begin therapy with the full treatment dose of an oral antiviral (eg, acyclovir, valacyclovir) 48 to 72 hours before cataract surgery. Prophylactic treatment with an antiviral medication can greatly reduce the risk of a flareup after cataract surgery. Lastly, significantly abnormal lid pathology, such as severe entropion or ectropion, should be addressed before intraocular surgery.
Surgical considerations. Cataract surgery on patients with OSD is essentially routine except that a greater amount of balanced salt solution may be used to hydrate the cornea intraoperatively. Maintaining an intact epithelium throughout surgery decreases the risk of postoperative complications. After surgery, patients should immediately resume administering nonpreserved artificial tears in addition to starting a steroid, NSAID, and/or antibiotic.
Patients with OSD are predisposed to develop PEDs after cataract surgery. Careful postoperative monitoring is therefore required, particularly if the individual has decreased or absent sensation (ie, neurotrophic keratitis). Topical steroid treatment is necessary after cataract surgery to control inflammation, but it should be tapered as soon as possible because the agents also inhibit epithelial regrowth.
MANAGEMENT
First-line treatment. If not treated swiftly, PEDs can cause irreversible vision loss due to corneal haze, scarring, neovascularization, infection, and perforation. First-line management involves aggressive lubrication of the ocular surface with nonpreserved artificial tears and ointment as well as punctal occlusion (if not already present). Temporary collagen plugs, silicone plugs, or punctal cauterization may be used. The early placement of a bandage contact lens may be considered as well to protect the cornea from mechanical trauma during blinking. A bandage contact lens with high oxygen permeability, such as the Acuvue Oasys (Johnson & Johnson Vision), should be used.
Amniotic membrane and serum tears. If first-line measures are unsuccessful, amniotic membrane (AM) transplantation in the office and/or serum tears are the next step. AMs have been shown to promote corneal reepithelialization by releasing growth factors that stimulate and support the corneal epithelial cells and prevent apoptosis.3 Various AMs are available (dehydrated, cryopreserved, lyophilized). They may be placed in the office or sutured in the OR. Treatment with topical antibiotics should continue while an AM is in place.
Autologous serum and PRP tears contain components of natural tears such as vitamins, structural proteins, enzymes, and growth factors. These preservative-free tears have been used to treat PEDs for more than 2 decades.4 Platelet-derived growth factors inhibit apoptosis and improve cell growth and migration. Serum and PRP tears can reverse ocular pathology and promote corneal nerve regeneration, which is important in patients with poor epithelial healing secondary to neurotrophic keratitis. My clinic uses the system and protocol from Dr PRP USA to draw patients’ blood and prepare the PRP drops on the same day (Figure).
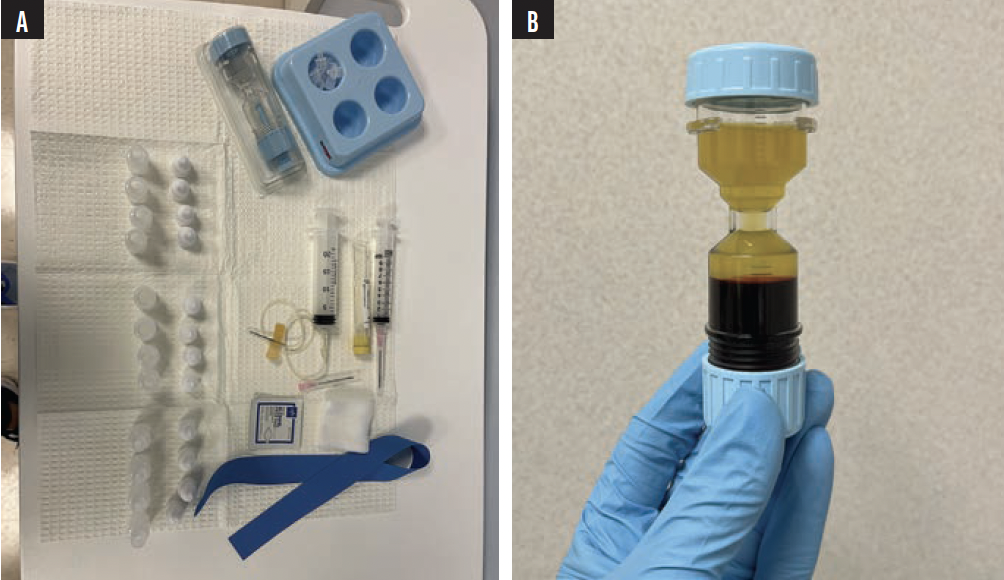
Figure. Preparations are made to draw a patient’s blood (A). PRP drops are mixed (B).
Antibiotics. Oral tetracycline and doxycycline have anticollagenolytic activity. The agents can decrease the risk of stromal melting and can be an effective adjunctive treatment in patients with PEDs.5
Vitamins. Ascorbic acid (vitamin C) has been found to accelerate epithelial wound healing and may decrease the risk of stromal haze.6
Recombinant human nerve growth factor. Cenegermin-bkbj 0.002% ophthalmic solution (Oxervate, Dompé) is an option for patients with a PED due to neurotrophic keratitis.7 The medication is administered six times per day for 8 weeks. Treatment increases corneal sensation and sensitivity and induces healing.
Insulin. Topical insulin (1 unit per mL) was recently shown to accelerate reepithelialization in patients with PEDs.8,9 The exact mechanism of action is not well understood. It has been hypothesized that the treatment increases DNA synthesis in basal epithelial cells and mediates receptor homeostasis in corneal epithelial cells. Topical insulin may be a better option than autologous serum drops in patients for whom a blood draw is difficult. In some situations, insulin may also be more cost-effective than serum tears.
Antivirals. Patients who have a history of herpetic keratitis should continue administering an oral antiviral medication for at least 1 week after cataract surgery. Treatment with a topical antiviral medication may also be considered, but it must be balanced with potential toxic effects on the cornea.10
Additional measures. In the rare situation where none of the aforementioned treatments is successful, a tarsorrhaphy or scleral contact lens wear such as Prosthetic Replacement of Ocular Surface Ecosystem (PROSE, BostonSight) may be attempted. Corneal neurotization should be considered for cases of severe refractory PEDs.
CONCLUSION
Optimizing the corneas of patients with OSD can reduce the risk of complications after cataract surgery. If a PED develops, treatment should be initiated as soon as possible to rehabilitate the corneal epithelium and improve the patient’s vision.
1. Dahlgren MA. Persistent epithelial defects. In: Albert DM, Jakobief FA, Miller JW, eds. Albert & Jakobiec’s Principles and Practice of Ophthalmology. Elsevier; 2008:749-759.
2. AAO PPP Cornea/External Disease Committee. Dry eye syndrome PPP – 2018. American Academy of Ophthalmology. November 13, 2018. Accessed August 15, 2023. https://www.aao.org/education/preferred-practice-pattern/dry-eye-syndrome-ppp-2018
3. Lee SH, Tseng SC. Amniotic membrane transplantation for persistent epithelial defects with ulceration. Am J Ophthalmol. 1997;123(3):303-312.
4. Tsubota K, Goto E, Shimmura S, Shimazaki J. Treatment of persistent corneal epithelial defect by autologous serum application. Ophthalmology.1999;106(10):1984-1989.
5. Perry HD, Kenyon KR, Lamberts DW, Foulks GN, Seedor JA, Golub LM. Systemic tetracycline hydrochloride as adjunctive therapy in the treatment of persistent epithelial defects. Ophthalmology. 1986;93(10):1320-1322.
6. Chen J, Lan J, Liu D, et al. Ascorbic acid promotes the stemness of corneal epithelial stem/progenitor cells and accelerates epithelial wound healing in the cornea. Stem Cells Transl Med. 2017;6(5):1356-1365.
7. Pflugfelder SC, Massaro-Giordano M, Perez VL, et al. Topical recombinant human nerve growth factor (cenegermin) for neurotrophic keratopathy: a multicenter randomized vehicle-controlled pivotal trial. Ophthalmology. 2020;127(1):14-26.
8. Soares RJDSM, Arêde C, Sousa Neves F, da Silva Fernandes J, Cunha Ferreira C, Sequeira J. Topical insulin–utility and results in refractory neurotrophic keratopathy in stages 2 and 3. Cornea. 2021;41(8):990-994.
9. Diaz-Valle D, Burgos-Blasco B, Gegundez-Fernandez JA, et al. Topical insulin for refractory persistent corneal epithelial defects. Eur J Ophthalmol. 2020;31(5):2280-2286.
10. Imperia PS, Lazarus HM, Dunkel EC, Pavan-Langston D, Geary PA, Lass JH. An in vitro study of ophthalmic antiviral agent toxicity on rabbit corneal epithelium. Antiviral Res. 1988;9(4):263-272.




