Pearls and Practices for Virtual Eye Care
By Sophie D. Liao, MD; Eimi Rodriguez-Cruz, BS; Malik Y. Kahook, MD; and Cara E. Capitena Young, MD




It is hard to believe that, a short few months ago, we were conducting business as usual. In early March, with the number of COVID-19–positive cases climbing precipitously in Colorado and an executive order by the governor to stop routine and elective patient care, we were suddenly facing a 90% drop in our clinic and surgical volume.
The changes to CMS telehealth policy announced on March 6 were potential game-changers, but they have also resulted in a race to understand and implement those changes. In our practice, harnessing virtual health capabilities has helped us to provide care to many of our patients. Telehealth will be a tool that can be carried on far beyond COVID-19.
KNOWLEDGE SHARE
We want to share some of the teleophthalmology pearls and practices that we have implemented and found to be helpful.
Pearl No. 1: Designate a team to lead your efforts. If you run a solo practice, that team may be you or you and your practice manager. If you are in a multispecialty group or a large academic institution, as we are, it is best to task a small team to lead your virtual health efforts.
Your virtual health team should check daily for relevant changes to federal, state, institutional, and payer virtual health policies and regularly update the rest of your group. In our department, a group of four leads these efforts. Key updates are emailed and cached on a shared drive that was established to hold all documents and communications related to departmental COVID-19 information. Our team includes superusers, our medical director, and our practice administrator, and it oversees dedicated staff who serve as a resource to troubleshoot issues that arise.
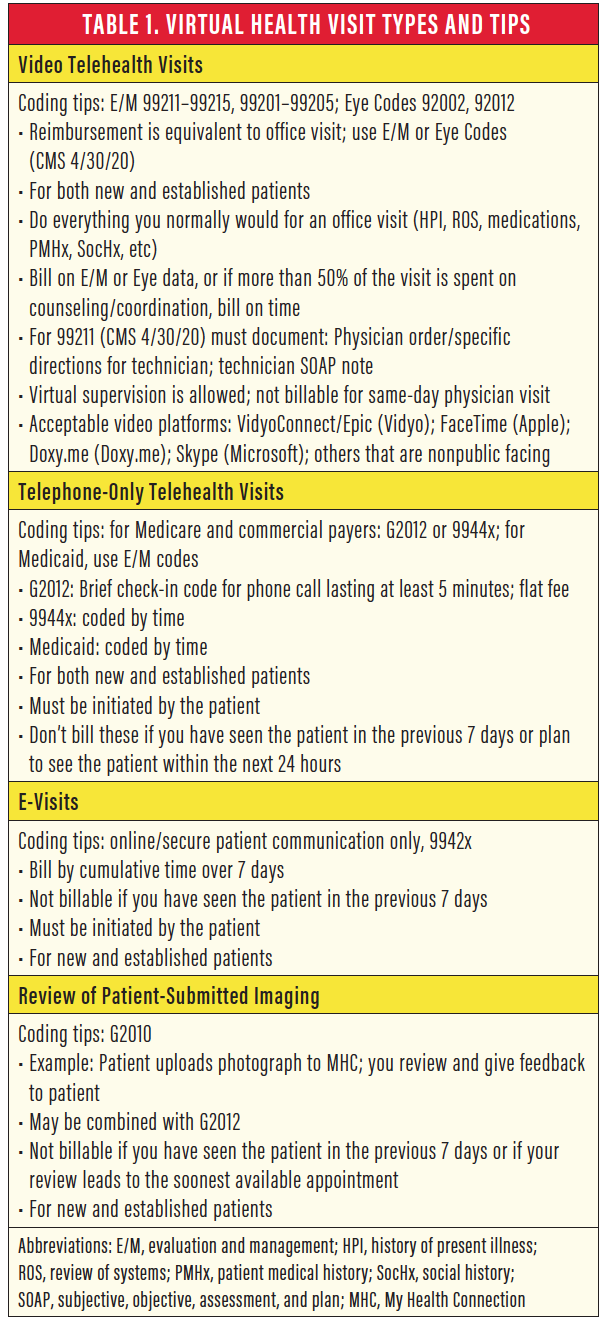
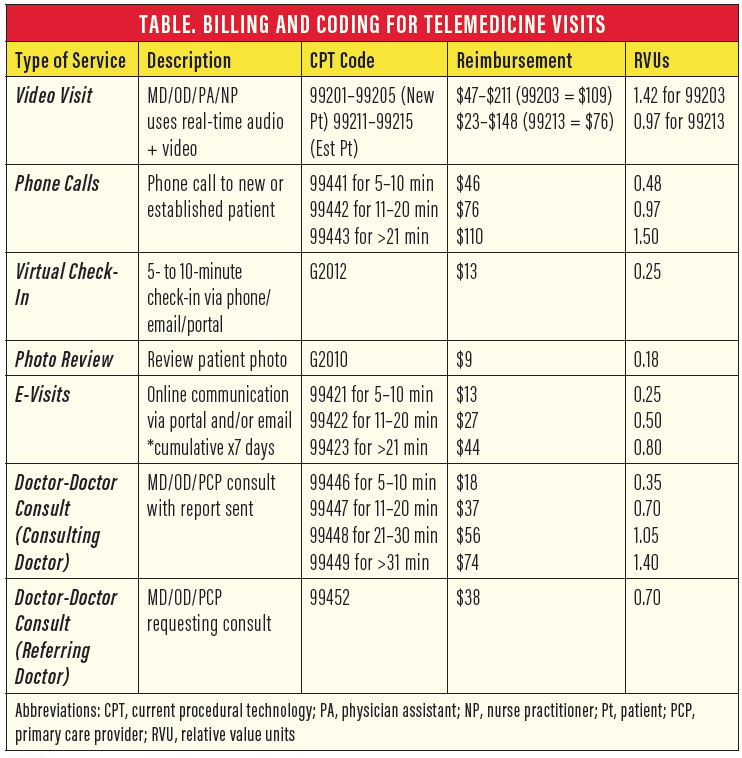
Pearl No. 2: Know which telehealth visits can be used in ophthalmology and how. E-visits may include video and telephone visits, image reviews, and online communication. Table 1 presents details about the types of visits allowed and their associated codes.
A first step is to identify which kinds of visits are appropriate for video and telephone virtual health. We tasked each division within the department to put together a list of patient diagnoses that would be appropriate for virtual health visits. The lists they generated included, for example, postoperative visits, external or adnexal evaluations, and complaints of red eyes.
You must also establish a virtual health workflow for urgent patient calls. Ours are now first triaged by a resident with attending oversight, then preferentially scheduled into a virtual health slot when appropriate.
Establish a protocol for staff members to verify that patients can participate in a virtual health visit. For example, for video visits, patients must have a private location they can be seen in during the appointment, and they must have access to a device that has a camera and microphone.
Pearl No. 3: Leverage virtual health to expand the patient population while minimizing face-to-face contact. Ways to minimize contact include sending patients a vision testing chart and instructions ahead of their virtual visit via regular mail, secured email, or communication through your electronic health record. Great printable and mobile-friendly charts are available from the AAO and at the website farsight.care.
Similarly, for evaluations of lesions, periocular problems, or red eyes and for select postoperative evaluations (eyelid surgery, Mohs repair), you can ask patients to send a close-up photograph to you ahead of time using a secure patient communication service.
Another way to minimize face-to-face contact is to institute hybrid virtual health diagnostic visits. For certain time-sensitive visits, some elements of the examination must be performed in person, whereas the remainder of the visit can be conducted virtually. Therefore, we identified low-volume satellite locations where necessary diagnostic imaging or an IOP check could be performed. The patient would then return home, and a subsequent virtual health visit would be completed with the provider.
A modified version of the hybrid visit can be used in the clinic setting. For example, all examination elements could be performed as per normal, but then the provider would step out of the examination room and complete counseling over a video system to limit the amount of time spent in close proximity to the patient.
We have also instituted drive-up IOP checks to maintain regular management of our glaucoma patients. (Editor’s note: see “Avoid a Logjam of Patients When the Economy Fully Reopens.”)
Pearl No. 4: Choose a video platform to use and one or two backups. Our university-based hospital chose the VidyoConnect (Vidyo) video conferencing system, which we use in conjunction with our Epic electronic health record system. This service allows screen sharing so that we can show the patient test or imaging results, and it provides a whiteboard for freehand illustrations to supplement our ability to communicate with patients.
Be prepared to use a backup platform because one may work better than another for your patients. Other similar systems include Doximity (Doximity), Skype (Microsoft), FaceTime (Apple), Doxy.me (Doxy.me), and Zoom (Zoom Video Communications). Keep in mind that, for all of these, your device and your patient’s device must have a camera, microphone, and speaker.
HIPAA compliance rules are currently relaxed, but that may change after the COVID-19 crisis abates. Refer to the US Department of Health and Human Services (HHS) COVID-19 website and note the most recent guidance from the HHS Office of Civil Rights regarding HIPAA and telehealth from March 20, which states:
“[Office of Civil Rights] is exercising its enforcement discretion to not impose penalties for HIPAA violations against healthcare providers in connection with their good faith provision of telehealth using communication technologies during the COVID-19 nationwide public health emergency.”
Pearl No. 5: Get help. If you have the luxury, it is worth having someone (medical assistant, technician, front desk staff member) on standby to help your visits go more smoothly by:
- Scheduling virtual health appointments;
- Calling the patient the day before their visit to prechart items such as history of present illness, reconciliation of medications, and allergy documentation; to obtain consent; and to ensure that all documentation is in place;
- Troubleshooting technology issues with the patient before and during calls;
- Rooming the patient, scribing for your visit, or providing medical interpretation; and
- Scheduling follow-up appointments.
We have also reintroduced trainee involvement in a virtual capacity to capture safe educational opportunities.
Pearl No. 6: Know your billing. Table 2 outlines our estimated CMS reimbursement matrix.
Pearl No. 7: If your patient is out of state, verify that you can see him or her.
States have different rules around this, so make sure you check each time. Our hospital’s virtual health command team took the lead on finding out what states allow us to conduct and bill for virtual visits. As of mid-April, nine states outside of Colorado allow Colorado-licensed providers to conduct virtual health visits, with varying levels of restrictions.
If you cannot legally see a patient who is out of state, you may still be able to perform a consultation with a provider located in that state (for example, an urgent-care provider seeing your patient) who can then administer care or treatment.
Pearl No. 8: Plan for post–COVID-19 life. Evaluate what virtual health is doing for your practice. Are there protocols and workflows that you have been forced to change that are now more efficient? Look at your productivity metrics prelockdown versus during this pandemic. How much of your previous volume are you capturing? What is the expected revenue? Which parts of your practice might be amenable to keeping on some version of virtual health, should reimbursement for these types of visits be retained by payers?
At our institution, we collect data daily and analyze it weekly. Give your practice a hard look now to best plan for your future.
Pearl No. 9: Know your resources. Beyond our internal hospital communications, we check these sites regularly for updates:
- AAO (www.aao.org/practice-management/telehealth);
- CMS (www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet);
- HHS (www.hhs.gov/hipaa/for-professionals/special-topics/hipaa-covid19/index.html); and
- HHS OCR (www.hhs.gov/sites/default/files/telehealth-faqs-508.pdf).
Telehealth: New Experience, New Perspective
By Cathleen M. McCabe, MD

These are extraordinary times. We are at once disconnected physically from family, friends, colleagues, and patients, but, at the same time, with the availability of video conferencing technology, we are more connected than ever. Our collective facility with the use of video chat and conferencing software has improved at a startling pace. This technology has allowed us to connect and communicate in ways that, although new to many of us, are powerful enough to cross the barriers of physical space that would otherwise effectively isolate us.
I believe that we will emerge from the current crisis—a human and global crisis—with a new perspective on community. The value of our connection to one another and the crucial role communication plays in our personal and professional lives have been vividly highlighted. And I believe this new medium of communication is here to stay.
INTEGRATING TELEHEALTH
With this in mind, and with the regulatory changes CMS has made with regard to telehealth (see CMS Changes to Telehealth), we were determined to develop a telehealth plan for our practice that would be sustainable into the future and would become an integrated part of our practice. We wanted it to work well with our practice management software, be intuitive for both doctors and patients, allow a flow that would mimic our in-office patient flow, and be technology-agnostic. Technologies based on application software are available, but we felt that a browser-based platform from vendors such as Doximity or Luma Health would be easiest for patients to navigate.
Browser-based software allows text messages or emails to be sent to patients with a simple link that can be clicked on to enter the virtual room. The platform we chose, Luma Health, also integrates in parallel with our practice management software so that, during a telehealth visit on the Luma Health site, demographic information for the patient is pulled from our practice management software.
THE VIRTUAL ROOM
The physician logs onto the Luma Health site and sees the telehealth visits scheduled for the day, alongside a link to enter the virtual examination room. Alerts can be set up to tell the physician when a visit is about to begin, when the patient arrives in the room, and how long the patient has been in the room. It is also possible to send links to enter the room to a third party, such as a technician, a scribe, a family member, or even a translator.
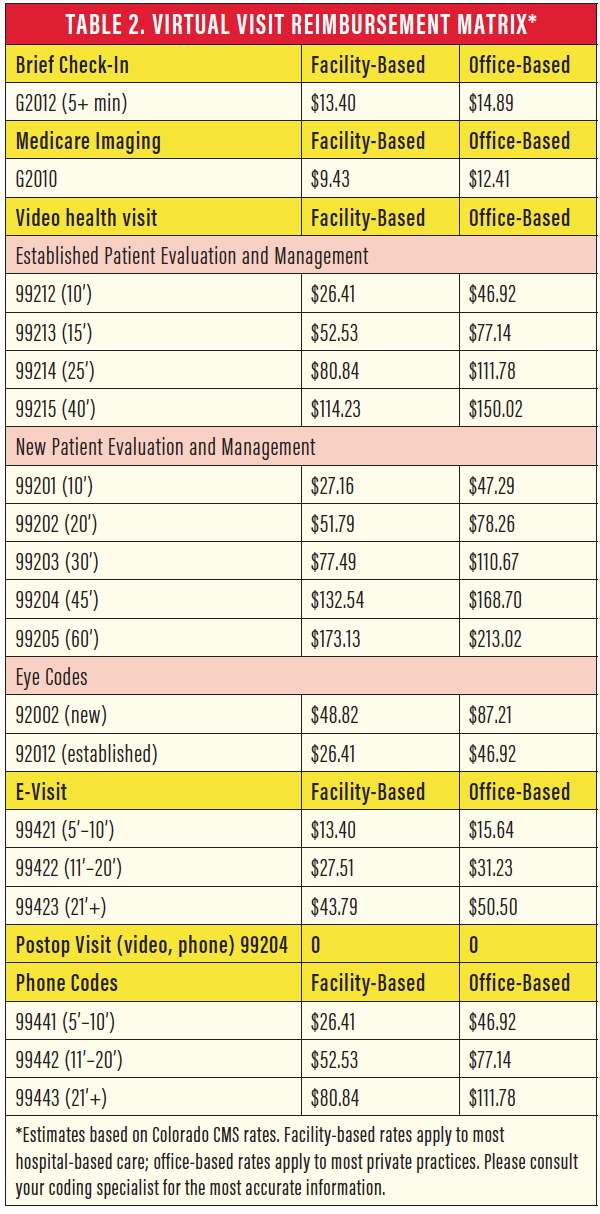
The telehealth visit can flow much like a traditional in-person examination (Figure 1). The patient receives an appointment reminder that also details additional steps to be completed prior to the examination, such as taking a web-based visual acuity or Amsler grid test, and tips for a successful examination, such as having a family member present and finding a place with good lighting for the examination.
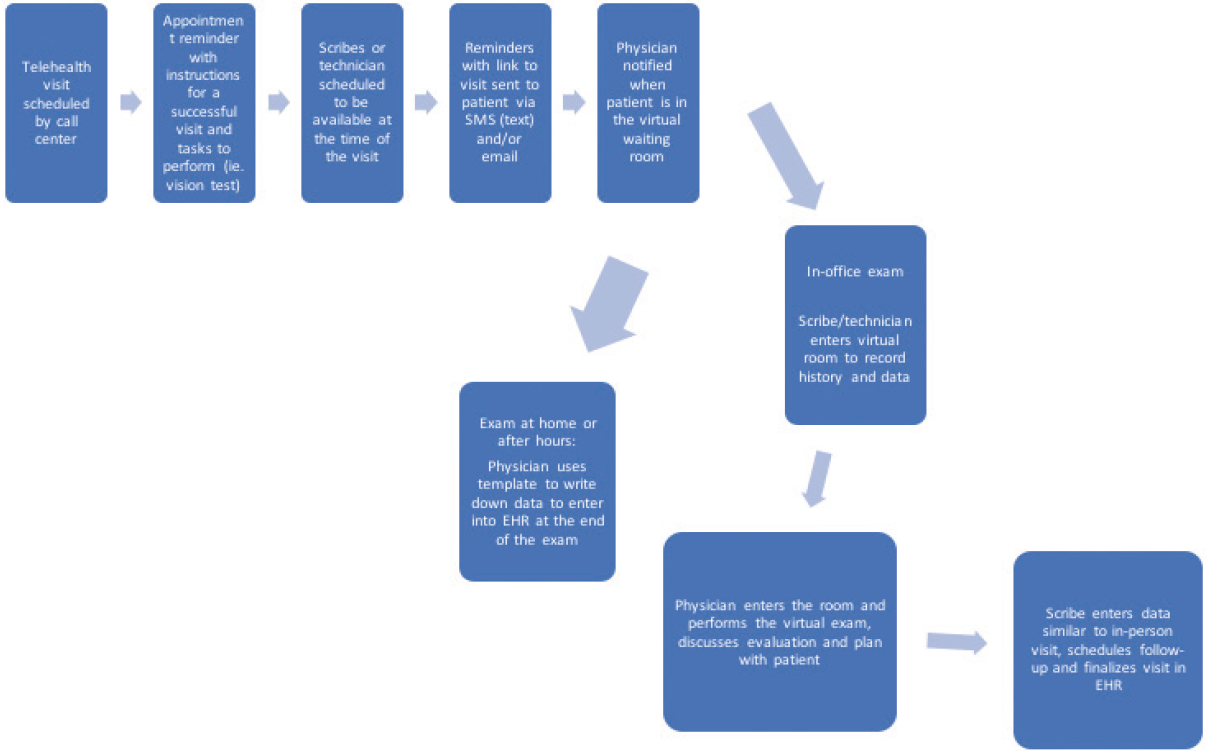
Figure 1. Flow chart for a telehealth visit.
The patient enters the virtual room and is greeted by a technician or scribe. The history, review of systems, allergies, and medications are reviewed and documented. When the patient is ready, the physician enters the virtual room (Figure 2), discusses the patient’s problem, examines the eyes externally, the relative pupil size, the extraocular motility, and the conjunctiva and external appearance of the cornea. The doctor can then decide that an in-person visit is necessary or can make a diagnosis and plan and discuss these with the patient.
Figure 2. A telehealth consultation can be performed by the physician in the office (A) or from home (B).
Telehealth visits can take place with the doctor and staff members in the office, or any of them can be in the virtual room from remote locations. To facilitate documentation, especially if the doctor is initiating a visit from home or outside of regular office hours on call, we have developed a template for written documentation that can be added to the electronic health record after the visit concludes.
ENHANCING CARE
In our practice, some doctors have converted a large portion of their schedules to telehealth visits with very positive patient acceptance. The best uses of telehealth have been in triaging emergency room visits, for conducting follow-up examinations for previous surgeries that were delayed due to the COVID-19 pandemic, and for patient follow-up for external disease conditions such as dry eye or blepharitis.
We intend to continue to use telehealth to enhance the care of our patients’ ocular health while protecting their overall safety by maximizing social distancing and minimizing unnecessary time in the office. In the future, physician-to-physician consultations, second opinions, after-hour or on-call visits, and hybrid visits in which the discussion portion of the examination is conducted through telehealth are likely areas for expansion of this technology in our practice.
Patient acceptance of telehealth visits has been exceptional overall (see Watch It Now). Patients have appreciated the chance to have their ocular health evaluated, and they value the interaction with the provider at a time when it is difficult to feel safe in an office setting.
As an example, I had a telehealth visit with a patient who developed a chalazion (Figure 3). Her rheumatologist had stopped her rheumatoid arthritis injections for fear of exacerbating the presumed eyelid infection. During the telehealth consult, I reassured the patient and gave her a course of action to help with the chalazion. She resumed her antiinflammatory therapy, and her lid was much improved the next day.
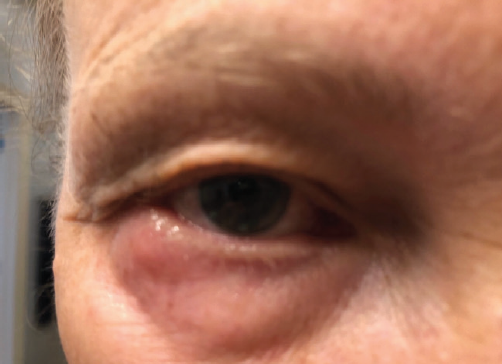
Figure 3. This patient photograph shows a right lower lid chalazion assessed during a telehealth visit.
Figures 1-3 courtesy of Cathleen M. McCabe, MD
One of Dr. McCabe’s patients provides a testimonial on the effectiveness of telemedicine.
CMS Changes to Telehealth
As of March 1:
- Site-of-service requirements have been removed to now permit patient-at-home telehealth visits.
- HIPAA requirements have been waived so that real-time video conferencing is available through FaceTime, Skype, and others, but no public-facing forums such as Facebook or Instagram are allowed.
- Established and new patient visits are both eligible for telehealth consults, and claims to determine if new or established will not be audited.
- Medicare will reimburse allowed telehealth codes the same as in-person visits.
- Flexibility in reducing or waiving copays and deductibles is now allowed.
- Prior authorizations are suspended.
- Non-Medicare payers should follow the same guidelines; many now offer $0 copays for telehealth.
- The narrow scope of diagnosis for telehealth has been dropped.
- Practice across state lines has been authorized.
Additional changes as of April 30:
- Four new eye codes have been added to telehealth consults (Table).
- Additional audio-only codes (99441–99443 codes) will be paid at the same rate as in-person codes; the new codes are based on the single telehealth visit instead of on cumulative time.
CONCLUSION
We believe that telehealth is here to stay in our practice and that it will only enhance our ability to take excellent care of our patients in the new normal going forward.
Increasing Patient Buy-In to Telehealth
By Blake K. Williamson, MD, MPH, MS

When the COVID-19 disaster struck, we decided almost immediately to implement telemedicine in our practice. We did so first and foremost because it was the right thing to do for our patients. Like most other practices, we had limited in-office visits to only patients with emergent needs, and we wanted to find a way to let our other patients know that we had not forgotten them.
Through telemedicine, we could continue performing certain examinations remotely, and we could answer patients’ questions and refill prescriptions. Another benefit, of course, was that telemedicine helped us to continue bringing in some revenue during the time that we had to close the practice except for emergent cases.
FINDING THE RIGHT FIT
We care for many elderly patients with limited proficiency in use of technology, even with their smartphones. Therefore, we knew that we needed to incorporate a telemedicine platform with the most straightforward and bare-bones approach. We chose the Doxy.me telemedicine solution and obtained free access to the premium clinic level of the software through our longstanding pharmaceutical compounding provider, ImprimisRx.
With Doxy.me, if patients can text, they can use the app. To attend an appointment, the patient receives a link to the appointment in a text message. The patient clicks on that link, which brings him or her into my virtual waiting room. When the patient has arrived, I start the call, and the two of us connect via video chat much like FaceTime and similar apps.
FRAME THE CONVERSATION TO INCREASE BUY-IN
When we initially implemented Doxy.me, we were disappointed with patients’ acceptance of this mode of practice. Looking back, the way we framed the conversation might have held us back from achieving our goal of at least 10 appointments per day per provider. One of our team members would call patients and say, “You have the option to do a telemedicine visit. Would you like to learn more?” We then changed the script to, “Dr. Williamson asked us to reach out and let you know we are here for you. He would like to check in on you and make sure you are doing OK. Are you available for a virtual eye experience at 9 am tomorrow?” With that simple tweak—using virtual eye experience to describe a telemedicine visit—we had much more success.
LOGISTICS
There are a couple of logistical tips and tricks that I find useful with Doxy.me.
No 1: Virtual waiting room. Not all patients remember they have a telemedicine visit, so I like to invite two patients at a time into the virtual waiting room. I consult with the first patient who shows up. When the second patient pops up in my virtual waiting room, I can quickly send a text message to say, “I will be with you in a few minutes.”
No. 2: Imaging. With Doxy.me, I can take photographs of the anterior segment. For a patient with pingueculitis, a conjunctival lesion, or a chalazion, I can photograph the problem and follow it over time. This can be billed separately as a G code for evaluation of a clinical photograph.
No. 3: Three-way calling. Doxy.me has a three-way calling option, which is helpful so that a scribe can be on the call. Wi-Fi is not always dependable, however, and I prefer my scribe to listen in via cellphone and enter my findings into the patient’s electronic health record as I complete the call.
No. 4: HIPAA compliant. CMS has temporarily relaxed its HIPAA guidelines for telemedicine, but Doxy.me is fully encrypted and completely HIPAA compliant. Restrictions on telemedicine may be reinstated in the future, in which case Doxy.me has us covered.
CONCLUSION
As our patients become more comfortable with virtual examinations, we hope to increase how much we use this mode of practice in our post-COVID-19 practice. Telemedicine is a great option for completing simple postoperative visits under the global period, allowing us to clear appointment slots for other billable visits. With a platform like Doxy.me, we will be able to do a quick check-in, take a crystal-clear picture, and make sure patients have no redness and are seeing well after their surgery.
Telemedicine Platforms: Live Demonstrations and More Information
DOXY.ME
Dr. Williamson demonstrates telemedicine with the Doxy.me platform.
EYECARE LIVE
Built by doctors for doctors, the Eyecare Live platform can be used to supplement patient care.

EYEXAMVIRTUAL
A joint venture between GenieMD and EyeXam, this telemedicine platform includes EyeXam’s self-guided method for measuring visual acuity with a mobile device.
LUMA HEALTH
Dr. McCabe demonstrates telemedicine with the Luma Health platform.
MODERNIZING MEDICINE
David A. Goldman, MD, demonstrates telemedicine with the Modernizing Medicine platform.
Virtual Eye Experience: The Next New Normal in Eye Care
By Giselle Ricur, MD, MBA, MS, FATA; and Roger Zaldivar, MD, MBA, MS


Over the past few months, we have witnessed one of the most paradigmatic shifts in the history of patient care, as the social distancing forced upon us by the COVID-19 pandemic has challenged the continuum of care. With many patients and physicians confined to their homes, the medical community worldwide has turned to information and communication technology (ICT) as a solution or tool that can aid in this crisis in sanitation.
TELEMEDICINE IS NOT NEW
Bashshur et al described telemedicine as “a modality of care that challenges the traditional sine qua non dependence on physical presence and contact between providers and patients for medical/healthcare delivery.”1
Telemedicine relies on the use of ICT to support medical care. The concept has been around for many decades. In 1905, Einthoven was the first to use the prefix tele in a medical context, coining the word telecardiogram.1 Since then, many medical specialties have adopted telemedicine principles to enhance patient care. In ophthalmology, the initial focus of telemedicine was on retinal image screening. Over time, teleophthalmology—also known as ocular telehealth—has expanded to other areas of eye care because it can efficiently extend patients’ access to care.2-4
Today, we are amid a new normal in eye care, one in which telemedicine is being implemented both at eye care facilities and in the homes of physicians and patients. Telemedicine offers a simple way to communicate with patients and to maintain patient support throughout the COVID-19 crisis. Telemedicine can also lower the strain on main hospitals and large medical facilities so that they can focus on their already overloaded critical patient flow rather than nonemergent patients. Surge capacity in many places has been compromised, and keeping non–COVID-19 patients out of the health care system can help to flatten the curve.5-7
This new normal is sparking a paradigm shift in patient care, and many are now understanding the potential of telemedicine. When we can take care of our patients while still practicing social or medical distancing, we should do so.
OUR EXPERIENCE
Instituto Zaldivar is an ambulatory surgery center specializing in cataract and refractive surgery. We have four locations, two in the province of Mendoza, Argentina, and two in the nation’s capital city, Buenos Aires, approximately 1,000 km away.
In the past, we relied on a telemedicine program devised in the 1990s to enhance patient outreach. We used it to facilitate patient and physician education through our websites and to offer knowledge transfer by broadcasting live surgeries via satellite to scientific meetings and expositions. In 2001 and 2002, a severe economic, political, and social crisis in Argentina led to a complete halt of the country’s activities, along with our patient flow.
At that time, we decided to leverage our experience in videoconferencing to open a virtual clinic in Buenos Aires, equipped with what was then state-of-the-art communication technology (Figure 4).8,9

Figure 4. The Instituto Zaldivar’s virtual telemedicine clinics in Buenos Aires (A) and Mendoza (B), equipped with TelePresence solutions.
Over time, our virtual clinic transformed into a regular clinic with practitioners in different specialties all supporting our cataract and refractive surgery department. Unified visual communications have evolved over the past 2 decades, and therefore we recently merged our legacy telemedicine equipment with newer ICT solutions. We now host both our original TelePresence suites (Cisco) with new telemedicine lanes equipped with Google Meet (Google) corporate videoconferencing solutions at all four of our locations. Our physicians regularly attend both in-person and virtual patient visits, depending on the day of the week. This can be done in any office, and the process is quite user-friendly (Figure 5).

Figure 5. Updates to the clinic’s telemedicine program included cloud-based videoconferencing solutions at all four locations so that physicians can perform in-person and virtual patient examinations.
Figures 4, 5, and 7 courtesy of Giselle Ricur, MD, MBA, MS, FATA
VEX IS THE NEW NORMAL
Regardless of the technology we use, telemedicine has been an integral part of our patient care model for more than 20 years. Over that time, we have redesigned our workflow and have mastered the virtual eye examination (VEX) experience. Today, it is helping us survive the COVID-19 crisis.
The VEX experience is a patient-centered model of eye care focusing on both synchronous and asynchronous examinations of the anterior and posterior segments with the support of visual communication solutions. When social distancing was mandated by the Argentinean government on March 19, we decided to leverage our VEX experience by rescheduling all previously programmed in-person appointments as teleconsultations.
We created a new virtual workflow by reconfiguring patient appointment templates in the practice management system, designing user-friendly guides, and writing COVID-19 telemedicine-specific consent forms. The guides and consent forms were emailed to patients with an invitation to meet online.
All staff members involved in our new workflow were trained virtually through webinars customized to match each individual process (eg, administrative staff, technicians, physicians), and a general communication strategy, including both internal and external communication on our website and social media channels, was implemented.
PATIENT GROUPS
We have broken our workflow down into three patient groups.
Group No. 1: Patients triaged online only. Patients in this virtual triage group are managed remotely using videoconferencing exclusively. This avoids having them undertake any travel to the institute.
Group No. 2: Patients seen after virtual triage. After a virtual triage, certain patients are required to travel to the institute for further testing. Depending on their condition, they are seen either in person or remotely by the specialist. They are assessed in real time by a specialist at a digital slit lamp or asynchronously once back at home with a teleconsultation that includes video of their slit-lamp examination and screening tests.
Group No. 3: Patients requiring mandatory in-person office visits due to the nature of their conditions. The workflow for patients in this group follows one of two pathways. In the first, the attending physician is present in the examination or surgical room; in the second, the specialist is at home or in another remote setting within one of our facilities (Figure 6).

Figure 6. Virtual COVID-19 workflow: The patient walks in for mandatory testing performed by technicians; the physician views (A, B) and speaks to the patient over VoIP solutions, whether at home (C) or within one of the facilities (D, E), in order to maintain medical distancing.
LESSONS LEARNED
In the context of the current pandemic, we have kept patients’ eye care and monitoring at a distance through use of high-definition visual communication systems. This has essentially transformed our regular consultation process into an immersive experience, regardless of geographic location.
Safety is one of the most important factors for our patients. Our VEX experience design allows us to maintain social and medical distancing while preserving the availability of our ophthalmologists to patients and at the same time maintaining connectivity and a sense of presence among all those involved. It also helps to keep nonurgent cases out of the already overloaded hospitals.
The technological innovation of telemedicine offers further advantages. It efficiently links experts to optimize diagnostic capacity, the quality of patient care, and the entire medical process. We have already noticed the cost-effectiveness of telemedicine at the operational level, and we have sustained the profitability of our business by linking all the Instituto Zaldivar offices and keeping them virtually open for business during the mandated quarantine.
TELEOPHTHALMOLOGY TRAINING PROGRAM
In response to positive reports about our experience, many colleagues have turned to us for aid and advice in their own telemedicine efforts. Therefore, we designed a training program to assist individuals—remotely of course—in implementing teleophthalmology programs of their own.
In this program, we conduct personal interviews with colleagues in order to help them to establish new virtual workflows. We also recommend ophthalmic diagnostic equipment they will need based on their existing infrastructure (Figure 7) and assess their information technology and communication platforms, software, and networks.

Figure 7. Eye care professionals can be trained virtually to use conventional slit lamps that are adapted to be digital.
We have also participated in webinars and personal online training sessions in lieu of hosting or traveling to the usual telemedicine workshops. After each, we send an online questionnaire and quiz to all participants to better understand the type of audience (eg, MDs, ODs, technicians, administrative staff) and to assess the level of their recently gained knowledge.
CONCLUSION
Implementing telemedicine has enhanced our patient outreach. Through live consultations with our patients and by examining them synchronously and asynchronously in a safe and secure manner, we have also optimized our own time and efforts in managing workload while sustaining our practice.
This new model of eye care—the VEX experience—offers a safe and efficient means of being able to stay close to your patients. In our opinion, telemedicine has the potential to become the new normal in many places, even after the pandemic has receded.
1. Bashshur R, Shannon G, Krupinski E, Grigsby J. The taxonomy of telemedicine. Telemed J E Health. 2011;17(6):484-494.
2. Rathi S, Tsui E, Mehta N, Zahid S, Schuman JS. The current state of teleophthalmology in the United States. Ophthalmology. 2017;124(12):1729-1734.
3. Sim DA, Mitry D, Alexander P, et al. The evolution of teleophthalmology beyond diabetic retinopathy screening programs in the United Kingdom. J Diabetes Sci Technol. 2016;10(2):308-317.
4. Labiris G, Panagiotopoulou E, Kozobolis VP. A systematic review of teleophthalmological studies in Europe. Int J Ophthalmol. 2018;11(2):314-325.
5. Chauhan V, Galwankar S, Arquilla B, et al. Novel coronavirus (COVID-19): leveraging telemedicine to optimize care while minimizing exposures and viral transmission. J Emerg Trauma Shock. 2020;13:20-24.
6. Baker-Schena L. COVID-19 moves telemedicine to the forefront. EyeNet. May 2020.
7. Health systems respond to COVID-19: Technical Guidance #2. Creating surge capacity for acute and intensive care recommendations for the WHO European region (6 April 2020). World Health Organization. http://www.euro.who.int/__data/assets/pdf_file/0006/437469/TG2-CreatingSurgeAcuteICUcapacity-eng.pdf. Accessed April 20, 2020.
8. Tang RA, Morales M, Ricur G, Schiffman JS. Telemedicine for eye care. J Telemed Telecare. 2005;11(8):391-396.
9. Ricur G, Zaldivar R, Batiz MG. Cataract and refractive surgery post-operative care: teleophthalmology’s challenge in Argentina. In: Yogesan K, Kumar S, Goldschmidt L, Cuadros J, eds. Teleophthalmology. Springer; 2006:213-226




