
Ocular surface disease is a wide category of clinical entities. In the majority of cases, the manifestations at the surface of the eye are caused by a local inflammatory reaction. Thus, the exact etiology may not always be consequential for how the patient is treated. However, a wide assortment of systemic conditions can contribute to dry eye and other ocular surface diseases, which in turn requires a more holistic approach to both gain control at the ocular surface and to address the underlying cause of the imbalance.
Background and Treatment
A 12-year-old girl was referred to our clinic with a history of night blindness for about a month. On examination, her conjunctiva looked extremely dry, and the cornea was hazy with a normal fundus (Figure 1). Schirmer testing demonstrated 1 mm OD and zero mm OS. She had a history of recurrent diarrhea. The young age coupled with night blindness and gastrointestinal symptoms raised our suspicion for nutritional deficiency. Another important thing to be noted in the history was that the patient had lost her mother a few months earlier and was being taken care of by a single parent. Based on the history, the patient was referred to a pediatrician, was subsequently diagnosed with low weight for her age and other nutritional deficiencies (including Vitamin A deficiency), and was started on treatment. One month after starting treatment, the patient’s cornea was clear (Figure 2), the conjunctiva looked relatively healthy, Schirmer testing demonstrated 7 mm OD and 5 mm OS, and she did not have any night blindness.
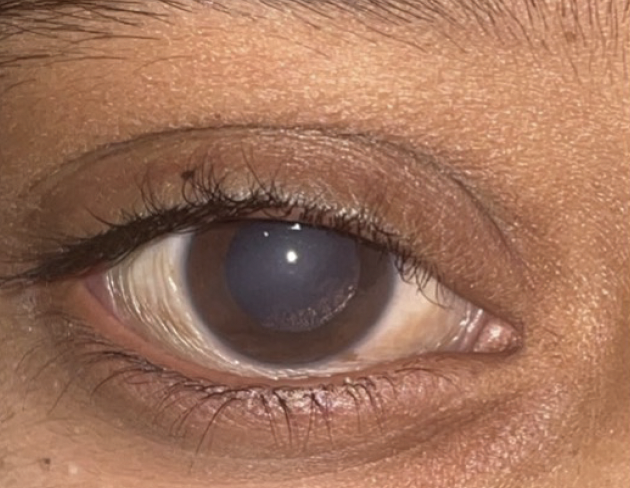
Figure 1. Ocular surface disease, coupled with gastrointestinal symptoms and a history of night blindness, raised our suspicion for nutritional deficiency.

Figure 2. Treatment of the underlying nutritional deficiency led to resolution of signs of ocular surface disease.
Discussion
Ocular surface disease often requires active treatment by the ophthalmologist to reverse signs and to provide the patient relief from symptoms, which can be severe and sight-threatening. In other instances, though, corneal findings are limited, resolving after treatment for the underlying systemic cause.
The link between vitamin A deficiency and ocular morbidity is well known, and it is a major cause of childhood blindness in developing countries. Vitamin A deficiency occurs when body stores are exhausted and supply fails to meet the body’s requirements, either because there is a dietary insufficiency, requirements are increased, or because intestinal absorption, transport, and metabolism are impaired.1 Early ocular changes associated with vitamin A deficiency include keratinization of the conjunctiva and development of superficial punctate keratopathy, and later characteristics include corneal keratinization, ulceration, and necrosis.2 The younger the child, the more severe the disease and the higher the risk that corneal destruction will be followed by death.1 Additional evidence for the role of micronutrient deficiency in ocular surface disease etiology and pathophysiology may be extrapolated from the positive therapeutic effects associated with nutritional supplementation (ie, omega-3 essential fatty acids) in resolving signs and symptoms.3
The current case highlights the correlation of nutritional deficiency with ocular surface disease. The fact that the keratinization resolved without direct treatment—that it resolved after addressing the nutritional deficiency—provides strong evidence that the patient’s poor tear film was something more insidious than standard dry eye. Of note, while the prevalence of ocular surface disease secondary to vitamin A deficiency is classically higher in developing nations and resource-poor areas, it is being increasingly recognized in vulnerable populations in the developed world, as well.4 Any report of unresolving gastrointestinal illness in a patient with hazy cornea on examination, especially in very young children who look small for their age, warrants special consideration for possible nutrient deficiency.
Declaration of patient consent
The author certifies that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be used. Participating patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
1. DeMaeyer EM. The WHO programme of prevention and control of vitamin A deficiency, xerophthalmia and nutritional blindness. Nutr Health. 1986;4(2):105-12. doi: 10.1177/026010608600400206. PMID: 3090484.
2. Sommer A. Effects of vitamin A deficiency on the ocular surface. Ophthalmology. 1983;90(6):592-600.
3. Pellegrini M, Senni C, Bernabei F, et al. The role of nutrition and nutritional supplements in ocular surface diseases. Nutrients. 2020;12(4):952.
4. Lin P, Fintelmann RE, Khalifa YM, et al. Ocular surface disease secondary to vitamin A deficiency in the developed world: it still exists. Arch Ophthalmol. 2011;129(6):798-804.


