1. What actions did your hospital or center take at the beginning of the coronavirus outbreak?

Yao Ke, MD: Zhejiang University is located in the Zhejiang province, with a population of 57 million. So far, there are 1,268 confirmed cases of COVID-19 here and only one death. At the beginning of the coronavirus outbreak, we limited our outpatient services and controlled the number of patients per day to less than 100, which is 1/30 of our normal volume. Epidemiologic history, body temperature, throat swabs, and chest CT were taken on every patient, and all were required to wear a mask.
All nonemergency operations were cancelled. Patients who needed emergency surgery were screened in the clinic for coronavirus and pneumonia. Patients who tested negative for coronavirus were cleared to undergo surgery; those who tested positive were isolated. All patients who required hospitalization were assigned to a single room after the emergency operation.

Li Xiaoxin, MD: Xiamen Eye Center is a tertiary eye hospital. We perform about 500,000 outpatient and 400,000 inpatient surgeries per year. We devised separate sets of guidelines for the eye hospital, all outpatient procedures, and all inpatient procedures. These are described in detail in my answer to question 4.

Wang Yan, MD: At the beginning of the pandemic, Tianjin Eye Hospital set up a variety of protocols to protect staff and patients. These included establishing standard operating procedures according to the Chinese National Health Commission and the US Centers for Disease Control and Prevention (CDC) guidelines and educating all employees on the procedures by hosting multiple drills; adding a screening station to identify patients with fever; performing a temperature check and collecting epidemiologic information for every patient and visitor (up to one per patient) entering the hospital; setting up an isolation zone to screen patients in a well-ventilated area; avoiding or reducing close contact with patients; establishing a buffer zone and one-way movement in the hospital to reduce the risk of cross-infection between patients; reducing personnel in the hospital and advising them to limit their outdoor activities; and requiring mandatory reporting of health status by employees, including their cohabitant family members.
Emergency Cases in Eye Care
- Acute retinal necrosis
- Acute uveitis
- Retinal vein occlusion
- Retinopathy of prematurity
- Diabetic macular edema
- Central retinal artery occlusion
- Neovascular glaucoma and secondary hypertension after silicone oil filling
- Eye injuries
- Acute endophthalmitis
We have also mandated all employees to wear surgical masks and protective gowns and all doctors to wear surgical masks, gowns, and goggles. We have installed protective shields on devices such as slit lamps (Figure 1) and noncontact tonometers to reduce risk of infection transmission from droplets. We also have employed frequent disinfection of the hospital, especially in the clinics and of medical devices, and we have equipped every clinic with air purifiers.
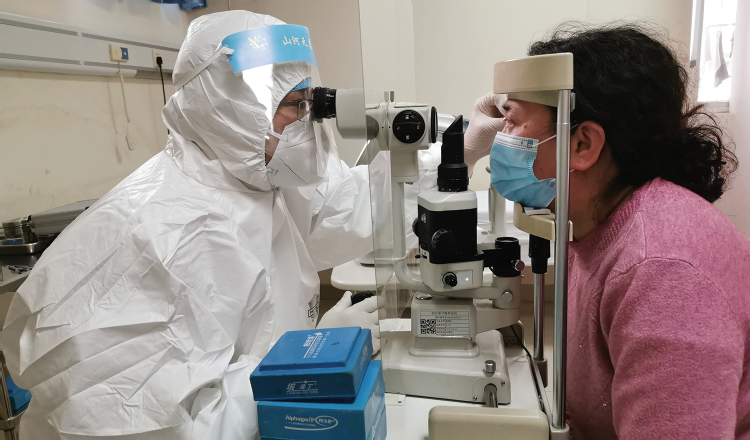
Figure 1. Slit-lamp examination, with added protection from a plexiglass shield.
At the peak of the pandemic, we temporarily shut down the chronic disease and elective surgery wards, and we provided only emergency services.
2. After China’s mandatory lockdown ended, how soon did you return to practice?
Professor Yao: Based on our prevention and control systems, our center never closed. Outpatient services and operations were restricted in February and March, and the doctors worked in opposite shifts. Young doctors worked 2 days a week, senior doctors worked 1 day a week, and doctors older than 70 years did not need to work. Starting in April, all employees returned to work, gradually resuming their workloads.
Professor Li: We never closed the clinic; however, we examined only a limited number of emergency cases, especially early in the pandemic.
Professor Wang: At the beginning of the pandemic, we closed 90% of routine clinical service and kept only our emergency service open. As the situation improved, we started to resume practice gradually according to priority, starting by treating ocular trauma, acute glaucoma, and retinal detachments. We then slowly expanded to elective surgeries, first outpatient and then inpatient procedures. We limited hospital stays for inpatient surgery. Lastly, we expanded to cataract, orbital, refractive (Figure 2), and oculoplastic surgery and to intravitreal injections. Our capacity has almost recovered to pre-COVID time. With cautious measures, 90% of our normal volume has returned. We are confident we will be back to a normal situation soon.

Figure 2. Professor Wang performs refractive surgery wearing full PPE.
3. What were the steps you took in reopening your hospital or center?
Professor Yao: In March, we gradually increased outpatient procedures to 500 per day, then to 1,000. Our typical daily outpatient volume is about 3,000. By April, Zhejiang province had adjusted to secondary response to infectious diseases, under the principles of safety prevention control, and we gradually increased the number of outpatient procedures from 1,500 to 2,000 and then up to 2,500. We also started to perform elective procedures.
Professor Li: Our first priority was protecting our hospital staff and our patients. We instituted mandatory temperature screening, and for all COVID-19 patients we opened an OR with negative pressure. Secondary measures included limiting the number of procedures we performed and spacing procedures out by at least 30 minutes to allow complete UV disinfection.
The lockdown has ended, but we continue administering screening tests for every inpatient procedure.
Professor Wang: We followed the most recent version of the Coronavirus Prevention Guidelines from China’s National Health Commission.1 According to the guidelines, appointments are required for all outpatient visits except emergency cases, and the use of telemedicine is required for patient consultations. Additionally, the guidelines mandate gradual reopening of the outpatient area of the hospital; virus testing including thoracic computerized tomography (CT) scan and C-reactive protein (CRP) for all inpatients; only one family member or companion visitor per patient for inpatient procedures; reduction of nonessential staff interactions; and extended cafeteria service hours to ensure social distancing during dining.
4. What guidelines have you implemented to protect ophthalmologists, staff, and patients?
Professor Yao: Our hospital established a leadership group for coronavirus pneumonia prevention and control under the guidance of the government. We have been adhering to strict prevention and control measures, including registering staff members’ daily health information, coronavirus nucleic acid throat swab sampling, and antibody detection. Ophthalmologists in the outpatient center are required to wear surgical masks, hats, and gloves; surgeons are required to wear medical surgical masks, hats, gloves, and disposable isolation gowns; and outpatient surgeons are required to wear hats, N95 masks, gloves, and disposable isolation gowns. A protective screen is installed on all slit lamps, and doctors perform hand hygiene routinely. It is recommended for doctors to wear protective glasses.
All surgical patients also undergo coronavirus nucleic acid throat swab sampling, antibody detection, blood tests, and CRP tests. Only one family member per patient is admitted into the hospital, and this caregiver must also undergo all coronavirus testing. Every patient who undergoes surgery must have an additional chest CT examination.
Professor Li: We established sets of guidelines for the eye hospital, the outpatient clinic, and the inpatient clinic and wards.
In the eye hospital:
No. 1: Surgery for any patients with nonemergency eye diseases is immediately rescheduled;
No. 2: All patients who require emergency eye surgery (see Emergency Cases in Eye Care.) are first tested for COVID-19. Those who test positive are assigned to a dedicated OR for further systematic assessment;
No. 3: If the patient’s condition is non–life-threatening, emergency surgery proceeds, and the OR staff wears personal protective equipment (PPE); and
No. 4: After the operation, the patient is transferred back to a special isolated care unit or hospital, and the room is disinfected.
In the outpatient clinic:
No. 1: All rooms must be properly ventilated (eg, open window or door or use of a fan if no other ventilation is possible);
No. 2: All staff must wear PPE including medical masks, hats, and protective spectacles. For individuals with glasses, a simple antifogging agent with medical alcohol and glycerin in a ratio of 1:1 can be applied to the lenses;
No. 3: A protective barrier must be applied to all slit lamps;
No. 4: For posterior segment examinations, nonmydriatic, widefield fundus, OCT, and other images are recommended instead of ophthalmoscope examination. Indirect ophthalmoscopy is recommended in place of direct ophthalmoscopy; and
No. 5: Hands must be washed or a sanitizer must be used after the ophthalmoscope exam.
In the inpatient clinics and wards:
No. 1: For each admitted patient, nurses are required to fill out an epidemiologic survey that includes questions about travel history, close contact history, and respiratory symptoms within the past 14 days. Patients who answer affirmatively to any questions are transferred to a single care unit for monitoring and screening.
No. 2: All rooms must be properly ventilated (see No. 1 in the outpatient clinic guidelines);
No. 3: All inpatients must wear masks;
No. 4: No patient can leave his or her room during the hospital stay; and
No. 5: All visitors must complete an epidemiology survey and temperature check.
Professor Wang: After reviewing national PPE guidelines and the AAO’s guidelines,1-3 we devised the following prevention and protection guidelines for ophthalmologists, optometrists, and clinics:
No. 1: Facial masks, facial shields, and goggles must be worn at all times (Figure 3);

Figure 3. Professor Wang wears a facial mask and goggles while scrubbing in for a procedure.
Images courtesy of Wang Yan, MD
No. 2: The clinic must be well ventilated;
No. 3: At least 1.5 m must be kept between staff and patients and nonessential conversation and visit times must be reduced;
No. 4: Shields must be installed on all devices, which must be disinfected after each use;
No. 5: Conversation during examination must be avoided or reduced;
No. 6: Limit one patient per consulting room;
No. 7: Indirect ophthalmoscope or fundus camera for fundus examination must be used instead of direct ophthalmoscope;
No. 8: OCT can be used for angle examinations;
No. 9: If gonioscopy or ultrasound biomicroscopy is required, thorough disinfection after each use is mandatory to reduce cross-infection or contamination;
No. 10: For intravenous injections, detented needles (preferably with safety guard) must be used to reduce repeated puncture;
No. 11: For examinations or procedures that might produce virus-containing aerosols, OR staff members should wear N95 masks;
No. 12: For general anesthesia, during intubation or removal of intubation, only personnel wearing N95 masks are allowed in the OR;
No. 13: Strict hand hygiene must be practiced;
No. 14: Touching noncontamination areas is not allowed with gloves on; and
No. 15: All health care personnel should monitor temperature daily; when an individual shows suspicious symptoms, he or she should suspend working and report to the infection control department (home isolation or seeking medical care is advised).
5. What additional tips do you have for keeping a hospital running and ensuring safety?
Professor Yao: Zhejiang University has had no nosocomial infection and no missed diagnosis of coronavirus pneumonia cases. Based on our successful prevention and control experience, the hospital has released a guide book: COVID-19 Outbreak Hospital Response Strategy.
Professor Li: I urge other hospitals to take epidemiologic records for every patient and visitor who enters the hospital or clinic. This will help to recognize those who have symptoms of coronavirus.
Professor Wang: Patients should be screened and triaged at reception, and patient visits should be scheduled to avoid crowding. Setting up a buffer zone and enforcing social distancing in the waiting area are also crucial. Ensure that all surgical patients (inpatient and outpatient) and their accompanying family members receive virus nucleic acid testing. If needed, thoracic CT and CRP should be performed to screen every potential patient or asymptomatic carrier.
6. What is your surgical volume now, and how does it compare to before the pandemic? What types of surgery, in your experience, are rebounding or recovering the quickest? What is taking the longest to rebound or recover?
Professor Yao: In April, the number of outpatient and inpatient services at our center recovered to 80% and 90%, respectively. Our workload in May was about 95% of our workload in May 2019. I think our graded reopening measures have been reasonable. Under the guarantee of safety, we have effectively resumed work. Professor Li: The Table above shows our current volume compared with our volume in 2019. We are down significantly in retina, glaucoma, cataract, and strabismus surgeries. Professor Wang: Elective surgery, such as refractive surgery, was suspended during the pandemic. We have gradually recovered these surgeries with meticulous precautions to protect patients and staff, and our surgical volume has recovered slowly, from 20% to now almost full volume from pre-COVID times. Nationwide, refractive surgery volume has been significantly affected by the pandemic. There was a 90% drop in volume in February compared with February 2019 and a 60% drop in March versus March 2019. Our peak month is typically June; however, the government’s postponement of college entrance exams will likely affect that. More hospitals and clinics are using online platforms to conduct patient education, which will help us recover to a new normal. By Tu Haixia, MD; and Wang Yong, MD Wuhan Aier Ophthalmic Hospital is a specialized ophthalmic hospital. Throughout the pandemic, the hospital has maintained outpatient and emergency operations. Early isolation management measures issued by the municipal government in Wuhan, China, helped to control the spread of COVID-19; however, they also affected the medical care of our area residents. Some patients could not travel to the hospital due to transportation closures, and others were afraid to leave their houses. In patients with acute angle-closure glaucoma who are not treated in a timely manner, irreversible visual impairment can result. Figure. Full PPE, including a face mask and shield, is worn during surgery. From January 23 to April 8, the early isolation period, 27 patients were hospitalized in our facility for acute angle-closure glaucoma. In addition to eye pain and poor vision, these patients experienced severe symptoms with varying degrees of headache, nausea, and high IOPs (range, 35–60 mm Hg; average, 43 mm Hg). The time between onset and treatment ranged from 2 to 60 days (average, 25 days). In comparison, previous time between onset and medical treatment was fewer than 7 days. All patients were treated with paracentesis to reduce IOP, and 80% also underwent a combined phacoemulsification and goniosynechialysis to open the angle. In the latter group, 80% experienced a decrease in IOP to 21 mm Hg or less, and 20% needed further medication to control IOP. Because of irreversible mydriasis or optic nerve injury, only 45% of patients had 20/40 or better BCVA postoperatively. As we all know, it is important to educate patients to seek medical care before it’s too late, even during a lockdown. 7. How is the pandemic shaping the future of patient care? Professor Yao: Until we have a vaccine, strict prevention and control measures will continue to be required. All doctors, staff, and patients must understand and adapt to the new intensity of our prevention and control measures. In order to avoid medical conflicts, a full explanation must be given to all patients. Professor Li: Self protection in the form of all PPE—medical masks, hats, and protective spectacles—will become commonplace in medicine now. We all must do much more than ever before to keep our staff safe and to keep our patients safe. Professor Wang: This pandemic has reinvigorated people’s attention to public health, their own health needs, and health care services. When patients choose a health care provider, there may now be more focus on the facility and function, with higher demands placed on quality, safety, and professionalism. This will be the same for refractive surgery patients. I think the pandemic could bring refractive surgery service to a higher level, and I am quite optimistic for the future of those and other elective operations that can better improve patients’ quality of life. 1. Diagnosis and treatment protocol for novel coronavirus pneumonia (Trial Version 7). National Health Commission and State Administration of Traditional Chinese Medicine. March 3, 2020. https://www.elotus.org/promo-files/COVID-19_resources/Guidance%20for%20Corona%20Virus%20Disease%202019%20(English%207th%20Edition%20Draft).pdf. Accessed May 15, 2020. 2. Important coronavirus updates for ophthalmologists. American Academy of Ophthalmology. May 11, 2020. https://www.aao.org/headline/alert-important-coronavirus-context. Accessed May 15, 2020. 3. Li JPO, Shantha J, Wong TY, et al. Preparedness among ophthalmologists: during and beyond the COVID-19 pandemic. Ophthalmology. 2020;127(5):569-572.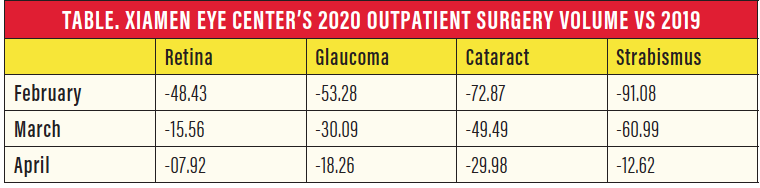
Glaucoma and COVID-19
Delays in patient care can cause irreversible visual impairment.







