I have developed two novel allogenic donor cornea therapies, one for the treatment of keratoconus and one for the treatment of presbyopia.
CAIRS. Corneal allogenic intrastromal ring segment (CAIRS) implantation can be performed in isolation or in combination with CXL. For this procedure, intrastromal corneal ring segments (ICRSs) are fashioned from human donor corneal tissue and implanted in a manner similar to that for standard synthetic ICRSs. Depending on whether the keratoconus is progressive or not, CAIRS can be combined with CXL to strengthen the cornea. Using donor corneal tissue instead of synthetic ICRSs avoids the possible complications associated with implanting synthetic material in the cornea, including implant extrusion, intrusion or migration; neovascularization; corneal melt; corneal necrosis; and infection.
Each allogenic ICRS is obtained from a donor corneoscleral rim that has been de–endothelialized and de–epithelialized and cut to shape with a double-bladed trephine (patent pending). Allogenic ICRSs are more flexible than synthetic ones. Because they are more biocompatible than ICRSs, they are less likely to be extruded or migrated and they can be inserted at 50% corneal depth rather than at 75% to 80%, as with synthetic implants. The shallower insertion plane can enhance the ability of the ICRS to reshape the cornea, and it can be used in a wider range of eyes with more severe thinning and/or steepening.
In the CAIRS procedure, a femtosecond laser–dissected channel is created with two entry incisions 180º apart. The allogenic tissue is pushed in gently from one side of the channel arc with a blunt rod and then pulled in from the other side with a reverse Sinskey hook. The same is repeated with the second segment for the other half arc of the channel. The ends are trimmed and positioned within the channels. After the segments are in place, epithelium-off accelerated CXL or contact lens–assisted CXL is performed, depending on the minimum corneal thickness. (For a primer on the technique, see http://bit.ly/Jacob0619 and http://bit.ly/Jacob0619b).
I have performed CAIRS in a large series of patients. In my experience, patients achieve good refractive and topographic outcomes, including regularization of the cornea and centralization of the cone, decreased aberrations, and decreased regular and irregular astigmatism (Figure 1). I have used the technique for all stages of keratoconus, from mild to advanced, with very good results.
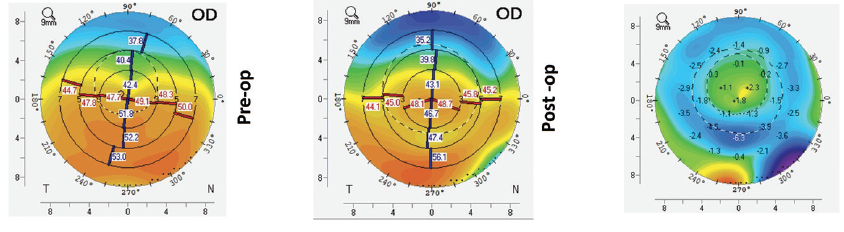
Figure 1. Preoperative (left), postoperative (middle), and topographical difference maps (right) after CAIRS implantation.
PEARL. Another procedure I have developed is presbyopic allogenic refractive lenticule (PEARL) implantation. PEARL is designed to treat presbyopia by using allogenic donor tissue. For this purpose, we used a lenticule of suitable thickness obtained from a small-incision lenticule extraction procedure performed on a young myopic donor planned for refractive surgery, as it was easy to obtain in the absence of other precisely shaped and sized allogenic tissue.
Once implanted, the PEARL inlay alters the cornea’s central radius of curvature and results in a hyperprolate central corneal contour. Made of allogenic material, the biocompatible inlay allows oxygen and nutrients to pass freely through the cornea, unlike some synthetic corneal inlays. This ensures a stable cornea, decreases the risks of corneal necrosis and melt that have been seen with synthetic inlays, and avoids the inflammation related to insertion of a synthetic material into the cornea.
To perform PEARL, the donor lenticule is marked at its center and cut with a trephine to a 1-mm diameter. It is then implanted in the cornea underneath a 120-µm femtosecond laser cap, centered on a coaxially sighted light reflex (Figure 2). The lenticule is implanted in the nondominant eye to provide improved near and intermediate vision. (For a primer on the technique, see http://bit.ly/Jacob0619c). In my experience, patients have good binocular uncorrected distance and near visual acuity, but they do need to be cautioned to expect some decrease in uncorrected distance visual acuity in the treated eye.
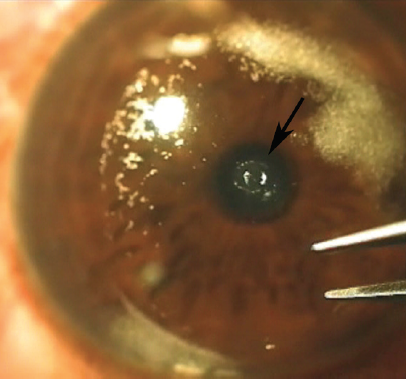
Figure 2. The PEARL lenticule (arrow) is inserted under a cap in the patient’s nondominant eye.

Soosan Jacob, MS, FRCS, DNB
- Director and Chief, Dr. Agarwal’s Refractive and Cornea Foundation, and Senior Consultant, Cataract and Glaucoma Service, Dr. Agarwal’s Eye Hospital, Chennai, India
- dr_soosanj@hotmail.com
- Financial disclosure: Dr. Jacob has a patent pending for shaped corneal segments and for the devices and processes used to manufacture them


