The term middle segment surgery (MSS), as presented in this series of articles, is defined as a surgical approach involving entry through the pars plana to address anterior segment surgical challenges. This technique has been utilized for decades but has gained new indications in recent years. MSS is not limited to a specific subspecialty, such as vitreoretinal, cornea, or anterior segment surgery. It does, however, require subspecialists to broaden their skills. For instance, a cornea specialist or an anterior segment surgeon who undertakes MSS must first master basic pars plana vitrectomy techniques. This includes trocar placement; infusion; posterior viewing; utilization of 23-, 25-, and 27-gauge cutters; scleral closure; management of anticoagulation status; prevention of hemorrhage and hypotony; and inspection of the anterior retina. Conversely, a vitreoretinal specialist engaged in MSS must have a firm understanding of IOL materials and be skilled in biometry aimed at refractive outcomes, limbal wound construction, glaucoma and corneal endothelial damage prevention, and posterior chamber IOL scleral fixation methods in eyes lacking capsular support.
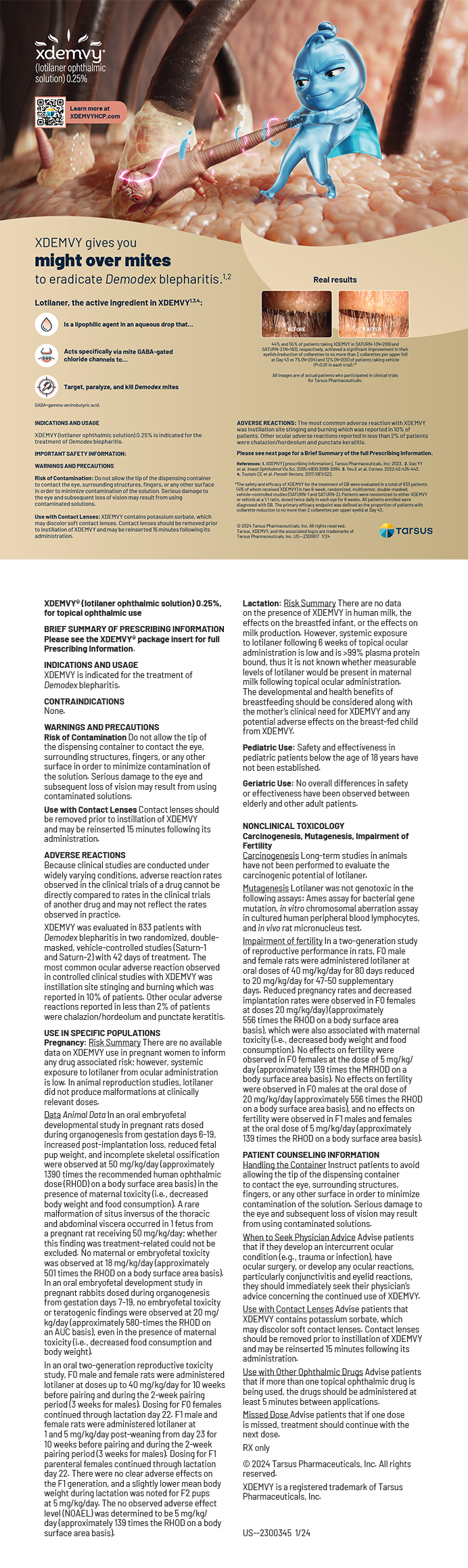
MSS is pertinent primarily in cases of visually significant IOL dislocation, often observed in patients with a history of pseudoexfoliation who present several years after successful cataract surgery (Figure 1) with a subluxated IOL–capsular bag complex. The pars plana approach can be useful in many other situations as well (see below to watch a related video):
- Shallow anterior chamber (Figure 2) in the context of cataract surgery;
- Retained cortex within the capsular bag in the setting of zonulopathy (Figure 3);
- Displaced cataractous crystalline lens in an eye with severe zonulopathy (Figure 4);
- Posterior infusion during endothelial keratoplasty in a unicameral eye (Figure 5);
- Aqueous misdirection syndrome after ultrasound confirmation of absent choroidals; and
- Vitreous decompression preceding a classic corneal triple procedure with open-sky cataract extraction and IOL implantation.
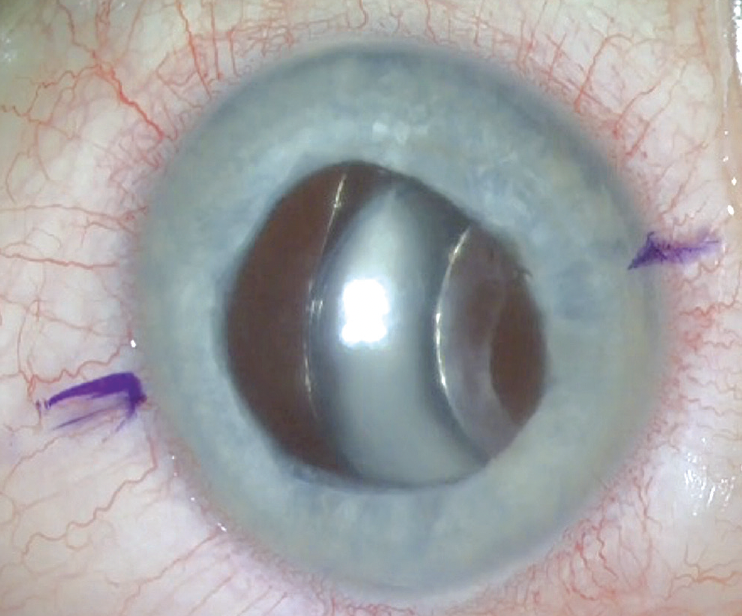
Figure 1. Dislocated IOL–capsular bag complex with a Soemmering ring.
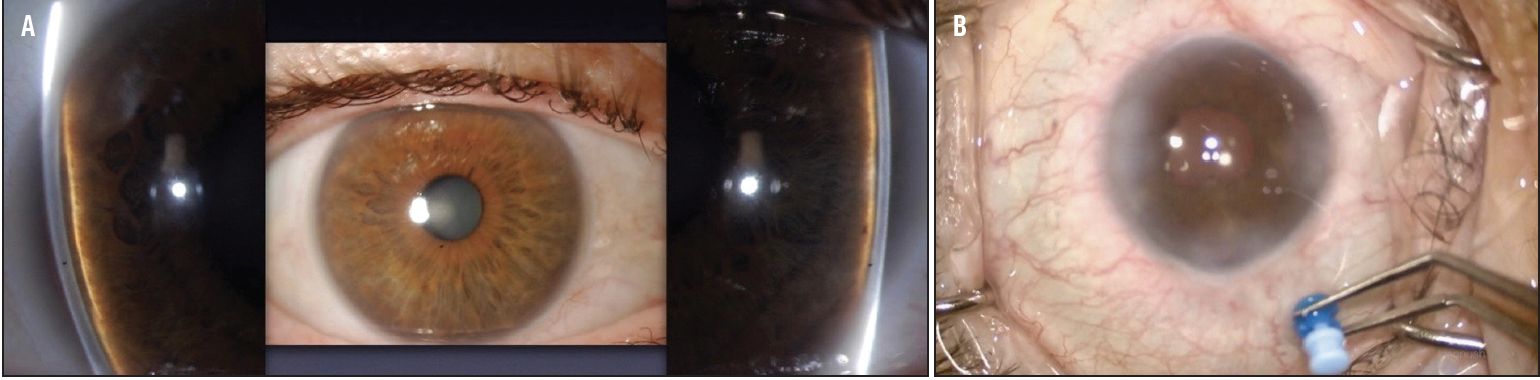
Figure 2. Cataract in eye with shallow anterior chamber (A). A 25-gauge cutter for 0.2-mL decompression of the vitreous cavity, facilitating the deepening of the anterior chamber with OVD (B).
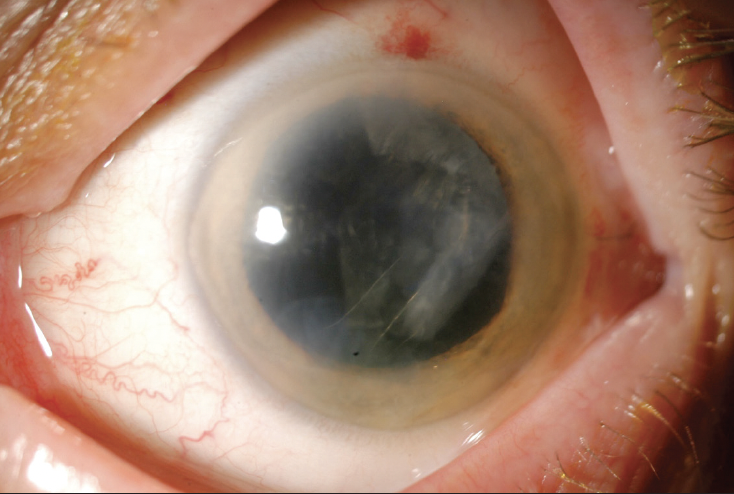
Figure 3. Retained cortex in the capsular bag in the setting of intraoperative zonulysis from 3 to 6 clock hours.

Figure 4. Subluxated cataract in an eye with 7 clock hours of zonulysis and severe phacodonesis.
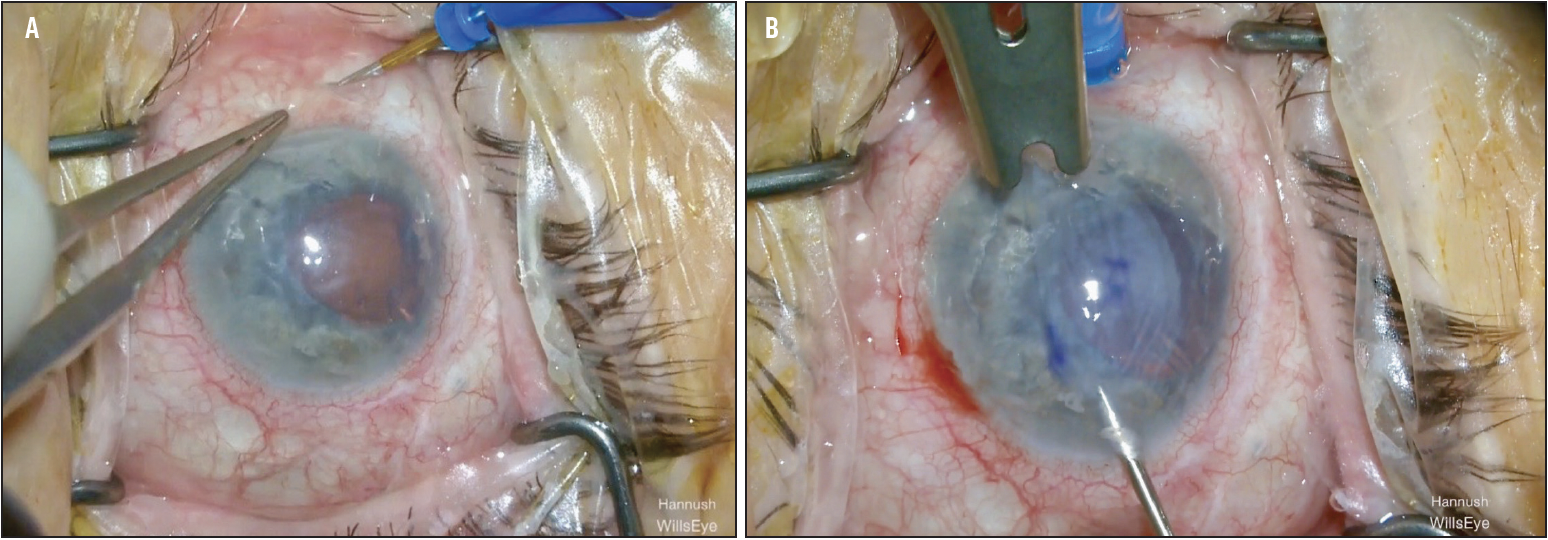
Figure 5. Sclerotomy in a unicameral eye before Descemet stripping endothelial keratoplasty (A). Descemet stripping endothelial keratoplasty graft pull through using posterior infusion to reduce the likelihood of posterior graft migration in a unicameral eye (B)
To integrate MSS into the lexicon and practice of ophthalmic surgery, several steps are essential:
- Training during or after formal residency/fellowship, supported by cornea/retina section chiefs and department heads through formal cross-training in postgraduate programs and inclusion in continuing medical education;
- Proper credentialing at hospitals and surgery centers, akin to the historical inclusion of phacoemulsification, laser cataract surgery, keratoplasty, intrastromal corneal ring segments, etc., with suggestions for terminology such as pars plana anterior vitrectomy or pars plana vitrectomy without posterior visualization. Some institutions/centers might opt for less specificity;
- Support from national organizations such as the AAO, ASCRS, Cornea Society, Retina Society, and American Society of Retina Specialists;
- Consideration of medicolegal implications, advice from liability carriers, and community standards; and
- Consideration of the practice model, volume/catchment area, and proficiency in MSS.
THE FUTURE OF MSS
Beyond MSS integration, surgeons, academic programs, private practice models, and industry must collaborate in the following ways:
- Advance biometry for accurate IOL power calculation in eyes with cloudy corneas;
- Make the acquisition and implementation of endoscopy technology more accessible;
- Enhance pre- and intraoperative imaging of the anterior segment to the pars plicata, likely through affordable OCT devices that aid real-time anatomic assessment by surgeons; and
- Improve ophthalmologists’ understanding of the utility of salvaging the capsular bag and techniques for capsular support.
Importantly, the industry, in cooperation with surgeons, should develop and obtain FDA approval for an IOL specifically designed for intrascleral fixation in the absence of capsular support. This would encourage more surgeons to adopt the technology and avoid the off-label use of other IOLs.
MSS plays a crucial role in enhancing surgical outcomes and patients’ quality of vision and life. This movement can be strengthened through concerted efforts by surgeons, training institutions, and industry.