
Thanks to advances in phaco technology and techniques, there are few instances when surgeons cannot crack and emulsify a cataract. Just because they can, however, doesn’t mean they should.
The repeated instillation of a dispersive OVD can help protect the cornea, but reducing the amount of ultrasound energy used during surgery may be more important. Much of the energy is used when the initial groove is created to help crack a dense nucleus. I have had success with a stop and chop technique—even in moderately dense lenses—but I prefer to use the miLoop (Carl Zeiss Meditec) when I am concerned that a posterior plate may require increased surgical time and ultrasound energy.
DECREASING PHACO ENERGY: A CASE EXAMPLE
Use of the miLoop is associated with a statistically significant reduction in ultrasound energy,1 and the device can easily break through a posterior plate that would slow and complicate manual cracking. This was particularly helpful in the case of a 66-year-old man with high myopia and a dense brown/black posttraumatic cataract from a childhood injury. The patient had previously been told by another physician that cataract surgery would not be beneficial.
After a thorough examination, I explained to the patient that his postoperative visual acuity might be limited by retinal or optic nerve pathology. He decided to proceed with cataract surgery. Attachment of the retina was confirmed with B-scan ultrasonography.
My plan was to perform small-incision extracapsular cataract extraction and to divide the nucleus into multiple segments with the miLoop, which I hoped would allow me to use a small scleral incision.
Despite dividing the lens into four small pieces with the miLoop, phacoemulsification was difficult. I had made a small extracapsular incision but did not need to extend it to the full length—only to the width of the lens loop (Figure 1)—but enlargement of the clear corneal incision and proper placement of corneal sutures can be required. If I place limbal sutures, I start to remove them 2 to 3 weeks after surgery and have thus far managed to avoid inducing significant astigmatism.
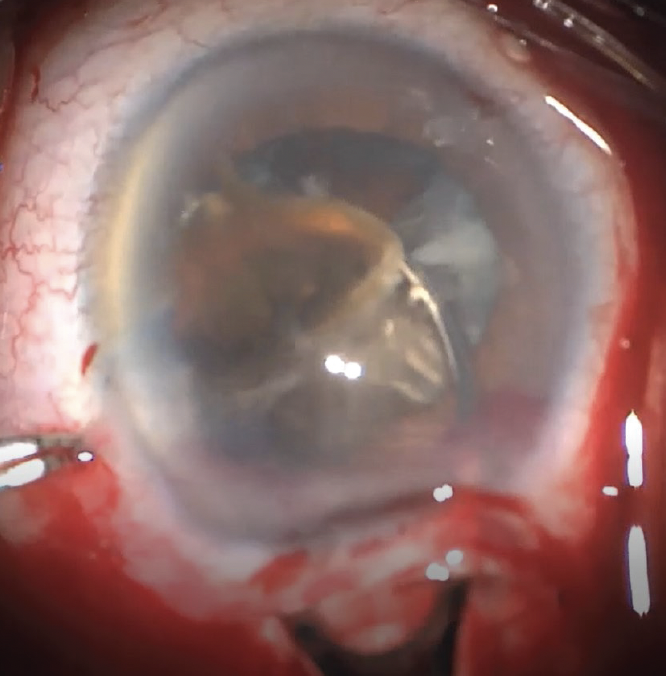
Figure 1. The lens loop is used to remove a dense cataract piece.
High myopia had caused some significant changes in the patient’s retina, but his postoperative UCVA was 20/100.
TIPS ON USING THE MILOOP
No. 1: Stain the capsule. Staining the capsule with trypan blue dye facilitates proper placement of the device. The nitinol filament is oriented in a snare and can be used to reach around the entirety of the lens and create a clean break between the two halves. The most recent version of the miLoop has a guard to prevent the instrument from being advanced too far into the eye.
No. 2: Prevent torque on the zonules. Perform thorough hydrodissection and make sure that the snare is opened to the greatest extent. It may look like it is distending the capsule (Figure 2). Sweep past the center of the lens and then back to the center before closing the snare to ensure the break is made in the middle of the lens (Figure 3). This can facilitate safe removal of the residual cortex during the posterior sweep of the miLoop.
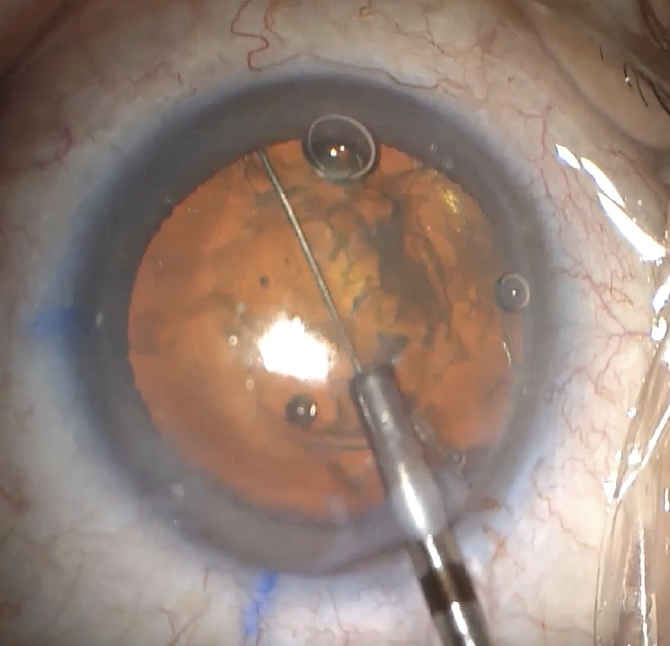
Figure 2. Full extension of the miLoop.
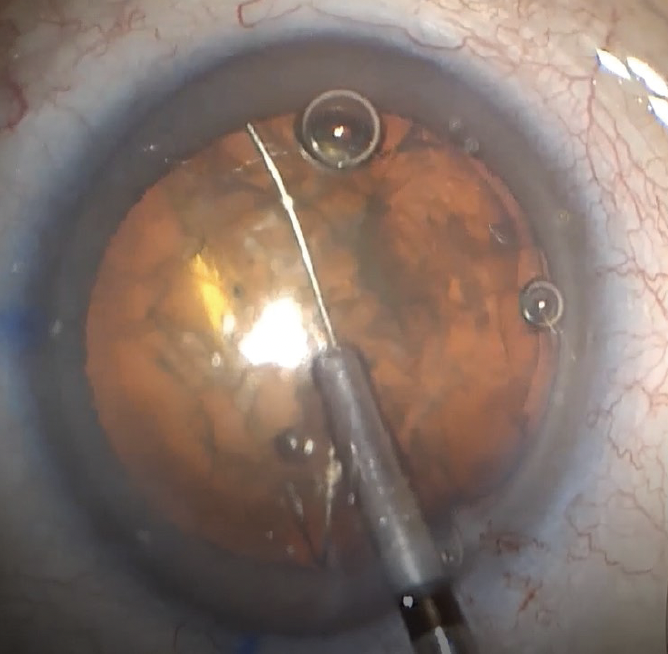
Figure 3. The miLoop extends past the equator.
No. 3: Carefully manage nuclear fragments. The use of a second instrument through the paracentesis can prevent the pieces from prolapsing into the anterior chamber. If further nuclear disassembly is required, a carousel technique can be helpful.2 Alternatively, the miLoop can be closed completely in the anterior chamber and the lens rotated about 70º because the device generally causes further rotation when deployed the second time (Figure 4). This should produce four quadrants that are similar in size.
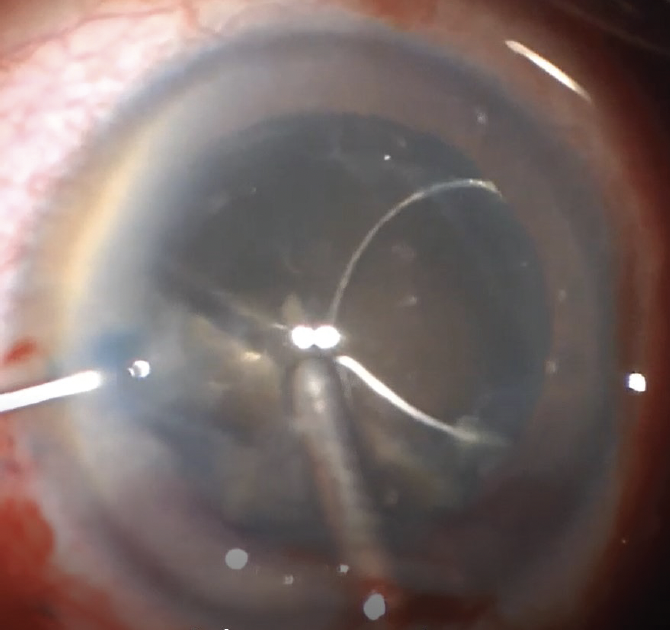
Figure 4. The use of the miLoop causes the lens to rotate.
CONCLUSION
In certain situations, use of the miLoop may help reduce the duration of surgery, the amount of ultrasound energy required, the patient’s recovery time, and the chances that the patient will need corneal surgery in the future.
1. Ianchulev T, Chang DF, Koo E, et al. Microinterventional endocapsular nucleus disassembly: novel technique and results of first-in-human randomised controlled study. Br J Ophthalmol. 2019;103(2):176-180.
2. Wiley WF, Bafna S, Logothetis HD. Comparative study of phacoemulsification parameters with and without nitinol filament nuclear disassembly. J Cataract Refract Surg. 2021;47(8):1028-1031.




