Lens subluxation is defined as a partial deviation of the lens from its original position with a pathologic mechanism involving partial zonular dehiscence. The anterior chamber angle of an eye with anterior lens subluxation is often narrow, mimicking primary angle-closure disease. Because of increased iridolenticular contact, a subluxated lens can precipitate acute angle closure via a pupillary block mechanism. Patients with undiagnosed anterior lens subluxation may experience repetitive appositional angle closure due to the mobility of the lens, which can permanently damage the anterior chamber angle. Studies have shown that between 4% and 21% of patients diagnosed with primary angle-closure glaucoma had anterior lens subluxation and were initially misdiagnosed.1-3
Anterior lens subluxation is typically managed with surgical intervention. Cataract surgery on these eyes, however, is frequently associated with a high rate of complications, especially if the operation is performed without a plan that takes the subluxation into account. Accurate detection of the condition is therefore important to successful management.
DIAGNOSTIC CHALLENGES
The diagnosis of lens subluxation is straightforward when phacodonesis, significant tilting or decentration of the lens, or the presence of vitreous in the anterior or posterior chamber is detected at the slit lamp. A history of hereditary disorders (eg, Marfan syndrome) and globe injury is typical in patients with lens subluxation. Disease manifestation, however, can be occult for several reasons.
No. 1: Lack of phacodonesis. Eyes with a subluxated lens can develop posterior synechiae, either at the pupillary border or behind the iris, precluding phacodonesis. This is more likely to occur in eyes with a history of an acute angle-closure attack.
No. 2: Subtle findings. Tilting or decentration of the lens can be subtle and difficult to detect at the slit lamp.
No. 3: Zonular integrity. Vitreous presents in the anterior chamber only if a large amount of the zonules have been lost.
No. 4: No stated history of trauma. A history of ocular trauma can help to narrow the differential diagnosis, but the information is frequently unreliable because it depends on the patient’s memory. Moreover, lens subluxation can develop spontaneously in the absence of trauma.
TIPS FOR DIAGNOSIS
No. 1: Refractive status. Information on the patient’s refractive status can indicate possible occult anterior lens subluxation. An eye with angle closure is usually hyperopic. Moderate to severe myopia is uncommon in this situation but, if present in an eye with a narrow angle and normal lens thickness, should raise a suspicion of anterior lens subluxation.
No. 2: Phacodonesis. Lens shaking in response to eye movement is the most important warning sign during the slit-lamp examination. Phacodonesis is more prominent when the pupil is undilated because there is less stress on the remaining undamaged zonular fibers, but displacement of the lens equator is more noticeable when the pupil is dilated. Full dilatation of the pupil, however, may inadvertently increase the IOP owing to worsening pupillary block or complete lens dislocation into the anterior chamber.
Assessing the center of the lens with reference to the center of the cornea is a simple and effective method of detecting subtle lens decentration. A helpful marker is a Y suture positioned at the center of the lens. If the Y suture is off axis, it indicates that the lens is decentered (Figure 1).
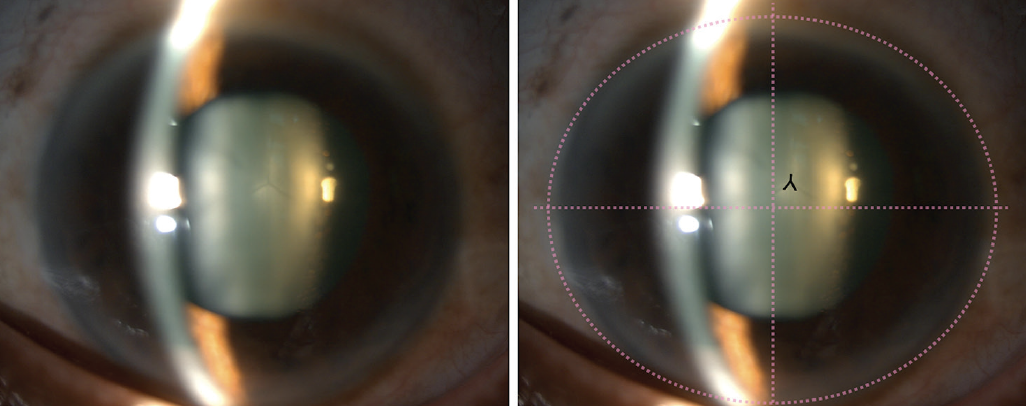
Figure 1. Slit-lamp photographs of a patient with a history of acute angle-closure attack show the superior displacement of the lens’ Y suture. The inverted Y shows the location of the Y suture. The dotted line represents the center of the cornea.
No. 3: Anterior chamber depth. The depth of a narrow anterior chamber must be carefully assessed. Uneven anterior chamber depth (ACD) in a single eye indicates lens tilt. A discrepancy in ACD between a patient’s eyes suggests lens subluxation. It can be difficult to detect ACD signs, however, when the degree of asymmetry is not substantial or there is underlying primary angle-closure disease, which is common among people of Asian descent. In this situation, the eyes’ biometric characteristics can aid diagnosis. Lens subluxation should be considered if the ACD is less than 1.8 mm or if the asymmetry in ACD between eyes is greater than 0.2 mm.4
No. 4: Relative lens position. In a study of patients with a history of angle-closure attack, the eyes with less hyperopia, a shallower anterior chamber, and longer axial length (AL) were more likely to have subclinical zonular instability.1 The aforementioned characteristics reflected that the lens was more anteriorly located relative to the size of the eye. The relative lens position (RLP) is an ocular biometric parameter that can quantify these traits.
The RLP, representing the relationship between LP and AL, can be calculated as follows: RLP = LP/AL x 10, where LP = ACD + 0.5 of the lens thickness. Angle closure from anterior lens subluxation is usually associated with a lower RLP than other angle-closure mechanisms. An RLP of 1.8 and lower suggested anterior lens subluxation in two studies.5,6
No. 5: Advanced imaging. Ocular imaging such as OCT or ultrasound biomicroscopy may be used to diagnose occult lens subluxation. The latest anterior segment OCT (AS-OCT) devices can capture the entire depth of the lens in three dimensions, which can help to determine the LP. This is especially useful for detecting a minor lens tilt. AS-OCT can also be used to detect decentration when the slit-lamp technique of locating a Y suture is not possible, such as in an eye with a dense cataract (Figure 1).
No. 6: No diagnosis. Anterior lens subluxation may remain undiagnosed in some instances despite the use of the techniques described herein. Consideration of the condition is warranted when a patient’s clinical findings fluctuate between visits. Variation in the individual’s visual acuity between visits due to refractive changes and changes in ACD associated with high intervisit IOP fluctuation suggest the presence of a mobile lens (Figure 2).
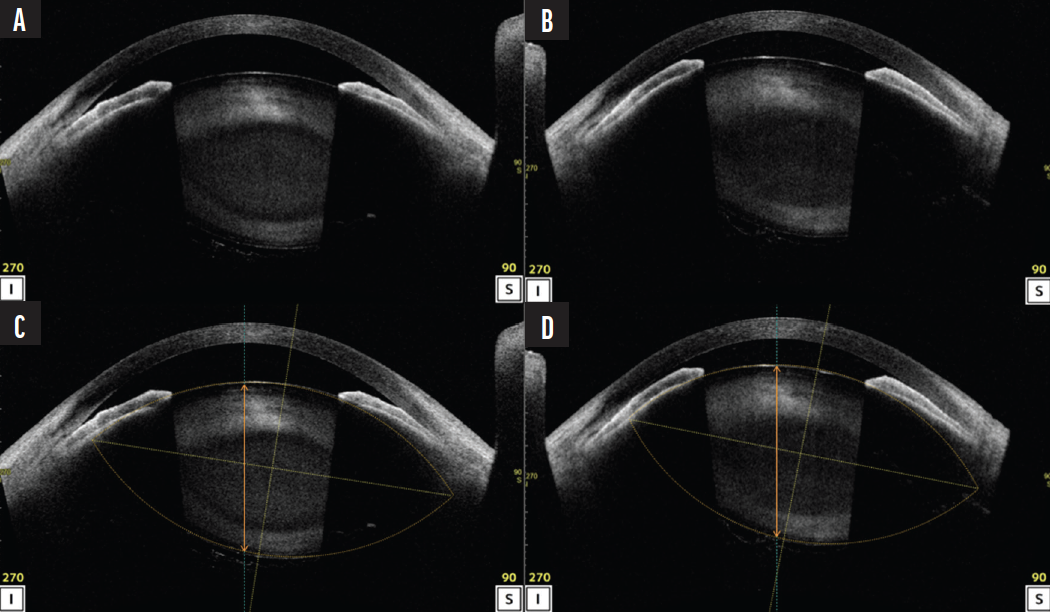
Figure 2. AS-OCT images demonstrate tilt and superior decentration of the lens. A and B are the original images; C and D are lens analysis reports showing the outline and center of the lenses. The original images and the lens analysis reports were obtained 1 month apart. The images in B and D reveal a shallower anterior chamber and greater lens tilt compared to the images in A and C.
CONCLUSION
Anterior lens subluxation can be misdiagnosed as primary angle-closure disease. A detailed examination of the anterior chamber and LP can facilitate the detection of occult anterior lens subluxation. Certain ocular biometry parameters and anterior segment imaging may be used as adjunctive diagnostic methods.
1. Kwon J, Sung KR. Factors associated with zonular instability during cataract surgery in eyes with acute angle closure attack. Am J Ophthalmol. 2017;183:118-124.
2. Luo L, Li M, Zhong Y, Cheng B, Liu X. Evaluation of secondary glaucoma associated with subluxated lens misdiagnosed as acute primary angle-closure glaucoma. J Glaucoma. 2013;22(4):307-310.
3. Zhang Y, Zong Y, Jiang Y, Jiang C, Lu Y, Zhu X. Clinical features and efficacy of lens surgery in patients with lens subluxation misdiagnosed as primary angle-closure glaucoma. Curr Eye Res. 2019;44(4):393-398.
4. Teekhasaenee C, Ritch R. Goniosynechialysis. In: Hong C, Yamamoto T, eds. Angle Closure Glaucoma. Kugler Publications; 2007:239-248.
5. Suwan Y, Jiamsawad S, Tantraworasin A, Geyman L, Supakontanasan W, Teekhasaenee C. Qualitative and quantitative evaluation of acute angle-closure mechanisms. BMC Ophthalmol. 2017;17(1):246.
6. Xing X, Huang L, Tian F, et al. Biometric indicators of eyes with occult lens subluxation inducing secondary acute angle closure. BMC Ophthalmol. 2020;20(1):87.