Watch the latest episodes of the Innovation Journal Club series on Eyetube.

The MIGS category has undoubtedly changed the management of glaucoma. After more than a decade of use in clinical practice, the longer-term benefits associated with the procedural management of glaucoma are starting to emerge—and they appear to be substantial. In episode 7 of Innovation Journal Club, host I. Paul Singh, MD, sat down with Mark J. Gallardo, MD, to discuss long-term outcomes with canaloplasty and future trends in MIGS.
Long-Term Outcomes With Canaloplasty
A study by Dr. Gallardo and colleagues reporting the 3-year follow-up of patients who received canaloplasty and viscodilation (iTrack; Nova Eye Medical), with or without cataract surgery, for the treatment of primary open-angle glaucoma, demonstrated sustainable reductions in postoperative IOP and medication usage.1 The drop in medication requirement was slightly greater after combination procedures, but the difference was not statistically significant.
The mean IOP in both groups of patients was consistently in the range of 13 to 14 mm Hg at 12, 24, and 36 months postoperatively (Figure 1). A number of patients were able to stop all antiglaucoma medication use, again with a slight benefit for combination procedures: 42.9% in the overall population, 26.1% among those in the iTrack-only group, and 34.1% in the iTrack + cataract surgery group.
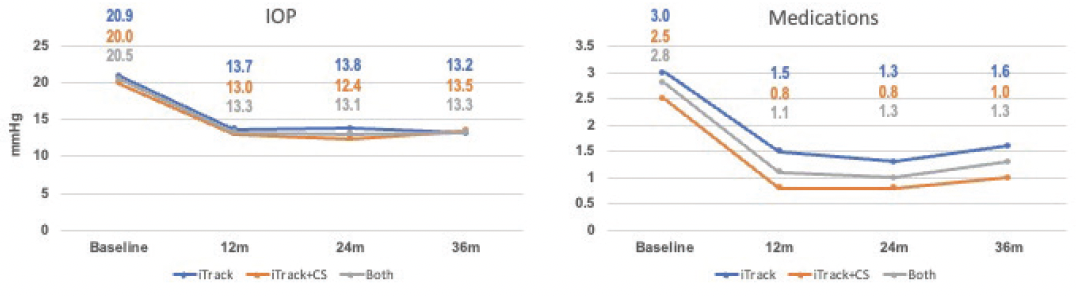
Figure 1. IOP and medication outcomes through 3 years of follow-up in a study led by Dr. Gallardo.
“In the past, when we thought about the definition of success, our complete success was meeting the target IOP with no medications. With a lot of the patients who we’re dealing with now going into cataract surgery and implanting a major device, the goal really is to eliminate the medication burden on a number of those patients,” Dr. Gallardo said.
According to Dr. Gallardo, the mechanism of iTrack—mechanical dilation and forceful viscodilation—likely explains the long-term effectiveness he observed. The canaloplasty portion of the procedure functions to mechanically break any herniations that might impede aqueous outflow in the Schlemm canal; viscodilation complements this mechanism by flushing the canal while also opening blockages in the juxtacanalicular tissue, trabecular meshwork, and within collector channels. In all, the procedure has an impact on all the relevant anatomy in the complex aqueous drainage system.
“What you want to be able to do is create enough force within the canal that the viscoelastic not only causes changes to the proximal system, but also dilates things downstream,” Dr. Gallardo said. “I really do think that the force of the viscoelastic that’s introduced has a significant role in the expansion and the microscopic changes to the tissue that occur.”
Trends in MIGS, 2013-2018
It is perhaps unsurprising that a study reviewing MIGS usage trends between 2013 and 2018 found a substantial increase in the number of procedures performed, with a corresponding decrease in the number of traditional incisional glaucoma surgeries during the same period (Figure 2).2
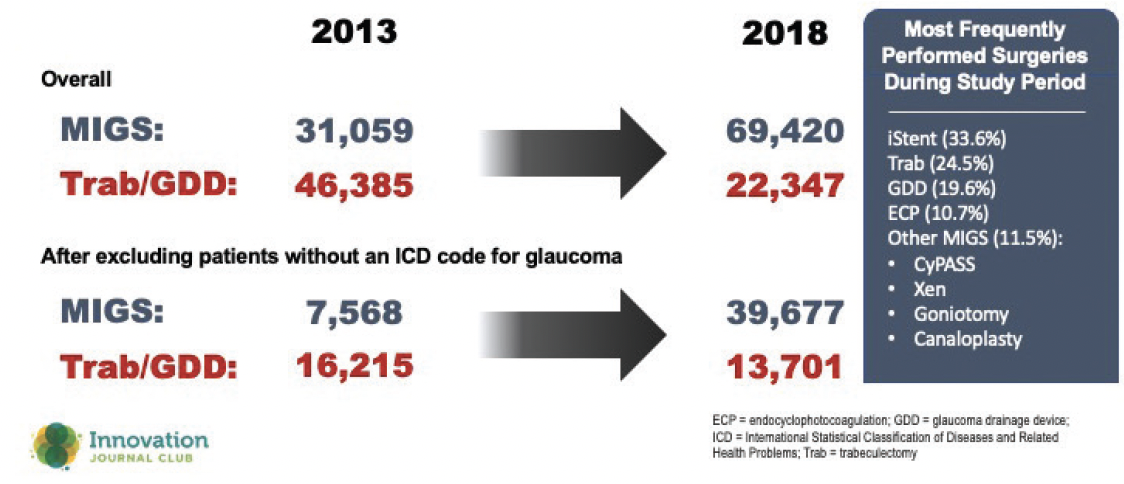
Figure 2. The volume of MIGS procedures increased 3-fold between 2013 and 2018, with a corresponding decrease in traditional incisional glaucoma procedures.
The shift may be explained by a number of factors. For instance, the availability of alternative options for surgically managing glaucoma, especially ones with a more favorable safety profile, should have organically reduced the number of trabeculectomy and tube surgeries performed year over year. Furthermore, that favorable safety profile has facilitated adoption by comprehensive ophthalmologists; the increase in provider base for procedural management, and expansion of this service beyond the sole purview of fellowship-trained glaucoma surgeons, also affects usage rates in the community.
And yet, there may be a much simpler explanation: MIGS procedures work.
“When I started practicing, I was doing about eight trabeculectomies a week, and now we probably do about 25 or 30 a year, and that’s because MIGS procedures have worked very well,” Dr. Gallardo said. “If there’s a question of longevity of MIGS procedures, I can tell not only anecdotally, but just by what I see day in and day out in the patients in my practice, that MIGS procedures have prevented patients from requiring filtration surgeries.”
Another trend revealed in the study of MIGS usage patterns was a growth in using combinations of MIGS procedures. Whether or not that is truly surprising may depend on one’s mindset in thinking about offering options to patients. Dr. Singh offered that using two or more devices or procedures, aimed at different anatomy within the drainage pathways, appears to have synergistic effects.
“We’re finding that combing procedures not only provides additional pressure reduction by maybe a point or two, but also provides greater medication burden reduction … and results in fewer nonresponders,” Dr. Singh said.
1. Gallardo MJ. 36-month effectiveness of ab-interno canaloplasty standalone versus combined with cataract surgery for the treatment of open-angle glaucoma. Ophthalmol Glaucoma. Published online February 17, 2022
2. Yang SA, Mitchell W, Hall N, et al; IRIS® Registry Data Analytics Consortium. Trends and usage patterns of minimally invasive glaucoma surgery in the united states: IRIS® Registry Analysis 2013-2018. Ophthalmol Glaucoma. 2021;4(6):558-568.


