By Robert J. Cionni, MD
Just a couple of years ago, providing surgical care to a cataract patient who desired spectacle freedom required intensive effort. Any error in preoperative measurements, data input, IOL power calculation, or astigmatism reduction calculation (for limbal relaxing incisions or a toric IOL) could lead to residual refractive error and, thus, an unhappy patient. Additionally, the time required of the surgeon and technician to plan each procedure was burdensome and fraught with the possibility of human error, which meant yet more time spent on double- and triple-checking each surgical plan. Errors in the execution of the surgical plan were also possible, especially as the ophthalmologist tried to align arcuate incisions or a toric IOL in the proper axis. These mistakes, too, resulted in an unwanted outcome.
Fortunately, the recent availability of several technologies is making the planning and execution of the surgical plan more efficient while also decreasing the chance of human error. This, in turn, is increasing precision to a level not seen before. I have had the opportunity to work with two of these technologies.
The Verion Image Guided System
Verion, the advanced surgical planning and guidance system from Alcon, digitally uploads the preoperative images and measurements it captures (Figure 1). I no longer spend hours after clinic completing each surgical plan. The digital upload of data into the system eliminates the possibility of human errors in transcription, which are much more common than one might believe. The system matches the steep corneal axis with a preoperative image. It digitally matches the visual axis, corneal diameter, undilated pupil, limbal vessels, and iris elements to the femtosecond laser and OR microscope, thus helping to ensure precise centration of the IOL as well as accurate placement of corneal incisions and toric IOLs. In the OR, I have found that Verion eliminates the time needed for and the uncertainties of typing in the plan and manually marking the eye.
The system seamlessly integrates the preoperative diagnostic equipment and surgical plan with the femtosecond laser, operating microscope, and Centurion Vision System (Alcon). Known as Alcon's Verion Cataract Refractive Suite, this combined platform is already making my job of ensuring the best possible refractive outcomes for my patients more efficient and more accurate.

Figure 1. The Verion reference unit and surgical planner.

Figure 2. VerifEye+ toric alignment tool with pupil tracking via a dynamic reticle.
VerifEye+
VerifEye+ is the newest upgrade of Alcon WaveTec's intraoperative aberrometer. This sophisticated device permits me to measure the aphakic refractive error in real time after removal of the cataract but before selection, placement, and alignment of the IOL. Data are constantly displayed in real time. Moreover, the pupil is now tracked to allow for easier and faster alignment of a toric IOL or placement of corneal arcuate incisions guided by an overlay seen through the surgeon's oculars and displayed on a video monitor (Figure 2). In a recent, randomized, collateral eye study comparing VerifEye+ to the Alcon Toric Calculator (111 eyes per group), 13% more eyes in the former group ended up with less than 0.50 D of residual refractive astigmatism 1 month postoperatively (data on file with Alcon).
THE FUTURE
Having purchased WaveTec Vision, Alcon now plans to integrate VerifEye+ into its Verion Cataract Refractive Suite by merging the best features of each system. Doing so should better ensure proper spherical IOL power, toric IOL power, and toric IOL alignment and thereby enable surgeons to achieve better refractive outcomes.
Today's patients have higher expectations of cataract surgery than their predecessors. With the registration capabilities of Verion and the wavefront capabilities of VerifEye+—which takes into account all astigmatism, including posterior corneal cylinder—I expect it to become possible for surgeons to attain LASIK-like results for cataract patients.
By Jonathan Solomon, MD
When conversing with a patient about premium IOLs, I typically use the analogy of buying a new car. I liken presbyopia-correcting lenses to the upgrades of heated seats, satellite radio, or a factory-installed ice chest. I compare the astigmatism-correcting package to an airbag. In other words, total spectacle independence is a luxury, whereas the reduction of visual distortion is a safety feature. Studies have shown that corneal astigmatism is present in a majority of patients undergoing cataract surgery, with three-quarters of all eyes having 0.50 D or more.1,2
Even so, there are a few things to consider when moving forward with astigmatic correction, and as is the case with most procedures, the outcome of each step is predicated on the success of the previous one. Inversely, the inherent error can be stackable. First, the rotational stability of current toric IOLs is well documented, and the overwhelming majority typically remains seated once placed with little variability.3-5 As newer lens designs become available, rotational stability will play a minor role in residual refractive-cylindrical error.6 Second, surgically induced astigmatism is a multifaceted variable that can be managed by improving wound architecture. A femtosecond laser is capable of reproducibly creating corneal incisions that significantly reduce the variability in surgically induced astigmatism,7 and assuming consistency in the orientation and size of the incision, predictability of the surgical impact will improve. Understanding the contribution of the posterior corneal power addresses a third important dynamic. What remains is human fallibility: errors of reference, axis identification, and alignment. How well do cataract surgeons recognize the landmarks for the horizontal meridian and then find the steep axis and place the astigmatic correction at the ideal location?
TECHNOLOGICAL ASSISTANCE
Collaboration among i-Optics, TrueVision Systems, and Lensar has simplified achieving astigmatic neutrality during IOL surgery by eliminating the guesswork. No longer do I rely on the marking pen and bubble level to avoid the effects of cyclorotation. Nor do I manually indent the cornea with markers under the slit lamp or operative microscope. Instead, the Cassini Corneal Shape Analyzer (i-Optics) obtains a high-quality image of the eye with an undilated pupil. The device gathers both anterior and posterior curvature data and compiles the information into true corneal power with what I find to be unprecedented reproducibility. (For more information on the technology, go to eyetube.net/?v=oohef.)
Figure 1. Cassini eye image with iris scroll and infrared Lensar image with iris scroll in preparation for registration.
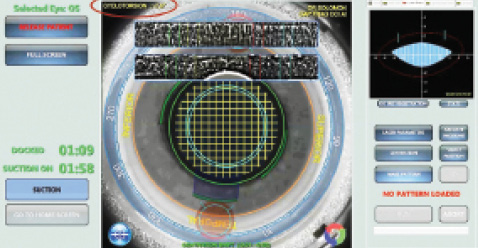
Figure 2. Lensar image after iris registration and nomogram adjustment with compensation of 7º of cyclorotation.
Wirelessly, the image and the necessary information on magnitude and axis are delivered to the Lensar Laser System (Lensar). The laser's Scheimpflug camera rapidly images the eye by simultaneously capturing an on-axis view and with an offset of 45º, by means of proprietary software. The dilated iris is “unscrolled” and registered like a fingerprint to the preoperative, in-office Cassini-captured infrared eye image. In less than a second, reference and identification errors disappear without being hindered by the difference in pupillary size (Figures 1 and 2).
Once registration is confirmed, the surgeon can create arcuate incisions or place small intrastromal guidance marks. In the case of astigmatic keratotomy, a default or site-specific nomogram is spontaneously presented to the surgeon for consideration in the graphical user interface. Axial identification and the placement of astigmatic correction are now automated. Alternatively, if a toric lens has been selected, the patient can be moved to the surgical microscope after the laser portion of the cataract procedure. The surgeon can then use the heads-up monitor of the TrueVision 3D Visualization and Guidance System (TrueVision), which is also powered by the Cassini Corneal Shape Analyzer. After the system completes a two-step validation with subsequent scleral-limbal registration, the surgeon lays the toric lens underneath the axial alignment mark presented.
MY EXPERIENCE
If my staff and I are ultimately able to reduce the workload in the office while simultaneously improving surgical accuracy, we expect greater practice efficiency. Already, wireless plug-and-play integration has reduced so-called stackable error at my practice, both clerically and surgically. As a result, astigmatic correction during IOL surgery can now be faster, safer, easier, and more repeatable.n
1. Hill W. Expected effect of surgically induced astigmatism on AcrySof Toric intraocular lens results. J Cataract Refract Surg. 2008;34(3):364-367.
2. Khan MI, Muhtaseb M. Prevalance of corneal astigmatism in patients having routine cataract surgery at a teaching hospital in the United Kingdom. J Cataract Refract Surg. 2011;37(10):1751-1755.
3. Bausch & Lomb Incorporated. Study 650. 2013.
4. Tecnis Toric 1-Piece IOL [package insert]. Santa Ana, CA: Abbott Medical Optics Inc.; 2012.
5. Alcon, Inc. Results of a controlled, randomized, double masked, multicenter, contralateral implant clinical study of the AcrySof IQ IOL. 2006.
6. Buckhurst PJ, Wolffsohn JS, Naroo SA, Davies LN. Rotational and centration stability of an aspheric intraocular lens with a simulated toric design. J Cataract Refract Surg. 2010;36(9):1523-1528.
7. Álvarez-Rementería L, Blázquez V, Contreras I. Surgical induced astigmatism in femtosecond laser assisted cataract surgery. J Emmetropia. 2012;3:61-65.
Robert J. Cionni, MD
- medical director, The Eye Institute of Utah, Salt Lake City
- adjunct clinical professor, The University of Utah, John Moran Eye Center, Salt Lake City
- (801) 266-2283
- consultant to Alcon and Alcon WaveTec
Jonathan Solomon, MD
- surgical/refractive director, Solomon Eye Physicians and Surgeons, Greenbelt and Bowie, Maryland, and McLean, Virginia
- jdsolomon@hotmail.com
- consultant to i-Optics, Lensar, and TrueVision Systems


