Many different types of IOLs have been developed in the continuous search to correct presbyopia. In the early 1990s, Storz Ophthalmics developed the bifocal zonal IOL, and 3M created the diffractive multifocal IOL. Many other companies such as Iolab, Domilens, AMO, and Pharmacia followed suit. Although these lenses were able to correct near vision, they were also associated with many secondary effects such as large amounts of halos and glare. Diffractive multifocal implants use a platform based on scattered waves that interfere constructively if they are in phase and destructively if they are out of phase.1
EARLY MODIFICATIONS AND RESULTS
Accommodating lenses underwent many modifications in the early days. The Crystalens AT-45 accommodating IOL (Eyeonics) received its premarket approval in November 2003. In more recent years, the Crystalens Five-O, Crystalens HD, and the Crystalens AO (all from Bausch + Lomb) were developed.
In a review of the literature, the Crystalens AO was associated with a statistically significant better uncorrected intermediate visual acuity and distance-corrected intermediate visual acuity than the AcrySof IQ Restor +3.0 D (Alcon) or the Tecnis Multifocal Lens (Abbott Medical Optics) and fewer photic phenomenon than the Tecnis Multifocal Lens.2 These findings may guide IOL selection for patients seeking to optimize vision at specific vergences or lighting conditions.

Figure 1. Oculentis’ Lentis Mplus IOL.

Figure 2. Physiol released the first-ever trifocal IOL.
NEW CONCEPTS
In early 2009, Oculentis introduced its Lentis Mplus IOL in European trials (Figure 1). The lens incorporated a new optical concept: its optical rotation was asymmetrical, with the shape of the near-vision segment providing seamless transitions between near- and far-vision zones.3 The Mplus is pupil independent, and the near-vision sector is asymmetrical, which demands perfect pupillary centration. If this lens becomes decentered, visual symptoms will result. To resolve this problem, surgeons have tried to place the near segment superiorly. Although this change seemed to slightly reduce early dysphotoptic symptoms, it had no long-term advantage. Consequently, the manufacturer introduced the Mplus X with a design that features a wider multifocal segment and increased asphericity, implying that some extra near vision is achievable.4
In 2010, Physiol released the first-ever trifocal IOL (Figure 2). Bifocal diffractive implants allow patients some spectacle independence for distance (> 1 m) and near (35-40 cm) vision. These lenses, however, have not been shown to provide satisfactory intermediate vision (eg, for activities such as computer work and reading). Glasses may be required for distances between 60 and 80 cm despite satisfactory near and disctance UCVA.
Figure 3. The FineVision IOL’s diffractive area extends throughout the anterior side of the lens.
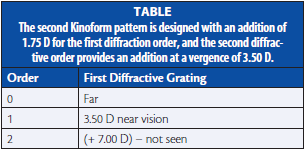
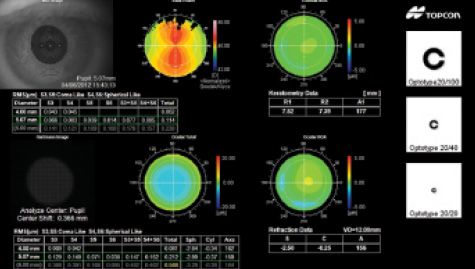
Figure 4. The small amount of halos induced by these IOLs gradually diminishes over the first 3 to 6 months after surgery.
The profile of the FineVision IOL (Physiol; Figure 3) can be thought of as a combination of two profiles (the design of the IOL and the kinoform pattern or the light waves created by the implant’s profile) and displays a full diffractive area with a specific diffractive pattern comprising alternating diffractive steps of different heights. This diffractive area extends throughout the anterior side of the IOL. The zeroth-order (identical for the two patterns) of the two profiles is used for far vision. In this innovative IOL design, the first kinoform pattern is designed with an addition of 3.50 D as the first diffractive order. Therefore, the second diffractive order occurs at a vergence of 7.00 D, which corresponds to lost light.
The second kinoform pattern is designed with an addition of 1.75 D for the first diffraction order, and the second diffractive order provides an addition at a vergence of 3.50 D (Table). The vergence of the first order of the second kinoform pattern is half of the first kinoform pattern addition power; hence, its first order contributes to intermediate vision, and its second order enhances near vision. The percentage of lost energy, which is usually 20% for standard diffractive, bifocal lenses, is reduced with this IOL to approximately 14%. The lens’ diffractive profile is also gradually attenuated throughout the entire optic, resulting in a continuous modulation of the light energy distribution directed to the three primary foci.5
In 2012, Carl Zeiss Meditec introduced the AT LISA tri 839MP IOL, and it provided very similar results to the FineVision lens. My Medline search found 15 peer-reviewed publications that confirmed this. Trifocality maintains distance and near vision performance and improves outcomes for intermediate vision. The third focal point, usable by the patient, does not create ghosting dysphotopsias.6
CONCLUSION
Having used many of the presbyopia-correcting IOLs available in Europe, I have found that it is still extremely important to get to know your patients’ lifestyle and expectations before choosing the IOL.
I implant about 75% of the patients in my practice with a trifocal IOL and 96% of these individuals are independent from glasses. The small amount of halos (Figure 4) induced by these IOLs gradually diminishes over the first 3 to 6 months after surgery. My patients find that the advantage of seeing well at intermediate distance is much more important than periodically being hindered by halos while driving at night.n
1. Percival SP. Prospective study of the new diffractive bifocal intraocular lens. Eye. 1989;3:571-575.
2. Pepose JS, Qazi MA, Chu R, Stahl J. A prospective randomized clinical evaluation of three presbyopia-correcting intraocular lenses after cataract extraction. Am J Ophthalmol. 2014;158(3):436-446.
3. Lentis Mplus and Lentis Mplus toric. Supplement to Cataract & Refractive Surgery Today. 2010;10(5).
4. Shah S. Assessment of a second-generation bifocal lens. Ophthalmology Times Europe. April 2014. http://www.oteurope.com/ophthalmologytimeseurope/Refractive/Assessment-of-a-second-generation-bifocal-lens/ArticleStandard/Article/detail/842257. Accessed January 13, 2014.
5. Gatinel D, Pagnoulle C, Houbrechts Y, Gobin L. Design and qualification of a diffractive trifocal optical profile for intraocular lenses. J Cataract Refract Surg. 2011;37(11):2060-2067.
6. Lesieur G. Outcomes after implantation of a trifocal diffractive IOL [in French]. J Fr Ophtalmol. 2012;35(5):338-342.
Erik L. Mertens, MD, FEBOphth
• chief medical editor of Cataract & Refractive Surgery Today Europe
• medical director of Medipolis in Antwerp, Belgium
• +32 3 828 29 49; e.mertens@medipolis.be; Twitter @Doktermertens
• consultant to STAAR Surgical, Bausch + Lomb, Ophtec, and PhysIOL


