CASE PRESENTATION
A 33-year-old man presented for a refractive surgery evaluation. The patient reported that he had a high prescription for his entire life and wished to reduce his dependence on contact lenses and glasses.
On examination, the patient’s BCVA was 20/20-2 with a manifest refraction of -16.50 -1.50 x 020º OD and 20/25+2 with a manifest refraction of -13.50 -2.00 x 090º OS. Pachymetry readings were 487 µm OD and 475 µm OS. The anterior chamber depth was 3.56 mm OD and 3.64 mm OS. Measurements of the white-to-white (WTW) distance in each eye with the Lenstar LS900 (Haag-Streit) were 13.34 mm OD and 13.31 mm OS. Regular astigmatism was found on topography, and the endothelial cell count in each eye was normal for someone his age.
The patient elected to undergo the bilateral implantation of a Visian Toric ICL (STAAR Surgical). Because surgery was performed before the EVO ICL (STAAR Surgical) became available in the United States, two laser peripheral iridotomies were performed on each eye before surgery. The IOLs were implanted, the one in the right eye oriented horizontally and the one in the left oriented horizontally and then rotated 3º per the indicated instructions to minimize residual astigmatism. No intraoperative complications occurred. Both implants are the largest available diameter (13.7 mm). One day after surgery, the IOLs appeared to be well positioned. The patient’s UCVA was 20/30 OD and 20/25 OS.
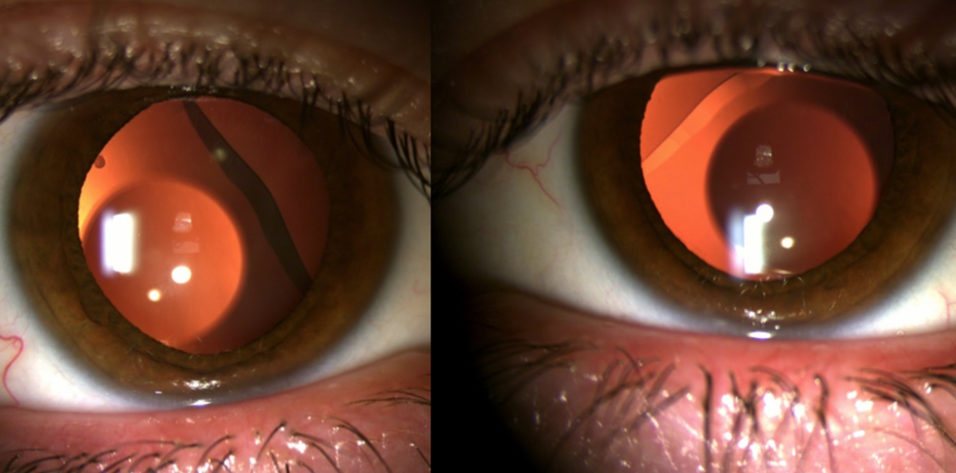
At 1 week, his visual acuity had not improved, and he reported worsening glare and halos. A dilated examination found that each ICL has rotated significantly, and inferior temporal displacement was observed (Figure 1).

Figure 1. Inferior displacement and rotation of the sulcus-stabilized Visian Toric ICL in each eye.
How would you proceed? What would you offer for the correction of the patient’s refractive error?
—Case prepared by Michael D. Greenwood, MD, and Seth Stofferahn, OD

IVAN GABRIĆ, MD
Daily practice includes what I refer to as fringe cases. This phrase is not a pejorative. Rather, the cases are so out of the ordinary that they prompt calling to a colleague down the hall, “Hey, you’ve got to see this!”
What struck me the most about this case is the impressive figures. The case notes, however, make clear what happened. Most refractive surgeons encounter a patient with measurements that fall outside the standard dimensions. In this situation, I tend to deliver what I call the three numbers talk.
“Our eyes are defined by three numbers,” I tell the patient. “Axial length is the most important factor in the refractive errors of myopia and hyperopia. The second number is corneal power and size, and the third number is lens power and accommodation. We can change only two of these numbers because it’s impractical to shorten or elongate your eye.” Usually, these remarks elicit a few giggles, but they also allow me to set reasonable expectations. My point is that the three numbers talk provides a frame of reference.
My training focused on two things for ICL candidacy: the correct manifest refraction and selection of the proper lens size. The ICL is available in four sizes—12.1, 12.6, 13.2, and 13.7 mm. WTW distances of less than 10.5 mm and greater than 12.9 mm are out of bounds. The patient was never a good candidate for the procedure because both WTW distances are 13.3 mm. Rotation of the ICLs and early cataract formation were all but guaranteed.
In a situation like this, if the individual requires a permanent refractive solution, I offer to implant a Verisyse IOL (Johnson & Johnson Vision) regardless of the patient’s age. When properly executed, iris capture of the IOL can provide a safe and permanent solution for phakic patients with good accommodation. If, however, the patient has even moderate presbyopia, I would offer refractive lens exchange as a permanent solution.
I would schedule the patient for removal of the ICLs as soon as possible because he is at high risk of cataract formation.
Good surgical outcomes are not the result of great surgery alone. They are more often the result of proper patient selection. With the availability of anterior segment OCT and clear instructions for use, situations like the one described should no longer occur.

LUKE REBENITSCH, MD
Rotation and displacement are known complications of ICL surgery. Sizing can be challenging, especially with the multitude of sizing modalities and associated nomograms. I have found that following the directions for use sizing nomogram provided with STAAR’s online calculation and ordering system often results in an overvault. I prefer to use the alternate optimized WTW nomogram or a sulcus-to-sulcus nomogram based on OCT or ultrasound biomicroscopy. Nearly every WTW sizing nomogram would have recommended the largest available ICL size (13.7 mm) for the patient. Rotation and displacement of the ICL are typically associated with an ICL that is a size too small or, rarely, one that was not positioned correctly. In these instances, the ICL can be exchanged for a larger size or simply repositioned. Unfortunately, a larger size is not available for this patient, and laser vision correction is not an option if the ICLs are explanted.
I would consider repositioning the phakic IOLs or exchanging them for spherical ICLs or iris-fixated lenses. If choosing an ICL exchange surgery, I would confirm that the two peripheral iridotomies were patent. Bioptic laser vision correction for residual astigmatism can be performed 2 to 3 months after surgery on the left eye. If the ICL in the right eye becomes displaced again and causes a visual disturbance, the lens may have to be explanted and potentially replaced with an iris-fixated lens. Thankfully, many patients in this situation continue to tolerate their vision and may simply be observed.

EVAN D. SCHOENBERG, MD
A Visian Toric ICL would have been my preferred approach for the initial management of the patient. The large WTW distances (13.34 mm OD and 13.31 mm OS) make this an off-label use of the ICL; the directions for use specify a WTW distance of less than 13 mm. The inferotemporal displacement of the lens bilaterally despite the use of the largest available size suggests that there may be a fundamental disconnect between the patient’s ocular anatomy and the available lens sizes.
Rotation of an implanted ICL is quick and easy. After counseling the patient that rotation may recur, I would reposition the ICLs in hopes of achieving stability and avoiding an IOL exchange. I would reposition the ICL to a horizontal orientation in the right eye and to 3º in the left eye per the implantation orientation diagram. Gentle pressure applied to the periphery after removal of the OVD might facilitate seating of the ICL’s footplates in the sulcus. If either ICL rotates again, it would be exchanged for a Verisyse IOL. A 6.2-mm incision would be made in clear cornea on the steep axis (110º OD and 180º OS) to reduce the astigmatism. Once refractive stability is documented, any remaining astigmatism would be corrected if necessary, most likely via a limbal relaxing incision.


WHAT WE DID: MICHAEL D. GREENWOOD, MD, AND SETH STOFFERAHN, OD
The anterior chamber of each eye proved too large to provide stability for a Visian Toric ICL. Leaving the implant in place could have led to early cataract formation and other problems including unsatisfactory vision and angle-closure glaucoma. We had used the largest-diameter ICL available, so we had no choice but to look for other options.
Before the original surgery, we were concerned that the ICL would not fit properly because of the large WTW distance in each eye. That said, there is no established ceiling on the anterior chamber width for one of these lenses. Both ICLs were explanted without complication and replaced with an iris-fixated phakic IOL (Verisyse, Figure 2) because it is less dependent on ocular parameters than the sulcus-fixated Visian Toric ICL. At his most recent follow-up visit, the patient’s UCVA was 20/20 OU.
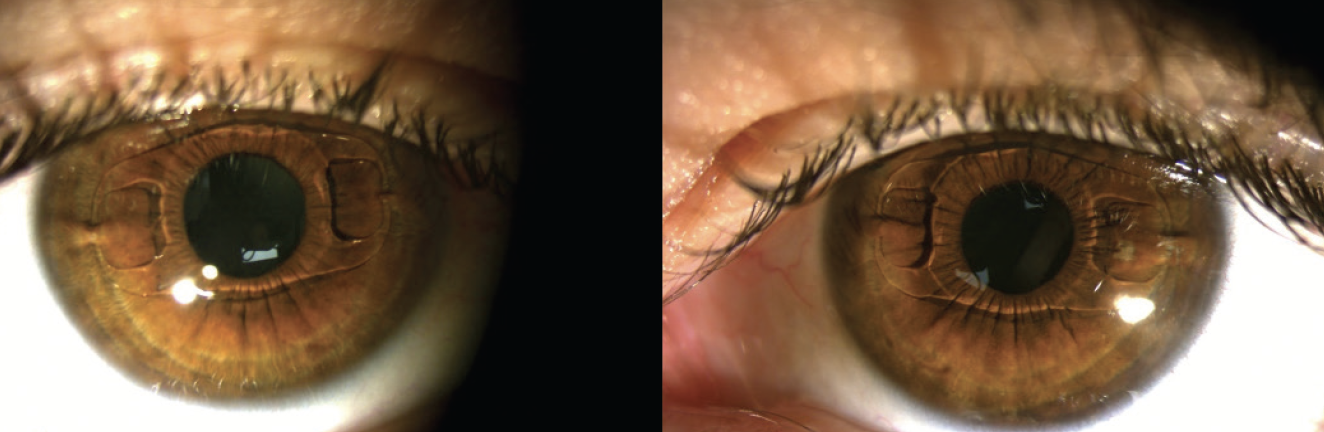
Figure 2. Iris-fixated Verisyse IOLs placed in the anterior chamber of each eye.
As a sidenote, one of us (M.D.G) underwent the bilateral implantation of a Visian ICL in 2015 and remains extremely happy with the result.