Where Things Are Heading in Switzerland
Farhad Hafezi, MD, PhD, FARVO

Switzerland in general and Zurich in particular have been at the heart of CXL research and innovation for more than 20 years. Most surgeons here still perform epithelium-off (epi-off) CXL with either the Dresden or an accelerated CXL (ACXL) protocol. The latter is typically 9 mW/cm2 for 10 minutes, which delivers the same fluence as the Dresden protocol (5.4 J/cm2) in a shorter period.
ON THE NEAR HORIZON
Ultrastrong epi-off CXL. Until recently, 9 mW/cm2 for 10 minutes was considered to be a reasonable trade-off between corneal strengthening and duration of irradiation. That view is changing.
My colleagues and I have developed an even stronger epi-off CXL protocol that produces Dresden-like levels of strengthening but in one-third the time. We perform UV irradiation at an intensity of 18 mW/cm2 for 9 minutes and 15 seconds, which delivers a UV fluence of 10 instead of 5.4 J/cm2. In the laboratory, we found that the protocol delivered a corneal stiffening effect that was indistinguishable from that achieved with the Dresden protocol and without requiring modifications to the CXL procedure such as adding supplemental oxygen.1
Epi-on CXL without oxygen and iontophoresis. Our research group has developed an epi-on CXL protocol that uses a riboflavin solution with penetration enhancers instead of supplemental oxygen or iontophoresis. In laboratory experiments, we found the protocol resulted in similar corneal stiffening effects as epi-off CXL that used an accelerated protocol of 9 mW/cm2 for 10 minutes. One advantage of the epi-on procedure is that it avoids the potential drawbacks associated with removing and regrowing the epithelium. We plan to publish our preclinical data in the near future.
Further in the Future
To our knowledge, ours is the only research group in the world that has all three of the following cutting-edge corneal biomechanical assessment instruments: a high-speed air puff corneal deformation device (Corvis ST, Oculus Optikgeräte), a Brillouin Optical Scanner System (Intelon Optics), and an OCT elastography system prototype. These instruments provide new insights into keratoconus.
Our group is also trying to improve photoactivated chromophore for keratitis-CXL (PACK-CXL) for the treatment of infectious keratitis.2 We have already shown that higher fluences than those used in the Dresden protocol are required to treat many cases of infectious keratitis successfully3,4 (the opacity of the ulcers makes the depth of the PACK-CXL effect rather shallow).5
We continue to learn more about the procedure’s strengths and limitations. For example, higher UV fluences are required to kill certain bacteria.3 Moreover, although bacteria and many species of fungi can be effectively killed by PACK-CXL performed with riboflavin and UV light, eradicating other organisms such as Acanthamoeba is far more challenging.6 Additional combinations of light wavelengths and chromophores are available.7 We are the first group to evaluate the combined effect of PACK-CXL performed with both rose bengal/green light and riboflavin/UV-A in the same session for the treatment of both recalcitrant fungal and Acanthamoeba keratitis.
1. Abrishamchi R, Abdshahzadeh H, Hillen M, et al. High-fluence accelerated epithelium-off corneal cross-linking protocol provides Dresden protocol-like corneal strengthening. Transl Vis Sci Technol. 2021;10(5):10.
2. Hafezi F, Hosny M, Shetty R, et al. PACK-CXL vs. antimicrobial therapy for bacterial, fungal, and mixed infectious keratitis: a prospective randomized phase 3 trial. Eye Vis (Lond). 2022;9(1):2.
3. Kling S, Hufschmid FS, Torres-Netto EA, et al. High fluence increases the antibacterial efficacy of PACK cross-linking. Cornea. 2020;39(8):1020-1026.
4. Hafezi F, Munzinger A, Goldblum D, Hillen M, Tandogan T. Repeated high-fluence accelerated slitlamp-based photoactivated chromophore for keratitis corneal cross-linking for treatment-resistant fungal keratitis. Cornea. 2022;41(8):1058-1061.
5. Hafezi F, Torres-Netto EA, Hillen MJP. Re: Prajna et al.: Cross-linking—assisted infection reduction: a randomized clinical trial evaluating the effect of adjuvant cross-linking on outcomes in fungal keratitis (Ophthalmology. 2020;127:159-166). Ophthalmology. 2021;128(1):e6.
6. Watson SH, Shekhawat NS, Daoud YJ. Treatment of recalcitrant Acanthamoeba keratitis with photoactivated chromophore for infectious keratitis corneal collagen cross-linking (PACK-CXL). Am J Ophthalmol Case Rep. 2022;25:101330.
7. Altamirano D, Martinez J, Leviste KD, Parel JM, Amescua G. Photodynamic therapy for infectious keratitis. Curr Ophthalmol Rep. 2020;8:245-251.
Where Things Stand in Israel
Boris Knyazer, MD

In Israel, where I practice, an estimated 9,393,500 citizens live on 20,770 km2 of land. The population is 74% Jewish, 21% Arabic, and 5% non-Arab Christians.
Health care delivery is just one area made more complex by the variety of cultures and religions (Judaism, Christianity, Islam, Samaritanism, the Druze Faith, and the Bahá’í Faith), climatic zones (Mediterranean, semi-arid, and desert), and socioeconomic statuses found in Israel. These factors lead to variations in the genetic and environmental risk factors for developing keratoconus, its prevalence in different population groups, its diagnosis, and its treatment.
DIFFERENCES AMONg POPULATIONS
In one study, the prevalence of keratoconus in Israel was 2.3%. Among 934 college students, the incidence was much higher in men than women (4.9% vs 1.1%) and in Arabs than Jews (3.0% vs 2.2%). The study also found family history (21.7%) and atopy (40.9%) but not eye rubbing to be significantly associated with keratoconus.1
I work at Soroka University Medical Center, Israel’s largest public hospital. It is in Beer-Sheva, which is located in the Negev area in the south of the country. The hospital serves a large population that is approximately 60% Jewish and 36% Bedouin. In 2022, my colleagues and I collected data on 200 patients with keratoconus who were treated in our department. We found that the Bedouin patients were significantly younger at the time of keratoconus diagnosis than the Jewish patients (18.7 vs 23.6 years), experienced more rapidly progressive disease (maximum keratometry values of 58.20 vs 56.20 D), and had thinner corneas (435 vs 465 µm). Additionally, compared to the Jewish patients, the Bedouin patients were more likely to have atopy (28% vs 18.1%) and a family history of keratoconus (37.9% vs 13.7%). All variables were statistically significant (unpublished data). Following this research, we advised health care services to educate the public on the consequences of untreated keratoconus and provide screening tests and early intervention in the community clinics of the minority population in the Negev area. As the Bedouin population in this area is a socioeconomically disadvantaged minority with limited access to health care services, we suggest our recommendations should be implemented in similar minority communities globally.
CXL CARE
Health care is universal here, and participation in a medical insurance plan is compulsory. Basic health care is a fundamental right of every Israeli resident. CXL has been covered by health insurance plans since 2014. Patients at public and private hospitals can undergo CXL almost immediately.
Progressive and pediatric keratoconus. The general indications for CXL are the same in Israel as in other countries. Ophthalmologists in my country consider CXL for the treatment of progressive keratoconus in adults. Most perform the procedure immediately when children are diagnosed with the disease.
Infectious keratitis. This is another indication for CXL, but we are not obliged to perform the procedure for the condition in Israel. Cornea specialists decide whether to proceed on a case-by-case basis.
COMPARING CXL APPLICATIONS
My colleagues and I are conducting research comparing standard and ACXL treatment protocols in pediatric and adult populations. We recently published the results of a 3-year study that compared two CXL intensities—3 mW/cm2 delivered for 30 minutes versus 9 mW/cm2 delivered for 10 minutes. We found both to be safe and effective.2 The findings give hope to cornea specialists that CXL treatment in pediatric patients can be simplified.
We are also evaluating PACK-CXL. Our group is the first to administer accelerated PACK-CXL at an intensity of 30 mW/cm2 for 3 minutes in patients with infectious keratitis. We found the safety and efficacy of this protocol to be at least the same as with standard topical antibiotic treatment. In one of our comparison studies, we found that PACK-CXL plus topical antibiotic treatment in bacterial keratitis was associated with shorter times for reepithelialization, duration of follow-up, and hospitalization and lower rates of emergent penetrating keratoplasty operations compared to standard topical antibiotic treatment.3
More than 2 years ago, my hospital’s cornea unit began treating all patients who have infectious keratitis with high-fluence PACK-CXL (HF PACK-CXL; 30 mW/cm2 for 6 minutes and fluence of 10.8 J/cm2).4 The transition was motivated by the experimental in vitro work of Hafezi et al, who demonstrated a higher bacterial killing rate with HF PACK-CXL compared to standard fluence (5.4 J/cm2).5 In the past year, all PACK-CXL cases in our department were performed at the slit lamp with the C-eye device (EMAGine).4
I expect our research during the next few years to focus on HF treatments for keratoconus, infectious keratitis, and keratectasia; new protocols for epi-off CXL; the treatment of thin corneas; and PACK-CXL with new chromophores. Evidence is accumulating that HF CXL is an effective and safe treatment. I expect it to be the way of the future.
1. Millodot M, Shneor E, Albou S, Atlani E, Gordon-Shaag A. Prevalence and associated factors of keratoconus in Jerusalem: a cross-sectional study. Ophthalmic Epidemiol. 2011;18(2):91-97.
2. Einan-Lifshitz A, Achiron A, Hed S, Hecht I, Dubinsky-Pertzov B, Knyazer B. Three-year follow-up of accelerated versus standard corneal cross-linking in paediatric keratoconus. Eye (Lond). Published online May 19, 2022. doi:10.1038/s41433-022-02093-4
3. Achiron A, Elhaddad O, Regev T, et al. PACK cross-linking as adjuvant therapy improves clinical outcomes in culture-confirmed bacterial keratitis. Cornea. 2022;41(9):1069-1073.
4. Knyazer B, Hillen M, Hafezi F. Corneal cross-linking for infectious keratitis at the slit lamp in wheelchair users. Journal of Refractive Surgery Case Reports. 2021;1(3):e36- e39.
5. Kling S, Hufschmid FS, Torres-Netto EA, et al. High fluence increases the antibacterial efficacy of PACK cross-linking. Cornea. 2020;39(8):1020-1026.
Epi-On, High-Fluence Protocols and New Therapeutic Procedures Hold Promise
Cosimo Mazzotta, MD, PhD

Standard CXL (S-CXL) can slow or halt the progression of keratoconus. The procedure can also have beneficial visual, optical, and topographic effects, including improvements in corneal curvature, topographic indices of asymmetry, and higher-order aberrations (HOAs).
In recent years, ACXL protocols have replaced older, more time-consuming techniques, leading to better patient compliance and clinic workflow.1
NEW PROTOCOL FOR EPI-OFF ACXL
The Siena Eye-Cross Study 2 evaluated the long-term clinical results of 9 mW/5.4 J/cm2 epi-off ACXL for the treatment of progressive keratoconus. In young adults and pediatric patients, the 5-year results demonstrated statistically significant improvements in UCVA, corrected distance visual acuity, corneal curvature, and HOAs, thus stabilizing progressive ectasia.1
In Italy and most other European countries, the Dresden protocol has been replaced by 9 mW/5.4 J/cm2 epi-off ACXL with an exposure time of 10 minutes. Total CXL treatment time has decreased from 1 hour to 20 minutes, which increases in patient comfort without reducing the procedure’s overall safety and efficacy compared to S-CXL.1
EPITHELIUM-ON ACXL
A higher fluence can also increase the efficacy of epi-on ACXL treatment with or without iontophoresis riboflavin loading and with or without intraoperative supplemental oxygen.2-4 One protocol for epi-on ACXL with iontophoresis, the Ionto-plus protocol, uses a high fluence of 7 J/cm2 (vs 5.4 J/cm2), pulsed light, UV-A power of 18 mW/cm2, and an exposure time of 13 minutes.3 In a prospective interventional case series, the Ionto-plus protocol improved the photochemical kinetic and functional outcomes of the original iontophoresis CXL (I-CXL) protocol.3 Results with Ionto-plus CXL were similar to those achieved with S-CXL, including a reduction in the maximum keratometry reading of 1.40 D and a decrease in HOAs. Fewer retreatments were required with Ionto-plus CXL compared to I-CXL, with its reported rate of 25%.3
Three-year results were recently reported for a protocol that uses chemically enhanced, hyperconcentrated (0.25% and 0.22%) riboflavin solutions without iontophoresis and with air-room oxygenation. This approach to epi-on ACXL was less invasive because no suction ring is needed, potentially making it a more attractive and cost-effective option for young patients for whom compliance with treatment may be challenging.4
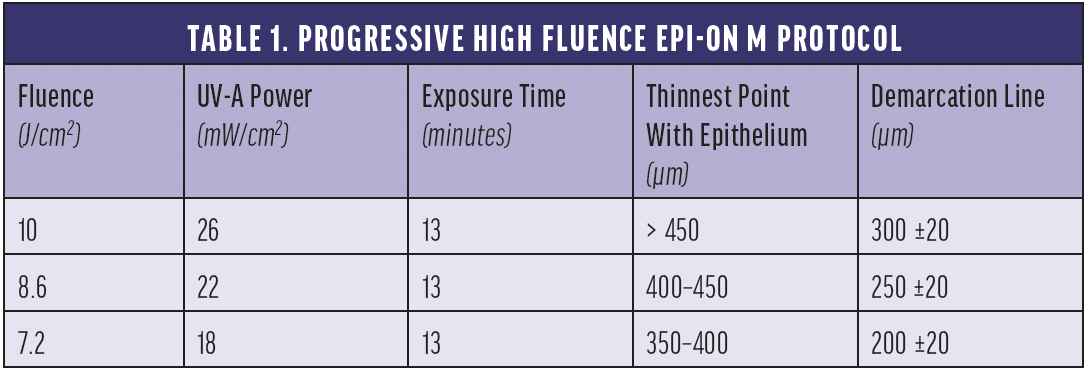
Translational clinical investigations at the Siena CXL Center of the latest protocols using fluences of 7, 8.6, and 10 J/cm2 with pulsed light are generating promising results. Demarcation line depths and corneal flattening appear to be comparable if not superior to those achieved with other epi-on CXL procedures.4
High-fluence protocols hold promise for reducing the gap in efficacy between epi-on and epi-off CXL. These less-invasive protocols also have the advantages of eliminating the risk of corneal infection, haze, and extreme thinning as well as shortening the rehabilitative period after treatment.1-5
COMBINED PROCEDURES
CXL is being performed in conjunction with other procedures in patients who have poor BCVA and are intolerant of rigid gas permeable contact lenses. For example, simultaneous selective transepithelial ablation and CXL (CXL+) are performed for refractive enhancement,6 and CXL can be combined with keratoplasty (donor-recipient CXL-assisted deep anterior lamellar keratoplasty) to stabilize the wound and reduce the risk of rejection and early or late dehiscence of transplanted tissue.7
The Siena Crosslinking Center, where I practice, recently began using a new therapeutic option I developed, ray tracing–guided phototherapeutic keratectomy combined with individualized pachymetry-based ACXL (M nomogram).8 The approach is used to treat corneas of all thicknesses, including thin (350–400 µm) and ultrathin (250–350 µm) corneas (Table 1 and Figure 1). The ray-tracing software allows the refractive contribution of the posterior corneal surface and epithelium to be evaluated, customizes excimer laser ablation to deliver well-balanced central corneal remodeling, reduces morphologic corneal irregularities, and minimizes tissue consumption. A small amount of aberration is left at the anterior corneal surface to compensate for posterior surface irregularity, thus avoiding an overcorrection. My colleagues and I hope to publish our long-term results with this combined procedure soon. Our goal is for the combined epi-on CXL procedure to be safe, efficacious, affordable, and accessible.
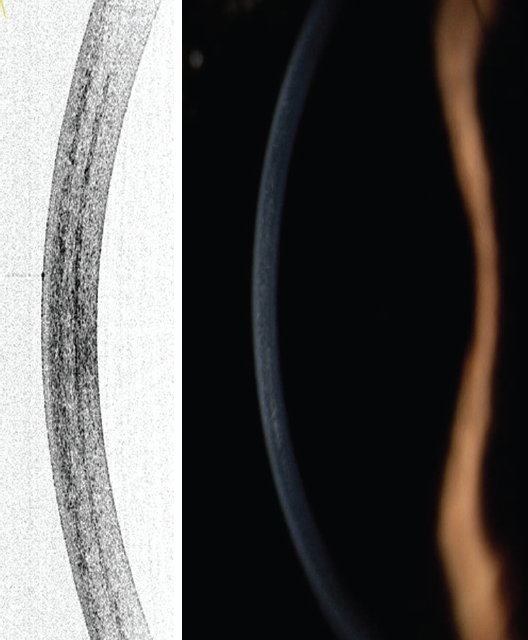
Figure 1. Demarcation lines at a depth of 300 µm are detectable on corneal OCT and at the slit lamp after the progressive high fluence pulsed light epi-on M protocol.
Courtesy of Cosimo Mazzotta, MD, PhD
1. Mazzotta C, Raiskup F, Hafezi F, et al. Long term results of accelerated 9 mW corneal crosslinking for early progressive keratoconus: the Siena Eye-Cross Study 2. Eye Vis (Lond). 2021;8(1):16.
2. Mazzotta C, Bagaglia SA, Sgheri A, et al. Iontophoresis corneal cross-linking with enhanced fluence and pulsed UV-A light: 3-year clinical results. J Refract Surg. 2020;36(5):286-292.
3. Mazzotta C, Sgheri A, Bagaglia SA, Rechichi M, Di Maggio A. Customized corneal crosslinking for treatment of progressive keratoconus: clinical and OCT outcomes using a transepithelial approach with supplemental oxygen. J Cataract Refract Surg. 2020;46:1582-1587.
4. Mazzotta C, Balamoun AA, Chabib A, et al. Transepithelial enhanced fluence pulsed light M accelerated crosslinking for early progressive keratoconus with chemically enhanced riboflavin solutions and air room oxygen. J Clin Med. 2022;11(17):5039.
5. Mazzotta C, Moramarco A, Traversi C, Baiocchi S, Iovieno A, Fontana L. Accelerated corneal collagen cross-linking using topography-guided UV-A energy emission: preliminary clinical and morphological outcomes. J Ophthalmol. 2016;2016:2031031.
6. Rechichi M, Mazzotta C, Oliverio GW, et al. Selective transepithelial ablation with simultaneous accelerated Corneal cross-linking for corneal regularization of keratoconus: the STARE-X Protocol. J Cataract Refract Surg. 2021;47(11):1403-1410.
7. Zagari M, Mazzotta C, Zagari S, Armia A. Donor-recipient crosslinking-assisted manual deep anterior lamellar keratoplasty: DRXL-DALK. In: Keratoconus: Current and Future State-of-the-Art. Armia A, Mazzotta C, eds. Springer Nature Switzerland; 10.1007/978-3-030-84506-3.
8. Mazzotta C, Romani A, Burroni A. Pachymetry-based accelerated cross-linking: the “M nomogram” for standardized treatment of all-thickness progressive ectatic corneas. Int K Kerat Ect Corn Dis. 2018;7(2):137-144.
Epi-On CXL: Scientific Progress Reported
Roy S. Rubinfeld, MD, MA

My 3-year-old daughter scratched my eye with her fingernail decades ago, ironically while I was a cornea fellow at Wills Eye Hospital. It was so excruciating that years later I had some idea of what my epi-off CXL patients described to me and why they often needed opioids. CXL as a procedure is remarkable, stiffening the cornea to slow or halt the progression of keratoconus and secondary ectasia. But what if it could be improved?
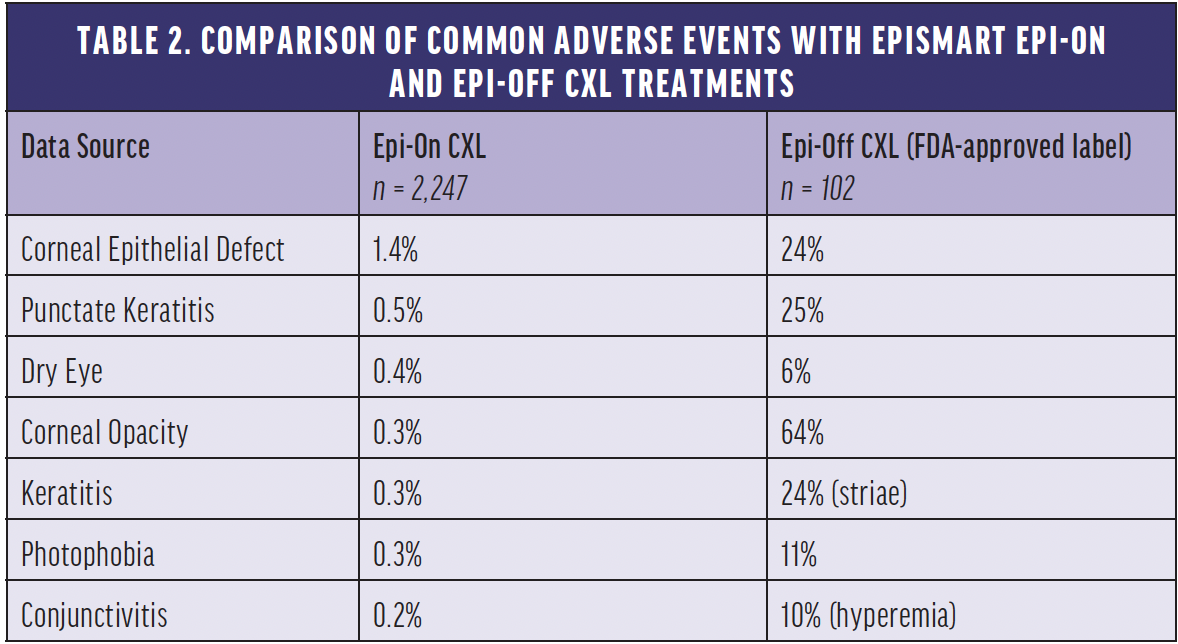
Since the introduction of CXL, work has been done by numerous groups worldwide to develop systems and protocols for effective epi-on CXL that avoid epithelial debridement but achieve adequate riboflavin saturation of the corneal stroma before irradiation with UV-A light. Until now, these have met with little success.1-3 Authentic epi-on CXL leaves the epithelium intact and undisturbed, reducing postoperative pain, promoting faster visual recovery, and minimizing the risk of significant complications. The timing of this article is uncanny because my colleagues and I just published the results of a phase 2 clinical trial of one epi-on technique, EpiSmart CXL (CXL Ophthalmics [CXLO]).4 In animal models, the procedure has achieved and maintained an adequate and sustained concentration of riboflavin across an intact epithelium without supplemental riboflavin drops during UV-A exposure (Figure 2).5-7
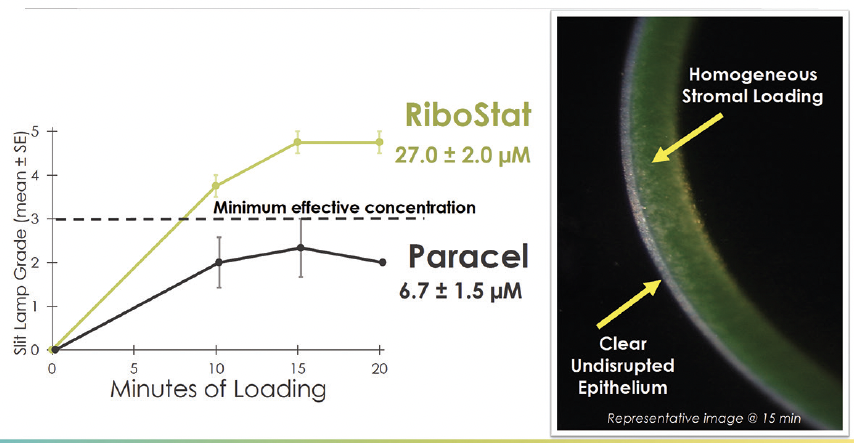
Figure 2. Comparative stromal riboflavin saturation in an animal model.6
STUDY DESIGN
In the phase 2 study, 2,228 patients with ectasia (1,922 with keratoconus) were randomly assigned to one of three UV-A treatment groups: 2.4 J/cm2 for 20 minutes, 3.6 J/cm2 for 20 minutes, or 3.6 J/cm2 for 30 minutes. All patients were treated with the EpiSmart CXL system with riboflavin 5’-phosphate 0.5% and sodium iodide 0.015% (RiboStat, CXLO) and pulsed UV-A light exposure in cycles of 15 seconds on/15 seconds off. An EpiPrep sponge was first used to remove lipids from the corneal surface without disrupting the epithelium, and a round loading sponge (CXLO) was saturated with riboflavin every 1 to 3 minutes until adequate corneal saturation was confirmed by the surgeon at a slit lamp. The corneal surface was then irrigated with artificial tears for 30 seconds before UV-A light exposure to minimize surface absorbance of riboflavin. Bilateral, simultaneous epi-on CXL treatment was performed on 1,315 patients (71%) with keratoconus using an investigational UV-A device (Figure 3).

Figure 3. Typical slit-lamp appearance after 15 minutes of loading in the EpiSmart study.
At both 6 and 12 months, in all groups, corrected and uncorrected distance visual acuity and maximum corneal curvature significantly improved in patients with keratoconus. BCVA and UCVA improved approximately 1 line at 6 and 12 months after treatment (P < .001–.0001), and maximum keratometry flattened. Minimum corneal thickness was unchanged. Compared with epi-off CXL for keratoconus, the incidence of adverse events was lower with EpiSmart epi-on treatment (Table 2), and most patients returned to their normal activities by the next day, confirming the results of earlier studies.8 The most common adverse event in our study was a mild corneal defect in the first postoperative week noted in 31 patients (1.4%)4 compared with 100% with epi-off CXL.9,10 EpiSmart epi-on CXL appeared to be safe and effective in patients with keratoconus in this large prospective study, meriting controlled further studies.
REDUCING THE GLOBAL BURDEN
About 1.4% of 20-year-olds in the developed world have keratoconus.11 In the developing world, it can be as high as 7%. The long-term global burden of keratoconus has been estimated to be greater than that of cataracts.12
I started working with William B. Trattler, MD, in 2008 and organized the world’s largest keratoconus research group, CXLUSA, with the goal of reducing the global burden of keratoconus by eventually developing an epi-on CXL treatment. This would represent a much-needed significant leap forward from what we currently use—the epi-off Dresden protocol, developed in the 1990s.13
An epi-on CXL treatment in combination with new awareness of how common the disease is and screenings starting in early school years has the potential to nearly eradicate keratoconus in the developed world. In the developing world, the treatment has the potential not only to increase patients’ quality of life but also decrease the burden of disease on their families, villages, and countries.
We are hopeful the wide availability of an effective epi-on CXL treatment will help increase utilization of CXL and reduce the global burden of keratoconus by making the procedure more patient and surgeon friendly.
1. Kobashi H, Rong SS, Ciolino JB. Transepithelial versus epithelium-off corneal crosslinking for corneal ectasia. J Cataract Refract Surg. 2018;44:1507-1516.
2. Nath S, Shen C, Koziarz A, et al. Transepithelial versus epithelium-off corneal collagen cross-linking for corneal ectasia: a systematic review and meta-analysis. Ophthalmology. 2021;128:1150-1160.
3. D’Oria F, Palazón A, Alio JL. Corneal collagen cross-linking epithelium-on vs. epithelium-off: a systematic review and meta-analysis. Eye Vis (Lond). 2021;8:34.
4. Epstein RJ, Belin MW, Gravemann D, Littner R, Rubinfeld RS. EpiSmart crosslinking for keratoconus: a phase 2 study. Cornea. Published online September 29, 2022. doi:10.1097/ICO.0000000000003136
5. Gore DM, O’Brart D, French P, Dunsby C, Allan BD. Transepithelial riboflavin absorption in an ex vivo rabbit corneal model. Invest Ophthalmol Vis Sci. 2015;56(8):5006-5011.
6. Rubinfeld RS, Stulting RD, Gum GG, Talamo JH. Quantitative analysis of corneal stromal riboflavin concentration without epithelial removal. J Cataract Refract Surg. 2018;44:237-242.
7. Rubinfeld RS, Gum GG, Talamo JH, Parsons EC. The effect of sodium iodide on stromal loading, distribution and degradation of riboflavin in a rabbit model of transepithelial corneal crosslinking. Clin Ophthalmol. 2021;15:1985-1994.
8. Stulting RD, Trattler WB, Woolfson JM, Rubinfeld, RS. Corneal crosslinking without epithelial removal. J Cataract Refract Surg. 2018:44:1363-1370.
9. Hersh PS, Stulting RD, Muller D, et al. United States multicenter clinical trial of corneal collagen crosslinking for keratoconus treatment. Ophthalmology. 2017;124:1259-1270.
10. FDA NDA 203324. Highlights of prescribing information—Photrexa viscous and Photrexa (Avedro). 2016. Accessed August 18, 2022. https://www.accessdata.fda.gov/drugsatfda_docs/label/2016/203324s000lbl.pdf
11. Chan E, Chong EW, Lingham G, Hewitt AW, Mackey DA, Yazar S. Prevalence of keratoconus based on Scheimpflug imaging. The Raine study. Ophthalmology. 2021;128(4):515-521.
12. Himalayan Cataract Project, Waterbury, Vermont.
13. Pérez-Santonja JJ, Artola A, Javaloy J, et al. Microbial keratitis after corneal collagen crosslinking. J Cataract Refract Surg. 2009;35(6):1138-40.




