
Aesthetic surgery has always been part of my practice and part of ophthalmology in general. Most ophthalmologists learn how to do at least some aesthetic procedures in training—namely, upper and lower eyelid blepharoplasties. Then, depending on the interest level of the doctor, he or she can either continue using this training by incorporating aesthetics into practice or give it up.
I enjoyed doing aesthetic surgeries in my residency. I treated a lot of shock trauma during my residency at the University of Maryland, and we worked in two Veterans Affairs hospitals, so I did a lot of blepharoptosis and reconstruction repairs. When I finished my fellowship in anterior segment surgery at the University of California, Irvine, I decided not to give it up.
Starting Out
When you begin to incorporate aesthetics into your practice, upper blepharoplasty and botulinum toxin injections are good procedures to start with. These treatments are straightforward, and, if you didn’t have training in blepharoplasty, a variety of courses are offered. It’s up to you how comfortable you are doing it.
Iris Color Change
By Marguerite B. McDonald, MD, FACS

Strōma Medical has perfected a way to change eye color safely and permanently using the Strōma Laser System (Strōma Medical; Figure). It may sound to some like a frivolous thing to do, but people all over the world have spent countless millions of dollars on colored contact lenses and even artificial iris implants, which are well known to be highly risky.
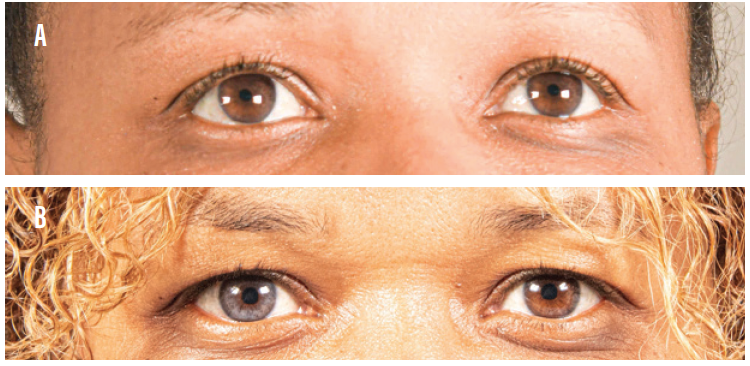
Figure. A patient’s eyes before receiving treatment with the Strōma Laser System (A). The same patient after receiving five treatments to the left eye and one to the right eye (B).
Courtesy of Stro-ma Medical
How it Works
The Strōma Laser System can make dark eyes lighter, transforming them to various shades of blue, green, and gray. The laser uses a frequency-doubled Nd:YAG laser (532-nm wavelength) to raise and lower the temperature of the anterior iris pigment 15 times over 30 seconds, which stimulates pigment on the anterior surface of the iris and triggers a cytokine and macrophage response. The macrophage response takes up to 3 weeks to carry away the pigment via the vascular system, exposing the stromal fiber.
The iris color change is done in stages. When the patient walks out after the first treatment, his or her iris looks the same. It takes up to 3 weeks for the color change to become apparent.
Safety and Efficacy
In a pilot study of this technique and technology, a one-eighth segment of one eye of each patient’s iris was treated with the Strōma Laser System. This study was completed in September 2019.
The investigators looked at all clinical outcome measures including dry eye, visual acuity, color, contrast sensitivity, retinal health, IOP, OCT images, the crystalline lens, corneal health, endothelial cell counts. No adverse events were reported, and they were able to establish the parameters needed to move forward (unpublished data).
The laser system has a high-speed tracking feature that ensures that each shot is delivered with great accuracy. There have been no reports of the laser missing the targeted area of treatment.
US trials of the laser have not yet started, but full iris trials outside the United States have shown promising safety and efficacy data. Thirty patients were assigned to three groups, 10 patients in each group (unpublished data). Researchers also administered a variety of psychometric tests to patients postoperatively, asking questions such as, “Do you think your eyes are more attractive?” No patient has reported thinking that his or her eyes are less attractive postoperatively.
I suggest starting with functional blepharoplasty and blepharoptosis repair, with supervision if you feel that you need it. As you get comfortable, you can consider doing treatments that are a little more complex. For overviews of a few aesthetic offerings you may consider adding to your practice, see the sidebars accompanying this article.
Intense Pulsed Light
By Laura M. Periman, MD

Intense pulsed light (IPL) is not a laser. It is a powerful broad beam light, well above the UV spectrum. This mode of cosmetic skin treatment has been around for more than 20 years and has a long list of FDA-approved indications, including rosacea and benign vascular lesions. Although many manufacturers outside of ophthalmology produce IPL machines, the M22 Optima IPL (Lumenis) has built-in treatment algorithms and safety features that make it easy for ophthalmologists to incorporate into their clinical practices.
When clinicians begin to look closely at dry eye disease, they will notice the high prevalence of ocular and facial rosacea in patients with dry eye. The M22 Optima IPL is my go-to treatment modality for patients with rosacea who have Fitzpatrick skin types I-IV. In my experience, IPL results in excellent improvement of a variety of dry eye disease symptoms, including clinical findings with fluorescein staining of the ocular surface, tear breakup time, meibomian gland expressibility, osmolarity readings (TearLab Osmolarity System), and inflammation (InflammaDry, Quidel). IPL has also been found effective in the treatment of acute and chronic chalazia (unpublished data)1-3 as well as in the control of Demodex.4
But the part that patients really love is that they look better, too. IPL is the only thing in our advanced dry eye toolkit that also gives patients an aesthetic benefit. This contributes to the very high patient satisfaction ratings (9.2 out of 10) with this treatment modality among our patients.
If you limit IPL to just that, however, you’ll miss out on other aesthetic uses of IPL. In my practice, for example, we also use it for treating cherry angiomas around the eyelids without surgery, for which it is incredibly effective (Figure), improving the appearance of nasal angle telangiectasis (common in rosacea), and, occasionally, permanent removal of unwanted facial hair on the upper lip or chin.

Figure. A 55-year-old patient with rosacea-associated ocular surface disease and incidental angioma (top). The angioma was effectively treated (bottom) in step 4 (aesthetic clean up) of the Periman Protocol.
How it Works
In addition to its photocoagulation, photoimmunomodulation, photosanitization, and photobiomodulation properties, IPL also has photorejuvenation properties that can be leveraged across a variety of areas in ophthalmic practice.5
In Practice
In my advanced dry eye practice, when I speak with a patient who has ocular or facial rosacea, I explain, “IPL is an effective technology for controlling this aspect of your dry eye problem.” I also share some clinical photos and explain to the patient how IPL works to normalize tear osmolarity and decrease inflammation (manuscript in process).
I like to joke with patients that IPL has a side effect that they need to know about: It will make your skin look better. We don’t lead with that in my practice because aesthetics is not our main focus. We just mention it as a happy side effect. Many patients have told us that with the complexion-improving effects of IPL, they need much less of the dry eye–exacerbating cosmetics, foundations, and powders than they did prior to treatment.
If you’re going to use IPL mainly for its dry eye benefits, it’s important to use the The M22 Optima IPL, not only for its excellent safety features and efficacious performance but also because most of the peer-reviewed literature on IPL is based on this specific platform.
Additionally, I have found that taking the time to treat the eyelids with laser-grade corneal shields in place enhances the ocular rosacea and meibomian gland dysfunction treatment results.
Ideal Patient
There are two main patient pools for IPL, and they often overlap. Most ophthalmic practices treat patients with dry eye. If a dry eye patient presents with telangiectasis of the lid margins, significant meibomian gland dysfunction, or with evidence of ocular rosacea or facial rosacea, you should begin a discussion about IPL and the dry eye benefits associated with it. On the other hand, if you want to focus on the aesthetic aspects of IPL, the ideal patient is someone who has a skin issue such as rosacea or sun damage and is self-conscious about it. It depends on what’s important to the patient.
A Workhorse
I have found IPL to be the workhorse of my advanced dry eye practice. Patients are thrilled with the improvements in their dry eyes and their appearance. We have made some instructional videos on YouTube and will be adding more content to DryEyeMaster.com. I encourage anyone interested in this technology to explore it further.
1. Paper presented at the: 37th Congress of the ESCRS; September 14-18, 2019; Paris.
2. Paper presented at the: ASCRS/ASOA 2019; May 3-7, 2019; San Diego.
3. Paper presented at: Women in Ophthalmology 2019 Summer Symposium; August 22-25, 2019; Coeur d’Alene, Idaho.
4. Fishman HA, Periman LM, Shah AA.Real-time video microscopy of in vitro Demodex death by intense pulsed light. Photobiomodul Photomed Laser Surg. doi: 10.1089/photob.2019.4737. [published online ahead of print January 27, 2020]
5. Dell SJ. Intense pulsed light for evaporative dry eye disease. Clin Ophthalmol. 2017;11:1167-1173.
Staffing the Aesthetics Side
Staffing concerns will depend upon how and where you perform aesthetics procedures in your practice.
Ambulatory surgery center. Most surgeons perform aesthetic procedures at the surgery center that they use, in which case staffing is a nonissue.
In the office. Another approach is to perform the uncomplicated aesthetics procedures in your office. I used to do this, and I would train my enthusiastic technicians how to act as my surgical assistants, essentially, during blepharoplasty.
In either scenario, you don’t necessarily have to hire new staff members and therefore add business overhead to begin offering aesthetics procedures.
Injectable Dermal Fillers
By Anaïs L. Carniciu, MD

Dermal fillers are injectable agents that treat the volume loss and associated signs of facial aging that occur with maturity. They can also be used to volumize skin irregularities such as depressed scars.
FILLER MATERIALS
Currently, dermal fillers are made from four main materials. The most commonly used material is hyaluronic acid (HA). Other available materials include calcium hydroxylapatite (CaHA), poly-L-lactic acid (PLLA), and polymethylmethacrylate (PMMA) with bovine collagen. See the Table for detailed information about each of these materials.
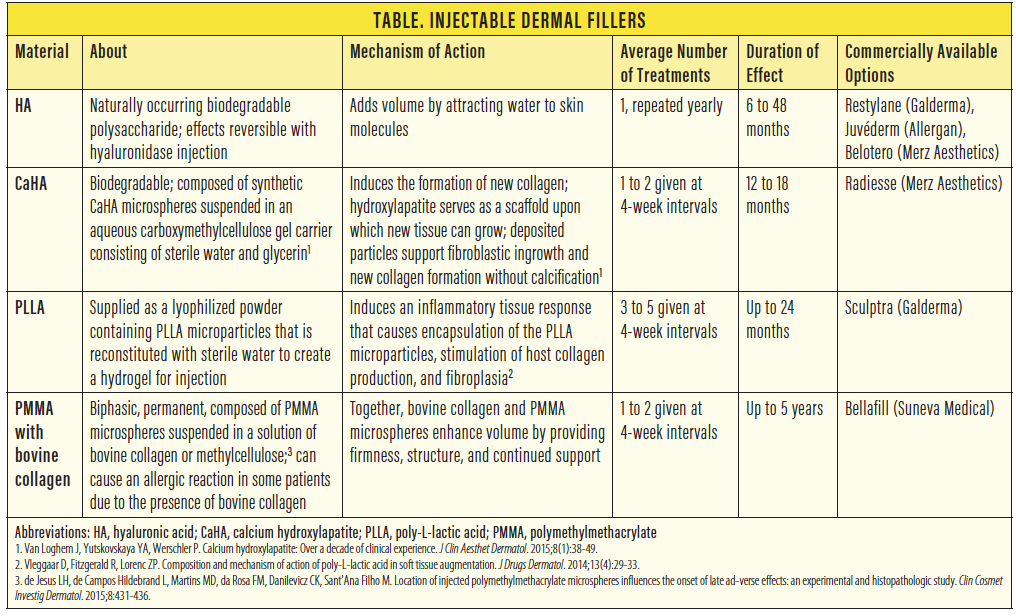
Of note, PMMA-based dermal filler carries the risk of an allergic reaction to the bovine collagen. With proper preprocedure allergy skin testing, this material may be considered only for patients seeking very long-term volume augmentation.
FILLER TRAINING
For ophthalmologists interested in additional aesthetics training after residency, it’s best to make use of resources from the AAO. The AAO offers programs at its annual meeting that can help surgeons learn the nuances of filler techniques and materials through hands-on training. Ophthalmologists with an especially strong interest in facial aesthetics can pursue additional subspecialty training in oculofacial plastic surgery as part of an American Society of Ophthalmic Plastic and Reconstructive Surgery fellowship, which is the route I took.
It’s advisable to become an expert with HA filler injections prior to incorporating any of the other materials in your clinical practice. HA is the safest of the filler materials available because it can be reversed with the injection of hyaluronidase. Without hyaluronidase injection, HA fillers dissolve on their own over 1 to 2 years.
Prior to adding filler injections to your clinical practice, I highly recommend that you have expertise with the injection of a cosmetic neurotoxin such as Botox (onabotulinumtoxinA, Allergan). Because cosmetic neurotoxin injection carries a much lower risk profile than dermal filler injection, the former is a safer clinical approach for developing injector expertise.
COMPLICATIONS AND PRECAUTIONS
A thorough, expert-level understanding of oculofacial anatomy is necessary for any aesthetic provider offering dermal fillers. Potential side effects of filler injections include under- and overtreatment, bruising, edema, allergic reactions, infection, and granuloma formation. Because injectable dermal fillers are also associated with rare but serious complications, including skin necrosis, blindness, and stroke, surgeons should always have a filler crash cart. These are materials that should always be available in the office, fully stocked and readily accessible, just as you’d have an endotracheal tube available in an intensive care unit. The crash cart should contain aspirin, nitroglycerin paste, and hyaluronidase to reverse an HA filler, if needed.
CONCLUSION
Dermal fillers are excellent nonsurgical treatments to offer your patients. Patient satisfaction is typically quite high, especially among patients with mild early facial aging changes who aren’t yet ready to go to an oculoplastic surgeon for a more invasive surgery in the OR.
Talking to Patients
I don’t do any external marketing for eyelid surgery. Most of the cases that we do in my practice are organic—what we call within the practice. I simply offer the procedure to the patient if I notice something, such as dramatic cholestasis and ptosis. I explain to the patient why that can be an issue and note that I can perform a procedure to correct it.
Aesthetics patients require a different conversation. The results for these patients are immediate or nearly immediate, and there are not a lot of complicated postoperative issues associated with aesthetic procedures. That’s not to say there are no complications, of course.
The initial examination is crucial and should include measurements such as margin-to-reflex distance and tests such as levator function. A detailed history is also necessary to determine if the patient has ever experienced visual field loss. This allows you to have a thorough diagnostic conversation with the patient.
Complex Procedures
More complex procedures can be incorporated into your practice as your comfort level grows. These can include ptosis repair in patients who have previously undergone ptosis repair surgery, lower eyelid blepharoplasty, and canthopexy.
Lower eyelid blepharoplasty and canthopexy are much more complex procedures than upper eyelid blepharoplasty in terms of anatomy and scope of surgery. If you’ve never performed these procedures, a surgeon who is experienced with them should supervise you until you are comfortable performing them.
I don’t perform any advanced oculoplastic treatments in my practice. I think it is best to refer patients who require these procedures to an oculoplastic surgeon—ideally a board-certified member of the American Society of Oculoplastic and Reconstructive Surgery—because of the level of complexity of the procedures.
Why Incorporate Aesthetics?
The biggest reason to incorporate aesthetics into your practice is the decrease in reimbursements that we have seen over time for any procedures billed through insurance. Commercial and even Medicare insurance payments are on a downward trend. A second reason is that we can help our patients to improve their appearance and feel better about themselves. If you have an interest in aesthetics, and you think your patients would enjoy the fact that you’re offering rejuvenation treatments, aesthetics can be a great addition to your surgical toolbox.




