Although the technology for the calculation of IOL power has improved over the past several years, incorrect IOL power is still a significant reason for IOL explantation or exchange. Refractive surprises are also seen commonly in patients who have had previous corneal refractive surgery, such as LASIK or radial keratotomy. The ability to change the power of an IOL in a noninvasive manner anytime during the postoperative period is an unmet need that, if successfully developed, would likely be a mainstream technology shaping the future of ophthalmology.
In our laboratory at the John A. Moran Eye Center of the University of Utah, we have had the opportunity to collaborate with Perfect Lens in the evaluation of a technology it has developed that uses a femtosecond laser system for IOL power adjustment. The system is based on the concept of refractive index shaping (RIS), which has also been applied to the cornea (see LIRIC).1-3
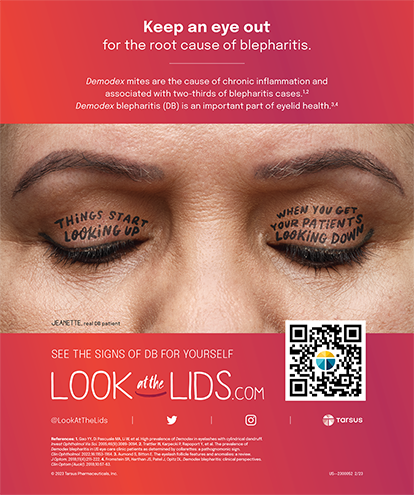
The laser emits green light at 520 nm and operates with energy levels that are below the threshold for ablation or incision. Application of the laser induces chemical reactions within targeted areas in the substance of the IOL optic, under the surface of the optic. There is an increase in hydrophilicity and a decrease in refractive index in the treated area, as the laser builds a RIS lens within it (Figure 1).
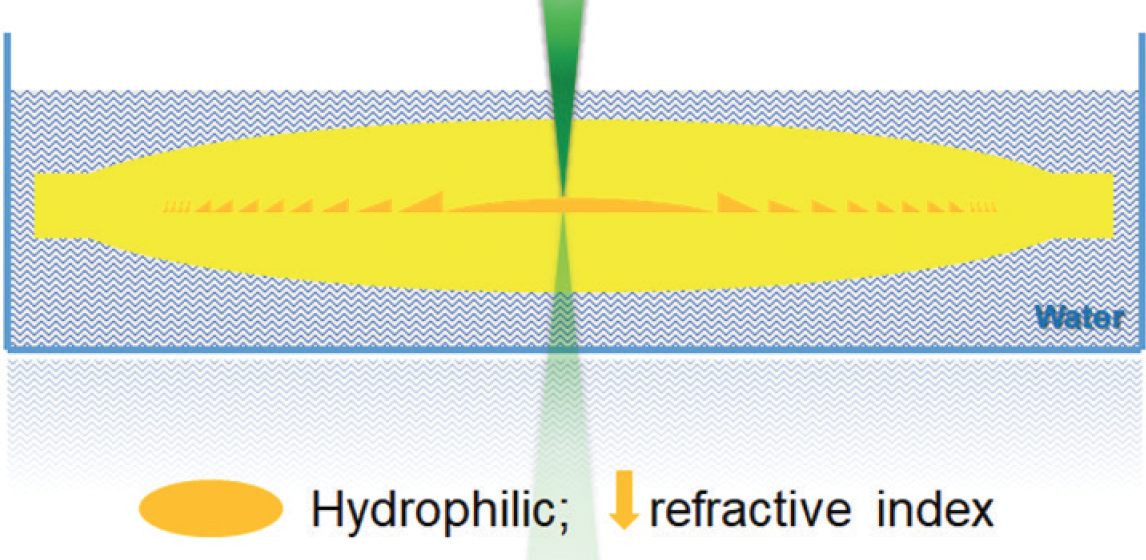
Figure 1. Schematic drawing shows femtosecond laser treatment within the IOL substance for power adjustment.
One of the most interesting aspects of this technology is that it can be applied to any commercially available hydrophobic or hydrophilic acrylic IOL; a special IOL material is not necessary.
MAKING THE ADJUSTMENT
IOL power adjustment can be obtained in a noninvasive and rapid manner. The eye is prepared with pupillary dilation and application of topical anesthesia. Alignment of the eye and docking to the laser system through a patient interface are then performed under the control of the laser device’s incorporated video and OCT systems.
The appropriate laser treatment is then applied. For a change of 3.60 D, for example, the treatment duration is approximately 23 seconds. Each treatment changes only a very thin layer within the optic substance, allowing the performance of multiple adjustments, which are also potentially reversible.
In vitro and ex vivo studies at other centers have demonstrated the accuracy and repeatability of this process and have shown that the optical quality of the lens is not significantly affected by multiple treatments.4,5 The femtosecond laser technology can be used to create multifocality in a monofocal lens, and it can also cancel a diffractive multifocal add on a traditional multifocal IOL.6,7 Creation of a toric change of up to 7.60 D in a monofocal hydrophobic acrylic lens has been demonstrated.8
RABBIT STUDY
We performed the first in vivo study evaluating the Perfect Lens technology at our laboratory.9 Six New Zealand rabbits underwent phacoemulsification with bilateral implantation of commercially available hydrophobic acrylic IOLs. Postoperative power adjustment was performed 2 weeks after implantation in one eye of each rabbit. The animals were observed clinically for an additional 2 weeks and then humanely euthanized. Their eyes were enucleated and bisected. The anterior segment was evaluated posteriorly through the Miyake-Apple view to assess capsular bag opacification.
LIRIC
Laser-induced refractive index change (LIRIC; Clerio Vision), a minimally invasive method being developed to correct the eye’s aberrations, has the potential to be used as a treatment for myopia, hyperopia, astigmatism, and higher-order aberrations.
Performed at a wavelength of 405 nm, LIRIC uses a 2-photon absorption process that alters collagen fibril density and, therefore, the refractive index of the cornea in a highly localized fashion. For a full interview with Scott M. MacRae, MD, on LIRIC, see http://bit.ly/Werner0619.
After IOL explantation for power measurements (Figure 2), the anterior segments of the rabbit eyes underwent complete histopathologic examination. Slit-lamp examinations performed after the laser treatments showed the formation of small gas bubbles behind the lenses; these disappeared within a few hours. The laser power adjustment procedure did not induce any damage to the optics of the lenses.
Figure 2. Light photomicrograph of an IOL explanted from a rabbit eye after in vivo power adjustment by a femtosecond laser. The laser-treated areas can be seen in the darker yellow color.
No postoperative inflammation or toxicity was observed in the treated eyes, and postoperative outcomes and histopathologic examination results were similar to those in untreated eyes. The power measurements showed that the change in power obtained was consistent and within ±0.10 D of the target.
BENCH TESTING
In an in vitro study also performed in our laboratory, we evaluated the IOL power, modulation transfer function, light transmission, and light-scattering characteristics of a commercially available blue-light–filtering IOL before and after power adjustment.10 A mean power change of -2.037 D was associated with a modulation transfer function change of -0.064 and a light transmittance change of -1.4% after laser treatment.
Backscattering measured with Scheimpflug photography increased within the lens optic in the zone corresponding to the laser treatment; however, the levels are not expected to be clinically significant. The treated areas within the optic could be appreciated under light microscopy without any damage to the IOL.
This study also demonstrated that power adjustment by femtosecond laser produced a highly accurate change in dioptric power without significantly affecting the quality of the IOL.
POTENTIAL ADVANTAGES
The femtosecond laser technology developed by Perfect Lens has potential advantages over existing technologies.
The FDA-approved Light Adjustable Lens and Light Delivery Device (both by RxSight) require use of a specific three-piece silicone lens manufactured with a special material that contains unpolymerized macromers within the optic substance.11 Once the appropriate power adjustment is obtained, the power of this lens has to be locked in by irradiating the entire lens, which generally takes two sessions. After that, the power of the lens can no longer be changed. Also, the patient must wear special UV-protective eyeglasses until the lock-in of the lens power is done because exposure to sunlight can cause uncontrolled polymerization of the macromers within the lens material.
Clinical studies are underway for adjustable IOLs that use a modular approach. These types of systems generally have a base component and an optic component, and power change must be done in an invasive manner, exchanging only the optic component during a secondary surgical procedure.12
CONCLUSION
Preclinical studies of the Perfect Lens femtosecond laser technology have generated interest in the ophthalmology community, and we look forward to learning more about it through clinical studies, which are set to start soon.
1. Sahler R, Bille JF, Enright S, Chhoeung S, Chan K. Creation of a refractive lens within an existing intraocular lens using a femtosecond laser. J Cataract Refract Surg. 2016;42(8):1207-1215.
2. Bille JF, Engelhardt J, Volpp HR, et al. Chemical basis for alteration of an intraocular lens using a femtosecond laser. Biomed Opt Express. 2017;8(3):1390-1404.
3. Xu L, Knox WH, DeMagistris M, Wang N, Huxlin KR. Noninvasive intratissue refractive index shaping (IRIS) of the cornea with blue femtosecond laser light. Invest Ophthalmol Vis Sci. 2011;52(11):8148-8155.
4. Koch D, Sahler R, Bille J, MacDonald S. Accuracy of IOL spherical power modification using RIS technology. Paper presented at: ASCRS Symposium; May 9, 2017; Los Angeles.
5. Youssefzadeh B, Sahler R, Bille J, Schanzlin DJ. Refractive lens diopter adjustment in rabbit cadaver eye. Paper presented at: ASCRS Symposium; May 9, 2017; Los Angeles.
6. Macdonald S, Sahler R, Bille J. Creation of multifocality in a monofocal IOL that has been implanted in a cadaver rabbit eye. Paper presented at: ASCRS Symposium; May 9, 2017; Los Angeles.
7. Olson RJ. New approach to treat postoperative multifocal IOL complications. Paper presented at: ASCRS Symposium; May 9, 2017; Los Angeles.
8. Sahler R, Enright S, Chan K, Bille J, Chhoeung S. Large-diopter toric change inside a hydrophobic IOL using refractive index shaping. Paper presented at: ASCRS Symposium; April 13-17, 2018; Washington, DC.
9. Werner L, Ludlow J, Nguyen J, et al. Biocompatibility of intraocular lens power adjustment using a femtosecond laser in a rabbit model. J Cataract Refract Surg. 2017;43(8):1100-1106.
10. Nguyen J, Werner L, Ludlow J, et al. IOL power adjustment by a femtosecond laser: in vitro evaluation of power change, MTF, light transmission, and light scattering in a blue-light filtering lens. J Cataract Refract Surg. 2018;44(2):226-230.
11. Werner L, Chang W, Haymore J, et al. Retinal safety of the irradiation delivered to light-adjustable intraocular lenses evaluated in a rabbit model. J Cataract Refract Surg. 2010;36(8):1392-1397.
12. MacLean KD, Werner L, Kramer GD, et al. Evaluation of stability and capsular bag opacification of a new foldable adjustable intraocular lens. Clin Exp Ophthalmol. 2015;43(7):648-654.