
Neurotrophic keratitis (NK) is a degenerative corneal disease typified by reduction or loss of corneal sensitivity.1 Several potential causes have been identified, including infections, corneal pathologies, topical medications, 5th cranial nerve palsy, systemic diseases, and iatrogenic etiology. Of note, contact lens abuse is frequently cited as a cause of NK, which may refer to not following correct wearing and cleaning procedures, or very long duration of use.2 In some instances, testing corneal sensitivity to rule in/out NK is justified by the results of the clinical examination: any recalcitrant punctate keratitis or unresolved severe dry eye should be carefully investigated. However, the patient interview is just as important for unmasking suspicious findings that lead to additional work-up.
Case Information
A 70-year-old patient presented to our practice for cataract evaluation due to decreased vision OS>OD. During the consultation, superficial punctate keratitis (SPK) OS was observed, and the cataract surgeon referred him internally to my dry eye clinic for further evaluation. Corneal staining showed 3+ SPK OS and punctate erosions, and clinical examination revealed MGD 2+ OU (Figure 1). The patient was using Lotemax and artificial tears. His VA was 20/25 OD and 20/70 OS. During the interview, the patient said he had been wearing monovision contact lenses for more than 35 years. He subsequently revealed that he had been prescribed various treatments for dry eye by another optometrist, including multiple doses of steroids and different dry eye drops, all with no discernible effect. Corneal sensitivity was tested with a cotton swab, revealing decreased corneal sensitivity in all but the superior quadrant.
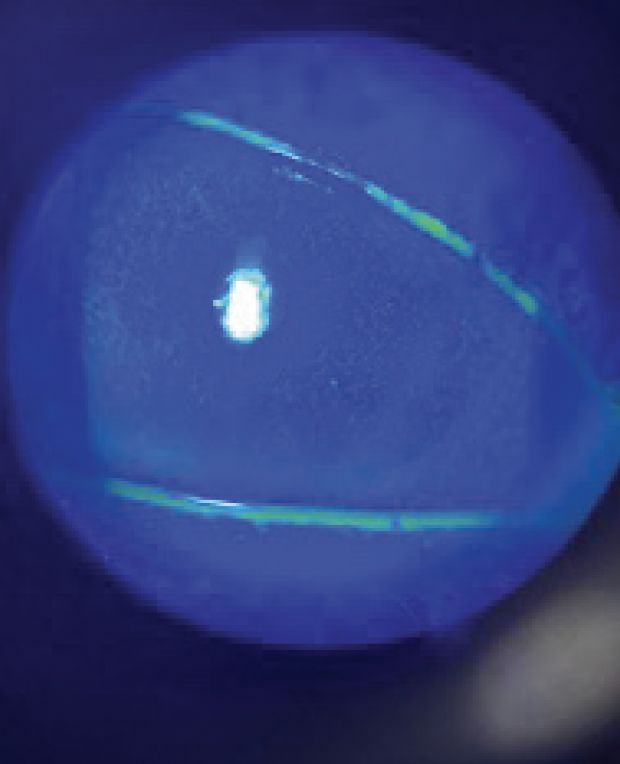
Figure 1. Corneal staining showed 3+ SPK OS and punctate erosions.
Based on the totality of the clinical evidence, the patient was diagnosed with NK, likely secondary to his long duration of contact lens wearing. The patient was started on Oxervate (Dompé) 6 times per day for 8 weeks. VA was 20/20 OS after the treatment and repeat corneal staining suggested a healthy cornea (Figure 2).
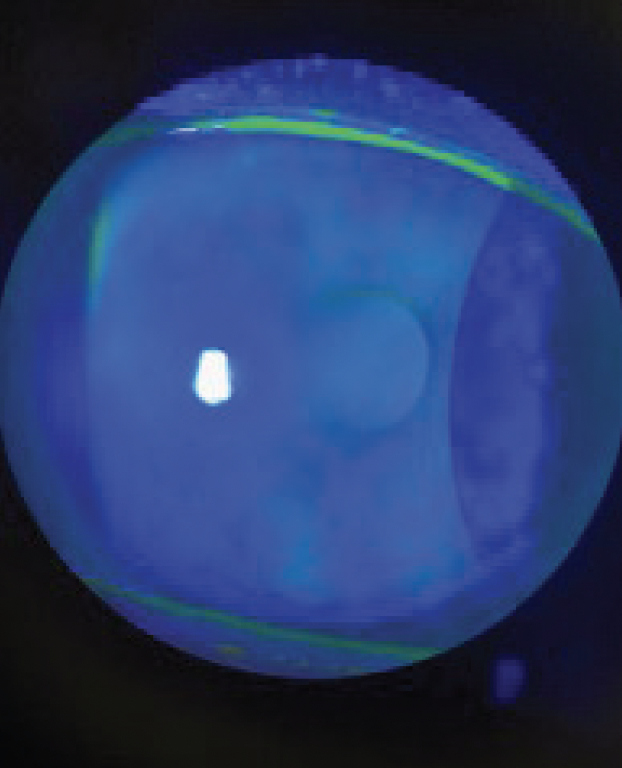
Figure 2. The cornea is clear after 8 weeks of treatment.
Discussion
Sometimes a good diagnosis is the result of asking the right question. In this case, one question unearthed a wealth of useful information. When I asked who had referred him for cataract surgery, the patient responded that he had been visiting his regular eye doctor around every 4 weeks and had tried numerous treatments for painful and irritating dry eye. His unexplained vision loss prompted a surgical consultation, but it is what he said in my examination chair that caused me to retrieve a cotton swab and test for corneal sensitivity. That information, combined with an impression that the vision changes didn’t match his cataract, led me to suspect NK.
There is some selection bias in the case presented here. As a specialist in dry eye disease, I may see more patients in my clinic with undiagnosed NK than a community optometrist. That said, NK is an undertreated and likely underdiagnosed clinical entity, despite its potential for severe visual complications. I have personally become more attuned to thinking about NK since Oxervate was released. In my experience, when I have a patient with recalcitrant SPK, unresolving dry eye despite treatment, and progressing signs, it takes very little effort to quickly test corneal sensitivity. A neurotrophic cornea is a hallmark finding in NK.3
Contact lens suspension is not mandatory while patients are being treated for NK. The clinician needs to make a judgement call on whether continued contact lens use while on treatment could prolong healing. However, contact lens wearing is not contraindicated with the use of Oxervate. This patient decided he would wear glasses during the 8 weeks of treatment, which was encouraging, and then he resumed wearing contact lenses. I will continue to follow this patient to monitor for corneal changes. Any recurrence might suggest that the contact lens was the insult and therefore needs to be stopped permanently.
1. Semeraro F, Forbice E, Romano V, et al. Neurotrophic keratitis. Ophthalmologica. 2014;231:191-197.
2. Sacchetti M, Lambiase A. Diagnosis and management of neurotrophic keratitis. Clin Ophthalmol. 2014;8:571-579.
3. Feroze KB, Patel BC. Neurotrophic keratitis. 2021 Nov 2. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022. PMID: 28613758





