Small eyes present unique challenges and risks during phacoemulsification, including endothelial injury, iris prolapse, a radialized capsulorhexis, malignant glaucoma, and suprachoroidal hemorrhage. A modified routine approach to phacoemulsification in these eyes is warranted.
SEVEN TIPS
My video (watch below) provides seven tips that I have found simplify surgery and reduce the risk of complications in small eyes.
No. 1: Mind the capsule. When creating the paracentesis, aim the blade slightly uphill (Figure 1) to avoid accidentally nicking the anterior lens capsule.
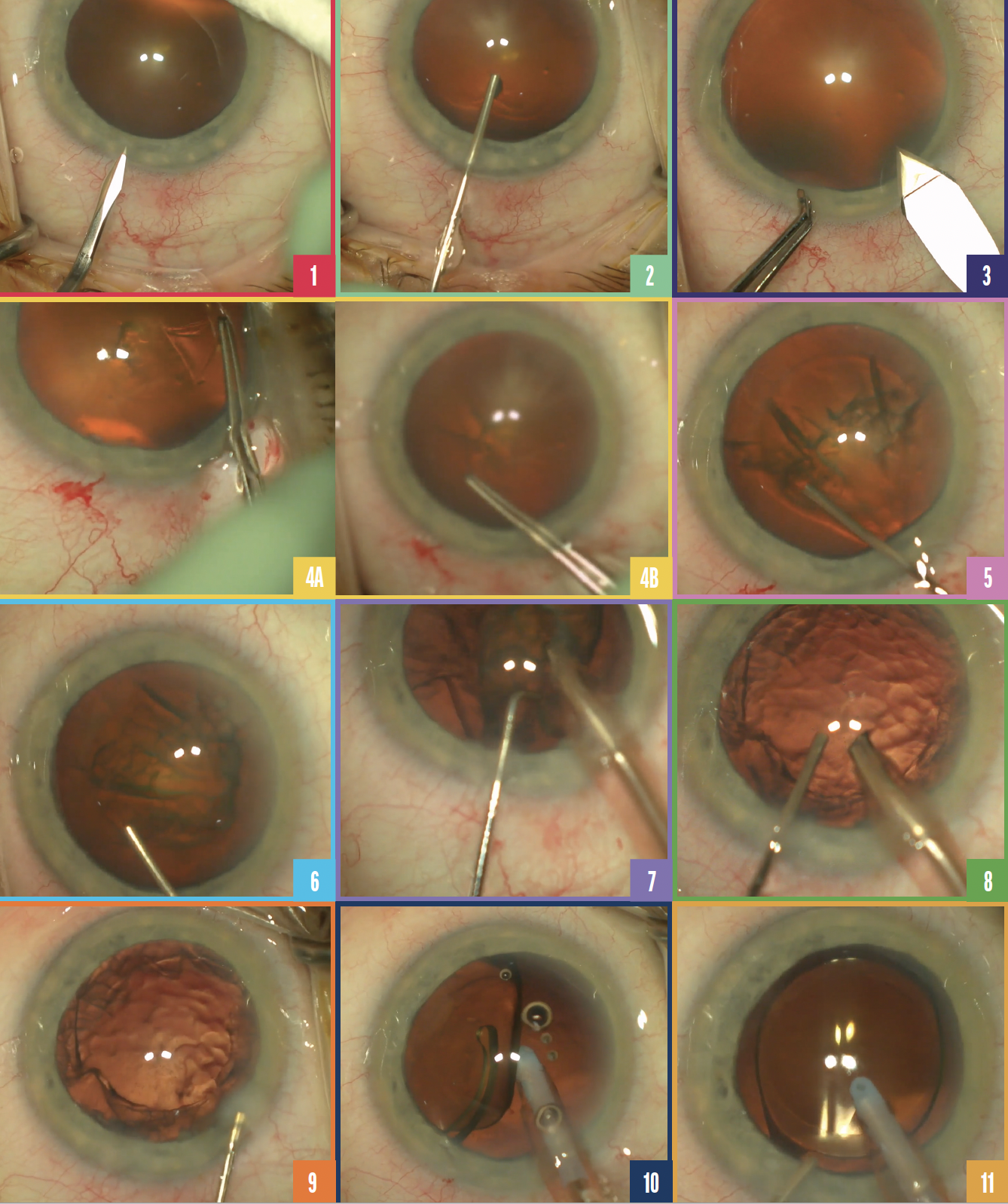
Figure 1. The paracentesis blade is positioned slightly uphill.
Figure 2. An adequate amount of OVD is used to inflate the anterior chamber.
Figure 3. Proper positioning of the main wound.
Figure 4. The capsulorhexis is created slowly to avoid radialization of the tear (A,B).
Figure 5. Blotting down gently with the hydrodissection cannula can aid OVD removal.
Figure 6. A dispersive OVD is injected before phacoemulsification commences.
Figure 7. Phacoemulsification is performed.
Figure 8. An OVD is injected to maintain the anterior chamber as the phaco handpiece is removed.
Figure 9. The wounds are prehydrated.
Figure 10. The OVD is removed from behind the IOL.
Figure 11. Balanced salt solution is injected as the I/A handpiece is removed.
No. 2: Resist the temptation to overfill the anterior chamber with an OVD (Figure 2). Overinflation to deepen the anterior chamber places stress on the zonules and can lead to iris prolapse.
No. 3: Take care with wound construction. The main wound must not be too short (< 2 mm) or too posterior (Figure 3). Both problems can increase the risk of iris prolapse.
No. 4: Exercise diligence when creating the capsulorhexis. The capsulorhexis is one of the most important early steps of cataract surgery. A well-constructed, properly sized capsulorhexis may allow IOL optic capture if complications arise. In small eyes with a shallow anterior chamber, forward lens vault can make the capsulorhexis prone to radializing or running downhill. The same is true of any eye with increased posterior pressure. Take your time when performing the capsulorhexis and add a cohesive OVD as needed to flatten the anterior lens (Figure 4).
No. 5: Maintain gentle hydrodissection. Small eyes present a high risk of iris prolapse, especially during hydrodissection. Use the hydrodissection cannula to gently and frequently blot the lens so that balanced salt solution does not build up behind the lens, vault the lens anteriorly, and result in iris prolapse (Figure 5).
No. 6: Protect the endothelium during phacoemulsification. I like to add an extra amount of a dispersive OVD just before initiating phacoemulsification to protect the endothelium (Figure 6). I often perform cataract surgery earlier in small eyes owing to angle closure, and these soft lenses require little ultrasound energy to remove (Figure 7). Nevertheless, it is good practice to perform endocapsular disassembly and keep the ultrasound energy as far from the endothelium as possible.
No. 7: Keep the chamber stable. In eyes prone to choroidal effusion or malignant glaucoma, chamber stability is crucial. After nuclear disassembly, inject OVD before the phaco handpiece is removed (Figure 8). Prehydrate the wounds while the scrub technician switches to irrigation and aspiration (Figure 9). This helps prevent the chamber from collapsing as instruments pass in and out of the eye toward the end of the case.
A cohesive OVD is injected again before the I/A handpiece is removed. After the IOL is implanted, the OVD is removed from behind the IOL (Figure 10). With final removal of the I/A handpiece, add balanced salt solution. This helps to maintain a stable chamber (Figure 11).