Posterior polar cataracts present a high risk of a ruptured posterior capsule and vitreous loss during cataract surgery. They can challenge even skilled cataract surgeons. This article and the accompanying video (watch below) present 10 tips for preventing and managing complications.
OUR TOP TIPS
No. 1: Identify posterior polar cataracts. The first key to successful management is to identify posterior polar cataracts during the slit-lamp examination. The cataracts have a characteristic bull’s eye or onion peel appearance in the central part of the posterior capsule (Figure 1).
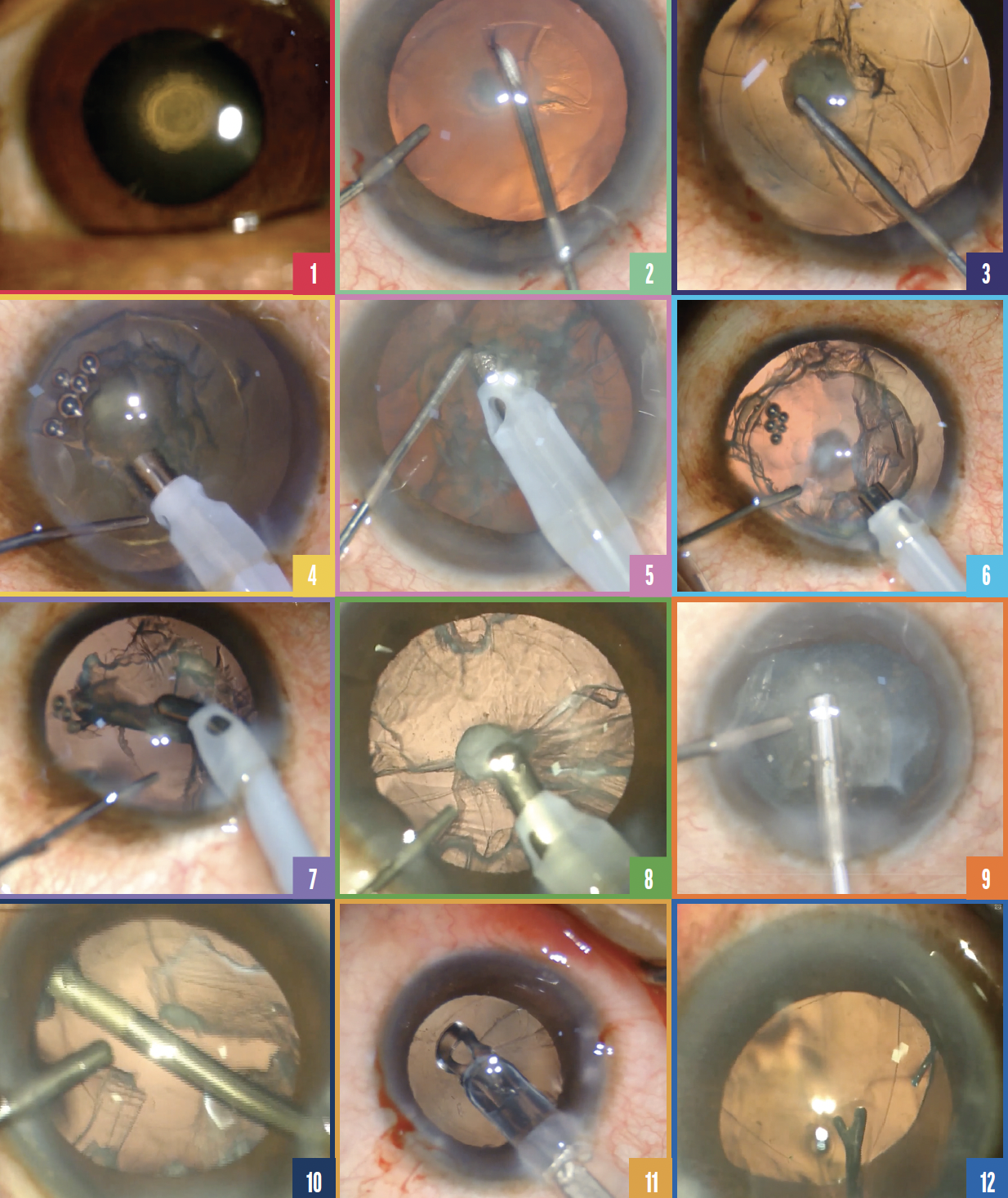
Figure 1. At the slit lamp, posterior polar cataracts characteristically have a bull’s eye or onion peel appearance in the central part of the posterior capsule.
Figure 2. The capsulorhexis with a diameter of approximately 5 mm is created.
Figure 3. Hydrodelineation is performed by pressing the cannula into the lens and delivering multiple fluid injections to separate the nucleus from the epinucleus.
Figure 4. Trenches are created with phacoemulsification to bowl out the nucleus.
Figure 5. Slow-motion phacoemulsification in a hard cataract.
Figure 6. An OVD is injected through a sideport incision.
Figure 7. Before the central area of attached plaque is removed, 360º of epinucleus is stripped from the capsular fornices.
Figure 8. A dispersive OVD is injected through a sideport incision to tamponade the vitreous.
Figure 9. Vitreous is removed from the anterior chamber.
Figure 10. Bimanual irrigation and aspiration are used to remove residual cortex.
Figure 11. A foldable IOL is implanted in the bag after a posterior capsular rent was converted into a posterior capsulorhexis.
Figure 12. Optic capture of a three-piece IOL is performed to stabilize the lens in an eye with a large tear in the posterior capsule.
No. 2: Size the capsulorhexis appropriately. The ideal diameter of the capsulorhexis is around 5 mm (Figure 2). A larger opening may not leave enough space to place an IOL in the sulcus if the posterior capsule tears. Too small a capsulorhexis could increase hydrostatic pressure during hydrodelineation and cause the posterior capsule to rupture.
No. 3: Avoid hydrodissection. Hydrodissection can cause hydraulic rupture of the posterior capsule and result in a dropped nucleus. The step should therefore be avoided in favor of hydrodelineation, which creates a cushion of epinucleus and an endonucleus that can be easily removed with phacoemulsification. The tip of the hydrodelineation cannula is pressed into the lens (Figure 3). Multiple fluid injections are then delivered in a controlled fashion to separate the nucleus from the epinucleus, yielding a characteristic golden ring.
No. 4: Do not rotate the nucleus. Rotation of the nucleus can rupture the posterior capsule and should thus be avoided.
No. 5: Perform slow-motion phacoemulsification. The approach to nucleus management depends on the cataract grade. If the cataract is soft, then adjacent trenches are created in the nucleus to form a bowl, which is then emulsified within a cushion of epinucleus (Figure 4).
For a harder cataract, step-by-step chop in situ and a lateral separation technique may be used. Slow-motion phacoemulsification with low aspiration, infusion, and vacuum parameters is preferred (Figure 5). The low vacuum and aspiration rate maintain a stable anterior chamber, and low infusion pressure drives less fluid around the lens.
No. 6: Inject an OVD through a sideport incision. Major fluctuations in anterior chamber pressure should be avoided. An OVD should be injected through a sideport incision before the phaco or I/A tip is withdrawn from the eye (Figure 6). This helps maintain a well-formed anterior chamber and prevents forward bulging of the posterior capsule during surgery.
No. 7: Manage the epinucleus and cortex. Before the central area of attached plaque is removed, 360º of epinucleus is stripped from the capsular fornices so that epinuclear and cortical matter does not drop into the vitreous. The central plaque is then slowly stripped and aspirated in a controlled manner (Figure 7). Cortical matter is removed in a similar fashion.
No. 8: Immediately inject an OVD if the posterior capsule tears. A dispersive OVD injected through a sideport incision before the phaco tip is withdrawn from the eye (Figure 8) helps tamponade the vitreous and prevent it from entering the anterior chamber.
No. 9: Perform a bimanual anterior vitrectomy. The infusion bottle is lowered. A bimanual vitrectomy with or without triamcinolone acetonide is performed with low suction and a high cutting rate to remove vitreous from the anterior chamber (Figure 9). Bimanual irrigation and aspiration are used to remove residual cortex (Figure 10).
No 10: Tailor the approach to IOL implantation depending on the status of the posterior capsule. If the posterior capsule is intact, then care must be taken to avoid the capsule during the injection of an IOL. When the posterior capsule has ruptured, the approach to IOL implantation depends on the size of the tear. If the rent is small, then it can be converted into a posterior capsulorhexis and a foldable IOL can be implanted in the bag (Figure 11). If the tear is large, then a three-piece IOL is implanted in the sulcus. Optic capture may be used to stabilize the IOL and reduce contact between the lens optic and iris (Figure 12).
CONCLUSION
Cataract surgery in eyes with posterior polar cataracts is challenging. A careful technique such as the one outlined here can help decrease the risk of a ruptured posterior capsule and vitreous loss.