
With the ever-growing array of presbyopia-correcting IOLs in the market and the endless variation in personal defocus curves and vision behavior among our cataract and refractive lens exchange patients, it is a daunting task to select the best IOL to meet the particular needs of a given patient. Historically, this has been achieved with good history-taking and the use of patient questionnaires.
The truth is, however, that most of us struggle to determine the exact needs of our patients. We don’t fully understand their visual requirements, and reading and intermediate viewing distances vary from patient to patient. Individuals spend different amounts of time doing different visual tasks, and we do so in changing environments with respect to ambient light, the presence of UV light, and the ergonomic positions that we work in. Vivior, makers of the Vivior Monitor, a visual behavior monitor (VBM) that patients can wear on their spectacles to track their visual behavior and environment, now provides a Lifestyle Match Index (LMI) to help us convert that data into useful clinical information.
The Vivior VBM is currently available in multiple European countries and is undergoing a clinical trial in the United States (it is currently interrupted by the COVID-19 outbreak). Vivior is exploring multiple opportunities within the United States to bring the device and its LMI technology to US ophthalmologists; a market introduction is expected in 2021. The LMI can include all IOLs available in a specific country, but the software is set up so that it includes only the IOLs that the respective clinic or surgeon is using.
RANKING CHOICES
The LMI performs a search, not unlike a Google search with ranking, of the available IOLs in the market with published defocus curves and then, in an objective manner, matches the IOL defocus curves to the individual patient’s personal needs. In my experience, the LMI addresses the patient’s personal visual needs better than I have been previously able to do.
The LMI display provides an overview of the patient’s personal defocus curve as well as a matrix that allows one to quickly gain an idea of the patient’s visual lifestyle. Figure 1 shows an example of a defocus curve (left) and a matrix charting viewing distance against ambient light (right). The defocus curve shows that the bulk of this patient’s visual tasks are performed at viewing distances between 0.4 and 1 m. The matrix illustrates that 44% of the patient’s tasks are at near, 43% at intermediate, and 13% at distance. The horizontal rows show that 61% of the patient’s vision takes place in good lighting conditions, 17% in mesopic conditions, and 22% in scotopic conditions.
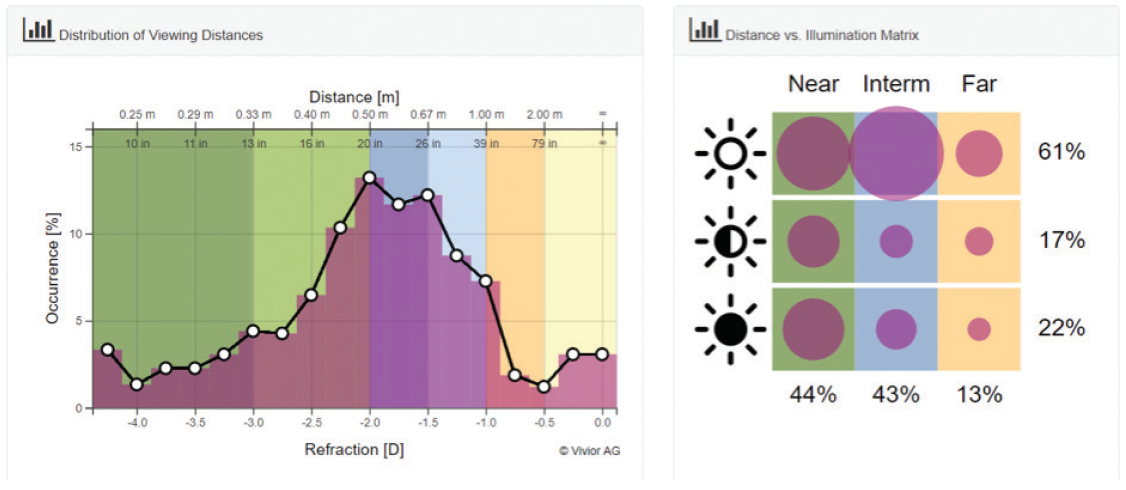
Figure 1. An example of a defocus curve (left) and a matrix charting distance against ambient light (right) generated by the LMI. The bulk of this patient’s visual tasks are performed at viewing distances between 0.4 and 1 m.
Figure 2 shows that, if this patient received a monofocal IOL targeting emmetropia, he or she would be free of spectacles for 8% of the day (note the lightly shaded area under the curve and the color bar to the right of the graph) and require spectacles for intermediate and near tasks for 92% of the day. If the ranking feature is used to select the IOL (Figure 3), one can see that a trifocal IOL would be the best fit for this patient because it can add 73% functionality over what the monofocal IOL could provide to this patient. Note that the lighter-shaded area of the graph is now much larger. Were an extended depth of focus (EDOF) IOL to be selected (Figure 4), it would provide this patient less additional coverage than the trifocal (45% vs 73%) but still significantly more than the monofocal IOL (8%).
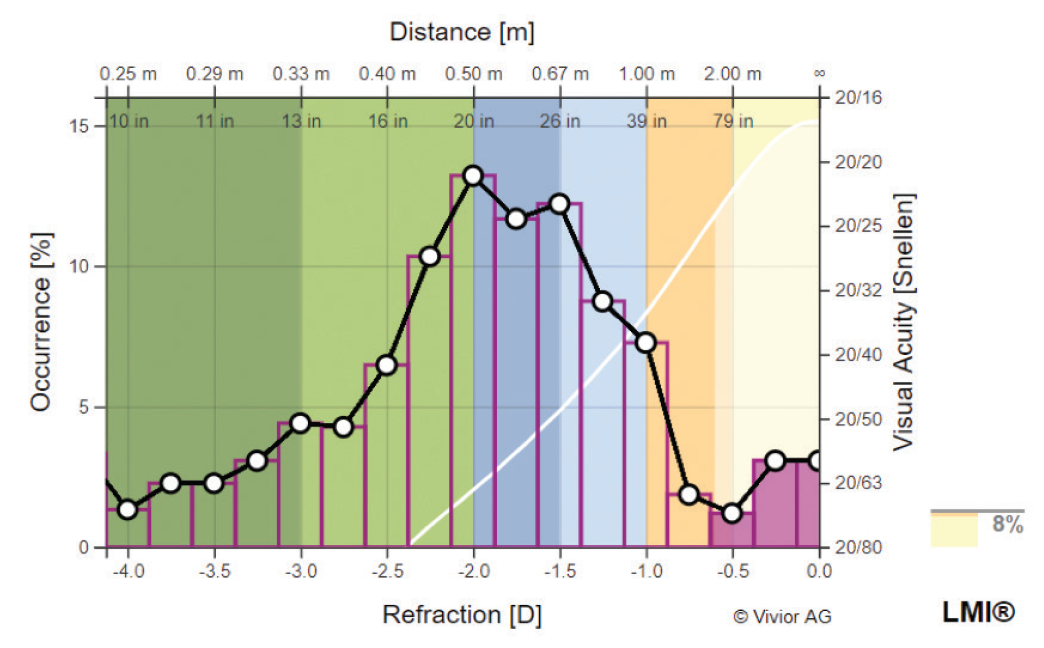
Figure 2. If a monofocal IOL targeting emmetropia is chosen for this patient, he or she would be free of spectacles for 8% of the day and require spectacles for intermediate and near tasks for 92% of the day.
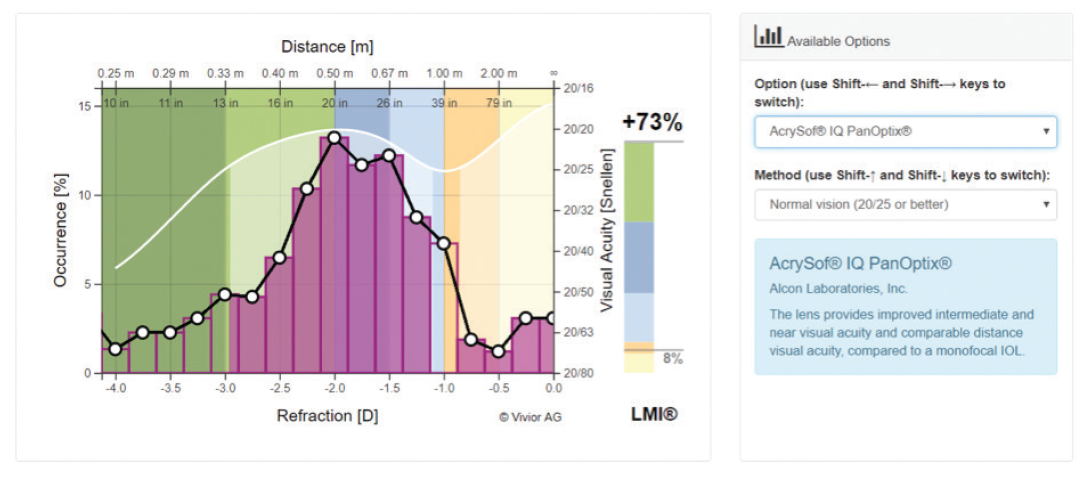
Figure 3. A trifocal IOL would be best fit for this patient because it adds 73% functionality over the monofocal IOL.
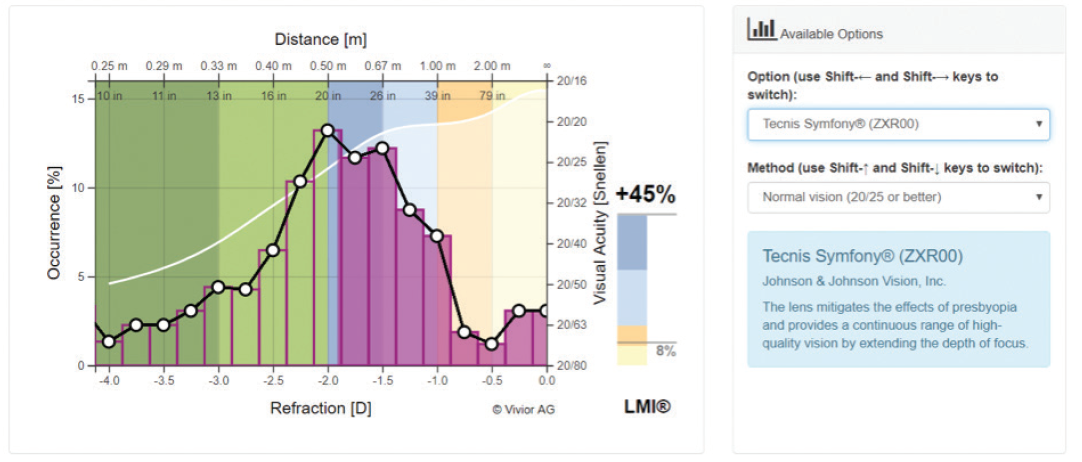
Figure 4. In this same patient, an EDOF IOL would provide less additional coverage than the trifocal (45% vs 73%) but still significantly more than the monofocal IOL.
Traditionally, we have used multifocal or bifocal IOLs for patients desiring spectacle independence, but until recently, in many cases, patient satisfaction was lacking. The LMI output shown in Figure 5 illustrates why: When a multifocal IOL with a +3.00 D add is chosen for this patient, the lens choice adds 37% to the monofocal defocus curve, compared with 73% with a trifocal. With a +2.50 D add multifocal IOL, the value-add over the basic monofocal IOL is even lower for this individual, at only 2% (Figure 6). If this presbyopia-correcting IOL were chosen for this patient, he or she would be disappointed with the near vision. We now know from the data that the expected benefits won’t be accrued.
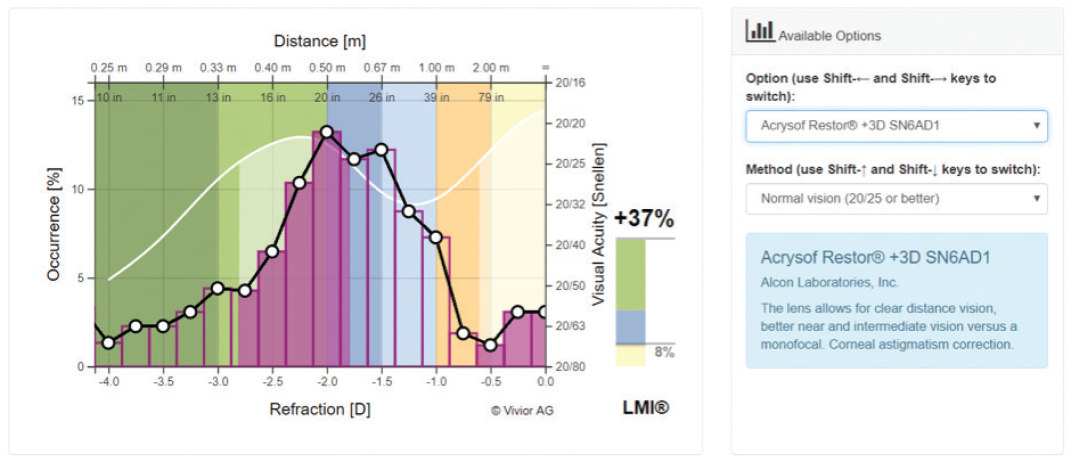
Figure 5. For a multifocal IOL with a +3.00 D add, the value-added number is 37% for this same patient.
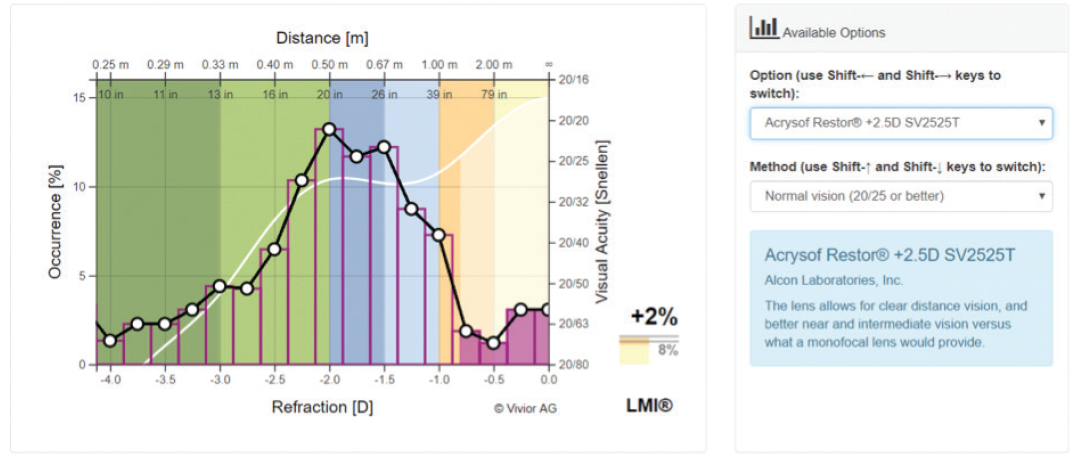
Figure 6. For a multifocal IOL with a +2.50 D add, the value-added number is only 2% for this same patient.
analyzing data sets
Vivior has now analyzed approximately 500 data sets from the Vivior Monitor. Almost 75% of the time, the best-fit presbyopia-correcting IOL is a trifocal IOL, followed by an EDOF IOL around 20% of the time and an older-generation multifocal or bifocal in about 5% of cases.
The older patients whom we normally see for cataract surgery tend to do a lot of reading, needlework, and other near tasks, so good uncorrected near vision is an important goal for their surgery.
I have been delighted with the LMI function of the Vivior technology, and patients love it, too. It certainly makes them aware of how much of their workday is spent at near and intermediate distances, and they love the fact that it is their data being matched objectively to the IOL selection.




