
I assess the type and density of the cataract at the slit lamp, and I continue the assessment during the first few steps of cataract surgery. At that point, I commit to an approach.
There are two reasons why I use a femtosecond laser (Lensar Laser System, Lensar) for all premium IOL cases. First, I believe the technology offers advantages for capsulorhexis creation and nuclear fragmentation. Second—and more importantly—the laser allows me to create steep axis indicators on the capsule and lens for toric IOL alignment or precisely positioned arcuate incisions.
For all cataract cases, I sit in a temporal position and make a paracentesis incision approximately 2 clock hours away from the main incision. A 19-gauge straight phaco tip and high vacuum promote efficient lens removal and reduce the amount of ultrasound energy required. My second-hand instrument of choice is a Fine Nichamin I Quick Double Chopper (Katena; Figure 1). This combination chopper features a rounded tip for general manipulation and horizontal chopping on one end and a sharper vertical chopper tip on the other.

Figure 1. A Fine Nichamin I Quick Double Chopper.
Figure 1 courtesy of Katena
TECHNIQUE NO. 1: TILT AND TUMBLE
For patients undergoing refractive lens exchange (usually 40–60 years of age) and those with soft cataracts, I favor the tilt and tumble technique described by Richard L. Lindstrom, MD.1
A 5.25- to 5.5-mm capsulorhexis is created. Gentle hydrodissection is performed in a controlled manner; the goal is to prolapse half of the nucleus out of the bag and allow it to tilt up onto its side. The hydrodissection cannula should be inserted through the main incision, and gentle and steady hydrodissection should be directed 90º away to one side so that the opposite side of the nucleus has enough room to pop out or tilt up toward the anterior chamber.
Hydrodelineation may then be performed to separate the endonucleus from the epinucleus. The phaco handpiece, preferably bevel down, is used to remove the most anterior portion of prolapsed nucleus first. This helps to create room in the anterior chamber for the remaining lens or nuclear pieces to tumble freely or cartwheel as they are aspirated (Figure 2). During aspiration and removal, manipulation with the second instrument maintains the tilted orientation of the lens and positions its edges or pieces to enter the phaco tip. Zero or minimal phaco energy is needed if high vacuum is used (see below to watch a video demonstration of the tilt and tumble technique).
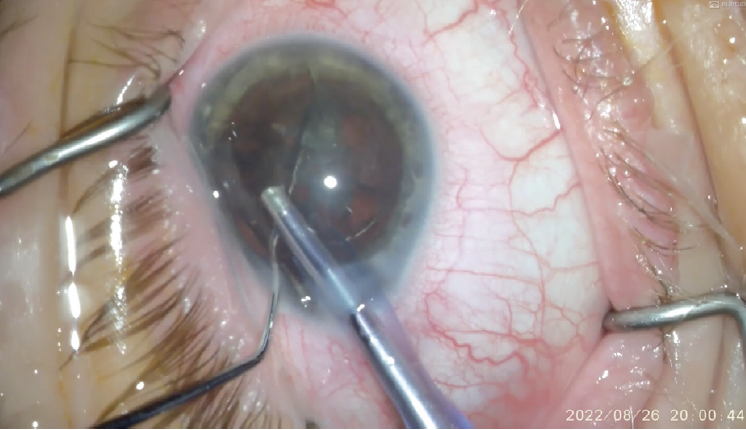
Figure 2. The phaco handpiece—bevel down—is used to remove the most anterior portion of prolapsed nucleus in the tilt and tumble technique.
Figures 2 and 3 courtesy of Joaquin O. De Rojas, MD
TECHNIQUE NO. 2: STOP AND CHOP
If the nuclear density of the lens requires more than minimal phaco energy (eg, ≥ grade 2+ nuclear sclerosis) and the nucleus can be cracked, I favor a simple stop and chop technique because it allows me to debulk the lens when I sculpt the center.
A 5- to 5.25-mm capsulorhexis is created. Thorough hydrodissection is performed by rotating the nucleus 1 or 2 clock hours before phacoemulsification is initiated. During sculpting, I find that achieving a depth equivalent to approximately 2.5 phaco tips increases the chances of a successful crack. If the lens is dense and the lens-bag complex moves during sculpting, I increase the phaco energy so that less translational force is placed on the zonules (see below for a video demonstration of the stop and chop technique). The red reflex through the sculpted area usually appears brighter—unless the patient has a dense posterior subcapsular cataract—once adequate sculpting depth is achieved.
Cracking the nucleus with both instruments within the groove is the crucial next step (Figure 3). Multiple attempts at cracking in two or three separate locations along the groove are sometimes required. The goal is to transect the posterior plate fully.
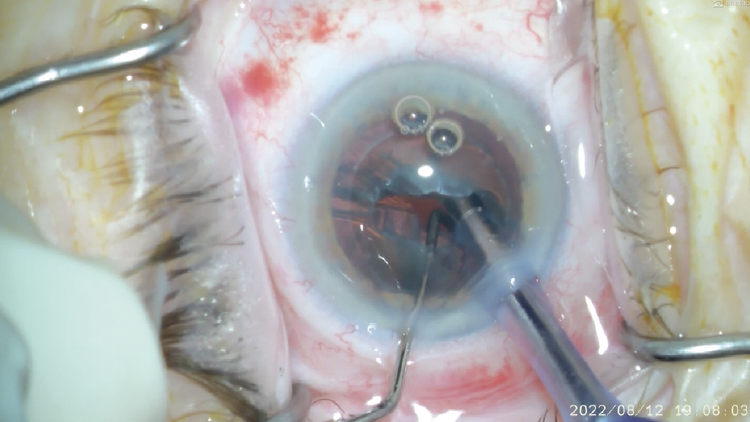
Figure 3. With both instruments deep within the groove, the nucleus is cracked in the stop and chop technique.
The first hemi-nucleus is engaged at the corner with high vacuum and brought up to the iris plane. Then, lens removal begins. During this phase of the technique, the phaco tip stays mostly in the center of the eye (roughly at the level of the mid-iris plane), and the blunt end of the chopper is used for micromanipulations of fragments and small horizontal chops as needed. Efficiency can be increased by using the instrument in the second hand to elevate and reorient lens fragments toward the phaco handpiece and to ensure that the lens fragment edges are free of physical obstructions (eg, from the anterior capsule or iris tissue). As the second hemi-nucleus is removed, the smooth portion of the chopper can be turned sideways and positioned just posterior to the iris plane to keep the posterior capsule away from the phaco tip and provide protection in the event of unexpected postocclusion surge.
TECHNIQUE NO. 3: VERTICAL CHOP
I begin with a stop and chop technique for dense nuclei but increase phaco energy if sculpting places too much stress on the zonules. If sculpting cannot be completed or the nucleus cannot be cracked despite increasing phaco energy, the sharp end of the chopper may be used for vertical chopping of the nucleus while it is held in place with phaco vacuum.
CONCLUSION
Fragmentation and removal of the nucleus is the step of cataract surgery that is perhaps the most nuanced and difficult to master, but it can also be one of the most rewarding. In the rare event that a brunescent or black cataract cannot be removed safely or efficiently with one of the techniques described here, I convert to manual small-incision cataract surgery.
1. Davis EA, Lindstrom RL. Tilt and tumble phacoemulsification. Dev Ophthalmol. 2002;34:44-58.




