Small-incision lenticule extraction (SMILE), approved by the FDA in 2016, is the latest addition to mainstream corneal refractive surgery. Tissue depth per diopter of correction with SMILE is roughly equivalent to that with PRK and LASIK. Unlike in LASIK and PRK, however, in SMILE a femtosecond laser (VisuMax, Carl Zeiss Meditec) is used to dissect a lens-shaped portion of stromal tissue for refractive correction, followed by manual removal of that lenticule (See Watch It Now).
Watch it Now
In October 2018, the FDA approved two significant expansions to the indications for SMILE. One was the addition of astigmatic correction so that the approved range of correction now includes spherical myopia from 1.00 to 10.00 D and cylinder from 0.75 to 3.00 D. The other change now allows surgeons to make a smaller entrance incision, potentially reducing disruption of corneal nerves and the corneal surface.
This expansion, which we are calling SMILE 2.0, will allow us to treat more patients—now including those with up to 3.00 D of astigmatism—and to have more flexibility in the parameters we use. In this article, we discuss the clinical trial results that led to the recent approval and describe how we incorporate SMILE into our two separate laser refractive surgery practices.
CLINICAL TRIAL RESULTS
In the initial clinical trials for approval of SMILE for spherical myopia, 99.7% of eyes achieved 20/40 or better UCVA at 6 months postoperative, and 87.5% had 20/20 or better UCVA.1 Similarly, in data supporting the recent premarket approval, which included both spherical and astigmatic corrections (NCT02430428), 98.6% of eyes achieved a UCVA of 20/40 or better, and 84.2% had 20/20 or better UCVA at 6 months.2
These 6-month UCVA results fit nicely among the data for most of the recent LASIK FDA approvals. This is impressive considering that LASIK has had more time to become a mature technology and that it was not this accurate from the start.
Although patients can have 20/20 or 20/25 UCVA 1 day after SMILE, our clinical experience and the SMILE data from these approvals indicate that some patients’ visual recovery can take longer. The trial data showed that it can take from 3 to 6 months for patients’ vision to stabilize and establish a new baseline UCVA. In the spherical SMILE study, for example, only 63.3% of eyes achieved 20/20 UCVA at 1 week, improving to 87.5% at 6 months.1
FINE-TUNING THE SETTINGS
In our clinical experience with SMILE outside of the FDA trials, the ease of lenticule dissection is directly related to the speed of the patient’s visual recovery. Typically, the less force needed, the faster the recovery. This is where the second element of the recent FDA labeling expansion becomes relevant.
The initial approval mandated femtosecond laser spot and track spacing of 3 µm, a transition zone of 0 µm, and a 90º incision angle. With the recent change, spot spacing, track spacing, and laser energy level are adjustable, and the surgeon has the ability to expand the transition zone of the lenticule dissection. Additionally, the incision angle may now be as small as 60º, representing a potential one-third reduction in the cutting of superficial nerves.
A common observation is that not all femtosecond lasers are the same. Mirrors become worn over time, or environmental factors can alter effectiveness. The result is a lack of plug-and-play setting optimization. Each laser must be separately optimized. Most US SMILE surgeons are now in the process of optimizing their settings, which holds promise for achieving smoother dissections and allowing faster visual recovery in the future.
As they optimize their settings, many surgeons are finding success using spot and track spacing in the range of 4.2 to 4.5 µm and energy levels of 125 to 150 nJ. Most are now also using the smaller, 2-clock-hour incision angle.
If SMILE surgeons are now able to achieve significant improvements in healing speed as the lasers are optimized, it would not be the first time the refractive market has noted such improvements. Early ophthalmic femtosecond lasers used for LASIK flap creation struggled to compete with microkeratomes regarding corneal clarity. Today, however, femtosecond lasers provide excellent visual results with a level of safety that no microkeratome could ever match. We now can inspect flap quality before the tissue bridges are released upon lifting the flap.
STARTING TO SMILE
Proper training for SMILE is imperative. Poor technique and planning can greatly affect visual results. Some tips for getting started are included in the above sidebar.
We are often asked how we position SMILE in our practices. We each practice in comprehensive vision correction centers that offer all forms of laser vision correction as well as phakic IOLs, corneal inlays, refractive lens exchange, cataract surgery, and CXL.
Most patients have at least heard of LASIK, which essentially now serves as a proprietary eponym for all forms of surgical vision correction, even lens-based. It is up to us to provide the singular and best recommendation for each patient who walks through our doors. Having SMILE as an option increases our ability to do so.
When we ask patients why they haven’t had vision correction already, the answer is almost invariably one of two things: fear or money. For the latter, there are financing options. For the former, this is really where SMILE shines. Patients like that there is no flap involved and no mechanical cutting—just the laser.
It is important to stress to patients that LASIK is better than ever. It can treat nearsightedness, farsightedness, astigmatism, and aberrations (which we sometimes call hills and valleys). In this context, SMILE can and should be brought up and offered as another option that may be better in a particular patient’s case. At least in theory, SMILE could offer the following potential benefits.
No. 1: A more comfortable postoperative period. The subbasal nerve plexus is affected less in SMILE than with a LASIK flap, and the incision typically lies under the upper eyelid.
No. 2: Faster return to physical activities. Although cap dislocation can occur, it is rare. SMILE may be preferred by mixed martial arts fighters and oil and gas workers, among individuals with other athletic interests and physically demanding careers. Patients may also go back to wearing eye makeup sooner after SMILE than after LASIK or PRK.
No. 3: A stronger cornea. SMILE most likely leaves the cornea stronger than either LASIK or PRK.3 Ectasia can still happen, but it may be less likely.
No. 4: Useful in eyes with large pupils. Patients still ask about this. Effective optical zones have been shown to be larger after SMILE than LASIK even when the same optical zone is programmed.4
It is equally important to discuss the potential cons.
No. 1: Potentially slower visual recovery. Although it can improve with surgeon experience and optimized parameters, visual recovery after SMILE tends to be slower.5
No. 2: Future enhancements. Given that the cap for SMILE is locked in at 120 µm in the United States, thin-flap LASIK is difficult, especially after any epithelial remodeling. PRK is the recommended enhancement strategy. Future options may include Circle (converting the SMILE cap to a LASIK flap) and a second SMILE procedure.
No. 3: Limited range. Astigmatic correction is limited to the range of 0.75 to 3.00 D programmed, and hyperopia cannot yet be treated.
SMILE 3.0?
SMILE is impressive in that it has already become a rival to LASIK in a short time. Just like other forms of vision correction, it will continue to improve. LASIK, PRK, phakic IOLs, and lens-based refractive surgery are all significantly better today than their first generations, and SMILE is already better than it was just a few years ago.
There are many things to look forward to in the future of SMILE.
Unlocking parameters. We look forward to having the ability to vary the thickness of the lenticule, change the location and size of the primary incision, vary the cap thickness to allow LASIK enhancements, and change energy settings even further.
Treating hyperopia and aberrations. Studies are already being done for hyperopia.
Developing new techniques. New ideas are always being generated. It is important to stay current.
conclusion
It is exciting to have another option for laser vision correction. There are many reasons that SMILE is growing so quickly in popularity, and we are proud to offer it in our practices.
As the articles in this cover focus look to the future of ophthalmology, it is helpful to keep in mind that SMILE will perform best when we evaluate each patient as an individual to determine the optimal personalized treatment modality for that patient. The procedure will not thrive so well in an environment in which competition leads practitioners to express negativity about certain laser vision correction options (because they don’t happen to offer them but the practice across town does). Let us hope that the future of ophthalmology makes room for all safe and effective refractive surgical options so that we can best serve each and every patient.
We look forward to SMILE 3.0 and other future iterations.
SIX TIPS for GETTING STARTED WITH SMILE
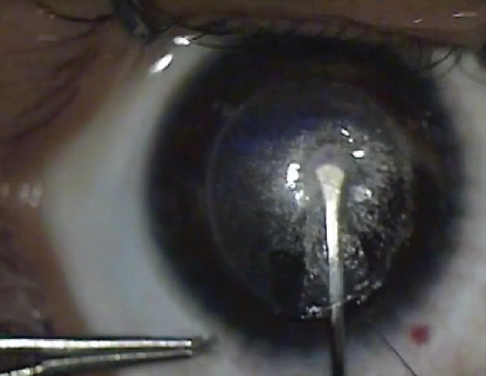
Figure 1. Perceived anterior dissection but in the posterior plane.
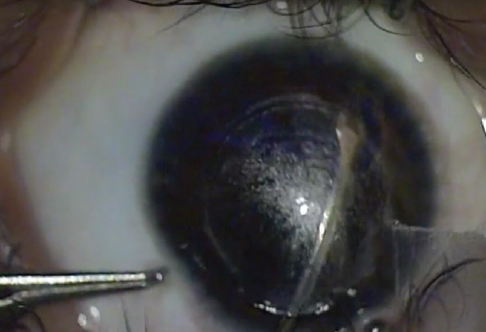
Figure 2. A visible bubble in the anterior segment is a clue that you are in the posterior plane.
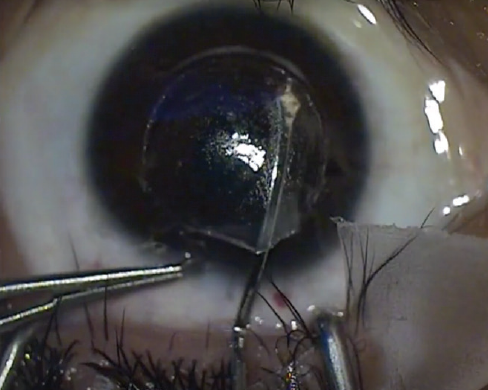
Figure 3. Rescue technique to find and dissect the anterior plane.
1. Reinstein DZ, Archer TJ, Gobbe M. Small incision lenticule extraction (SMILE) history, fundamentals of a new refractive surgery technique and clinical outcomes. Eye Vis (Lond). 2014;1:3.
1. VisuMax Femtosecond Laser. Small incision lenticule extraction (SMILE) procedure for the correction of myopia. Professional use information. Carl Zeiss Meditec. 2016. https://www.accessdata.fda.gov/cdrh_docs/pdf15/P150040D.pdf. Accessed May 2, 2019.
2. Premarket approval. US Food and Drug Administration. VisuMax Femtosecond Laser. Femtosecond laser system for refractive correction. October 25, 2018. https://www.accessdata.fda.gov/cdrh_docs/pdf15/P150040S003D.pdf. Accessed May 2, 2019.
3. Reinstein DZ, Archer TJ, Randleman JB. Mathematical model to compare the relative tensile strength of the cornea after PRK, LASIK, and small incision lenticule extraction. J Refract Surg. 2013;29(7):454-460.
4. Hou J, Wang Y, Lei Y, Zheng X. Comparison of effective optical zone after small-incision lenticule extraction and femtosecond laser-assisted laser in situ keratomileusis for myopia. J Cataract Refract Surg. 2018;44(10):1179-1185.
5. Chiche A, Trinh L, Saada O, et al. Early recovery of quality of vision and optical performance after refractive surgery: Small-incision lenticule extraction versus laser in situ keratomileusis. J Cataract Refract Surg. 2018;44(9):1073-1079.