Glued Scleral IOL Fixation Without Capsular Support
By Lisa Brothers Arbisser, MD

When faced with subluxated or secondary IOLs in eyes lacking capsular support, I recommend first considering all forms of optic capture. A simple lasso technique can be a strong choice for a subluxated capsular bag–IOL complex when a vitrectomy is otherwise unnecessary. If optic capture is not feasible, various options for IOL fixation may be considered. I’ve been asked to focus this article on glued scleral fixation.
TECHNICAL EVOLUTION
My approach to managing a subluxated IOL-capsular bag complex in an eye without capsular support has evolved over time. Initially, I performed anterior chamber IOL implantation with a large scleral tunnel incision. This approach shifted to the two-point iris fixation of a three-piece IOL. I employed iris fixation only briefly, however, because I abhorred touching uveal tissue.
I then briefly performed sutured scleral fixation of a one-piece PMMA lens, followed by a short period of four-point suture fixation of a hydrophilic acrylic IOL. The risk of calcification in certain eyes led me to settle on glue-assisted sutureless scleral tunnel fixation as my preferred method before the development of the flanged intrascleral haptic fixation (ISHF) technique popularized by Yamane and colleagues.1
Whatever form of IOL fixation is employed, the surgeon’s attention to detail is paramount to achieving excellent outcomes.
GLUED INTRASCLERAL IOL FIXATION
Background. Built on the sutureless Scharioth technique,2 glued scleral fixation of an IOL was first described by Agarwal and colleagues.3 This technique promotes a quiet eye by preventing pseudophacodonesis and minimizing vitreous traction. It also avoids large incisions, irritation of uveal structures, and sutures or flanges that can give way or extrude. Additionally, repositioning the lens to the sulcus is relatively predictable for refractive calculation.
Compared to the Yamane technique, there is less likelihood of IOL tilt with glued fixation because the lens haptics are parallel with the limbus and sequestered in Scharioth tunnels. Furthermore, this method circumvents the unpredictability associated with flange formation.
The keys to success with this technique are ensuring an adequate vitrectomy is performed, maintaining normotension via an anterior chamber maintainer or a trocar system, and protecting the endothelium during the procedure. When these steps are meticulously followed, surgical outcomes with glued IOL fixation are generally excellent.4
The technique in detail. Under a fornix-based peritomy, a guarded blade is used to create partial-thickness intrascleral flaps, which are precisely positioned 180º apart using a toric marker in a meridian determined by the measured anatomy of the anterior segment. The placement of these flaps, either superiorly or horizontally, may be influenced by an atypical white-to-white distance because the haptics have a fixed dimension. The eye must have sufficient conjunctiva to cover the flaps.
A belt loop is created with a crescent blade that enters through a groove perpendicular to the limbus, with an outward sweeping motion employed to create a flap that opens away from the limbus.
In cases where the eye has not undergone vitrectomy, a thorough anterior vitrectomy is performed. This is achieved by creating sclerotomies 2 mm from the limbus under each flap using a 23-gauge microvitreoretinal blade. A three-piece IOL is then inserted through a clear corneal incision. The leading haptic is grasped with microforceps through the sclerotomies under one of the partial-thickness scleral flaps. A handshake maneuver within the anterior chamber can facilitate grasping of the haptic tip for externalization (Figure 1). An assistant can hold the leading haptic in place, or the silicone stopper from an iris hook may be slipped over the exposed haptic to prevent it from falling back. After the lens optic has been completely removed from the inserter, the trailing haptic is externalized in a similar manner on the opposite side. Ideally, the optic is positioned at the level of the ciliary sulcus, with each haptic threaded through a limbus-parallel Scharioth scleral tunnel made with a 25-gauge needle at both ends of each flap. This maneuver centers the IOL.5
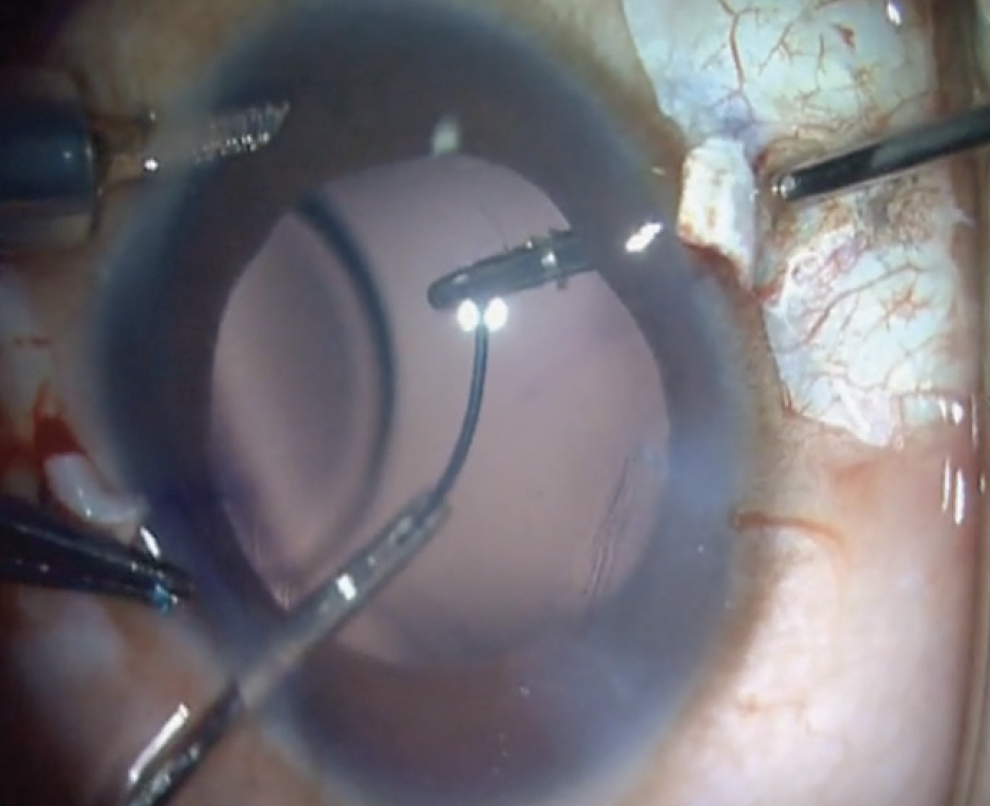
Figure 1. The glued IOL technique externalizes the IOL haptics through two sclerotomies. A handshake technique is used to transfer the tip of the trailing haptic from one set of forceps to another.
(Figure 1 courtesy of Amar Agarwal, MD)
A prophylactic peripheral iridectomy is prudent to avoid optic capture with reverse pupillary block, which is rare and avoidable. Irrigation is halted, an air bubble is placed in the anterior chamber, excess moisture is dried, and the flaps, along with the overlying Tenon and conjunctival tissue, are sealed with glue.
I recommend performing an (off-label) intracameral injection of moxifloxacin.
Challenges and drawbacks of the technique. As seen in the accompanying video, the haptics of a lens that has been in place for some time can be crimped or broken unintentionally during IOL fixation.
One disadvantage of the glued fixation technique is the necessity for a peritomy. This step requires a significant amount of time, may result in cosmetically unappealing outcomes, and reduces the space available for potential future filtration surgeries. Additionally, creating scleral flaps and tunnels with the correct depth poses its own set of challenges. Perhaps the most significant concern with this technique is the reliance on fibrin glue, which is costly and carries a risk of prion contamination, although this is a subject of debate. Furthermore, the practice of injecting air into the eye to dry the area for glue application is undesirable because it may damage the endothelium.
CONCLUSION
There is no solution for IOL fixation that suits every surgical situation. Ophthalmologists must therefore be able to draw from a variety of techniques and tools to tailor their approach to the specific needs of each case.
1. Yamane S, Sato S, Maruyama-Inoue M, Kadonosono K. Flanged intrascleral intraocular lens fixation with double-needle technique. Ophthalmology. 2017;124(8):1136-1142.
2. Gabor SG, Pavlidis MM. Sutureless intrascleral posterior chamber intraocular lens fixation. J Cataract Refract Surg. 2007;33(11):1851-1854.
3. Agarwal A, Kumar DA, Jacob S, Baid C, Agarwal A, Srinivasan S. Fibrin glue-assisted sutureless posterior chamber intraocular lens implantation in eyes with deficient posterior capsules. J Cataract Refract Surg. 2008;34(9):1433-1438
4. Kumar DA, Agarwal A, Dhawan A, et al. Glued intraocular lens in eyes with deficient capsules: Retrospective analysis of long-term effects. J Cataract Refract Surg. 2021:1:47:4:496-503.
5. Agarwal A. A Video Textbook of Glued IOLs. Slack; 2016.
IOL Fixation Techniques
By Megan Haghnegahdar, MD, and Brandon D. Ayres, MD


Over the past several years, an increasing number of anterior segment surgeons have adopted a pars plana approach to the management of complex cases. An anterior vitrectomy via the pars plana may be the method of choice when vitreous interaction is likely. Such situations include repositioning an IOL when the capsular bag might have been compromised, exchanging an IOL in the presence of an open posterior capsule or lost capsular support, and performing cataract surgery in an eye with zonulopathy due to trauma or disease (eg, Marfan syndrome or homocystinuria).
Certain cases, however, are unsuitable for an anterior vitrectomy via the pars plana. If the IOL or crystalline lens has dislocated entirely into the posterior segment or is resting on the macula, it is more appropriate to refer the patient to a retina specialist for a pars plana vitrectomy (PPV) with a wide-angle viewing system. An anterior vitrectomy via the pars plana should also be avoided in patients with a formed vitreous, such as young patients, those without a posterior vitreous detachment, or those with peripheral retinal pathology that significantly increases their risk of retinal detachment. Most anterior segment surgeons are not trained in using the posterior viewing systems necessary to handle these procedures safely.
TECHNOLOGICAL ADVANCES IN ANTERIOR VITRECTOMY EQUIPMENT
The evolution of vitrectomy units, fluidics, and phaco software has greatly enhanced the safety of anterior vitrectomy. Being knowledgeable about the specific capabilities and limitations of the equipment used is essential to success. The Centurion Vision System (Alcon) employs a 23-gauge vitrector at a cut rate of 4,000 cuts per minute (cpm), whereas the Stellaris PC Elite (Bausch + Lomb) uses a 25-gauge vitrector at a cut rate of 7,500 cpm. Both the Veritas (Johnson & Johnson Vision) and Visalis 500 (Carl Zeiss Meditec) feature a 23-gauge vitrector, with cut rates of up to 3,000 and 4,000 cpm, respectively. Third-party vitrectors, such as the trocar-less 27-gauge Vista 1-Step (Vista Ophthalmics), are designed to facilitate a pars plana approach and are compatible with most anterior segment machines.
IOL SELECTION
Advanced optical biometry is helpful for IOL selection. It is important to identify whether the patient is phakic, pseudophakic, or aphakic before taking measurements. If the crystalline lens or IOL has dislocated severely, an aphakic measurement might be necessary. Corneal edema can make keratometry difficult; historical data and the patient’s IOL card can help determine the correct IOL power.
Modern formulas are suitable for selecting an IOL for placement in the bag. Outcomes should be monitored, however, and adjustments or a nomogram applied after several cases have been reviewed. If the IOL is to be placed in the sulcus, the spherical power is typically reduced by 0.50 D. For higher powers (17.50–28.00 D), Warren Hill, MD, has recommended a 1.00 D reduction. Developing a personalized nomogram based on data from past cases can assist with future IOL selection.
IOL secured with PTFE sutures. IOL fixation with PTFE sutures (Gore-Tex, W.L. Gore & Associates) can be an effective strategy when anterior segment abnormalities preclude traditional placement of the lens within the capsular bag, implantation in the sulcus, or fixation to the iris. Suitable IOLs for this method include the following:
- One-piece PMMA IOLs such as the CZ70BD (Alcon);
- One-piece foldable acrylic IOLs such as the enVista, enVista Toric, or Akreos (models MX60E, MX60ET, and AO60, respectively, all from Bausch + Lomb); and
- Three-piece IOLs such as the CT Lucia (Carl Zeiss Meditec) and Tecnis (model ZA9003, Johnson & Johnson Vision).
Scleral fixation. One-piece PMMA IOL. The advantages of this design are the large optic and thin haptics that extend from sulcus to sulcus, all of which facilitates centration, and the biocompatible material that remains clear even when exposed to air, surgical gases, or silicone. Drawbacks include the large (around 7.00 mm) incision required for lens insertion, heightened risk of hypotony during surgery, propensity for suture tangling or twisting, risk of late suture breakage and dislocation, and requirement for scleral wound management. Typically, the use of a CZ70BD IOL is reserved for situations in which a large wound is required to remove the original lens implant, such as with an anterior chamber IOL.
The scleral fixation of a one-piece PMMA IOL with PTFE sutures begins with marking the limbus with a sterile marking pen in two spots 180º apart (usually at the 6 and 12 clock positions) to bisect the visual axis. Conjunctival peritomies are then created over the designated scleral incision areas. The scleral incisions are made 3.00 mm posterior to the limbus and 4.00 mm apart with a trocar blade, with a trocar inserted in one of these incisions at both the 6 and 12 clock positions or wherever the predetermined sites for scleral fixation are located. An anterior chamber maintainer is placed in one of the paracentesis wounds. If necessary, a vitrectomy is performed through the pars plana. Subsequently, a temporal 7.00-mm wound is prepared for IOL insertion. A handshake technique is used to introduce the first strand of a PTFE suture into the anterior chamber through the main wound with microforceps, passed to another set of microforceps through a proximal scleral wound, and externalized.
For double-armed polypropylene sutures, a 25-gauge needle may be utilized to create the scleral incisions. The suture needle is introduced through the main wound and docked into the lumen of a 25-gauge guide needle, facilitating externalization on the scleral surface. The suture’s free end is extended from the main wound and looped around the IOL’s haptic eyelet, with care taken not to tilt or torque the lens. The same suture end is then reintroduced into the main wound with microforceps and externalized through a distal sclerotomy with the handshake technique.
The process is repeated for the second set of scleral wounds and second haptic. Next, the IOL is carefully inserted into the posterior segment through the main wound to avoid suture entanglement. The suture is then tied on the scleral surface with a slipknot or 3-1-1 knot, which is buried within the scleral wound. The scleral and conjunctival wounds are closed with a polyglactin (Vicryl, Ethicon) suture, and the corneal wounds are closed with a nylon suture. OVD is removed, and a repeat vitrectomy is performed if necessary.
Foldable acrylic IOL. Suture fixation of a foldable acrylic IOL is similar to that of the one-piece PMMA IOL. Notable differences are the smaller incision required for acrylic IOL insertion and the method of threading the suture through the eyelets. The enVista IOL features a hole at the haptic-optic junction that facilitates the lacing of a suture. The suture is strategically placed over the haptic, beneath the internal acrylic bridge, and then across the haptic-optic junction. This technique prevents IOL tilt and gently depresses the haptics to maintain distance from the iris and ciliary body. Other than the unique suture lacing around the IOL, the technique mirrors that used for suture fixation of an Akreos IOL.
Potential disadvantages of this method include the risk of induced astigmatism if the sutures are overly tight and the possibility of opacification when the IOL is exposed to air, surgical gases, or silicone oil. To date, opacification has not been reported with the enVista IOL.
Optic capture. In eyes with an intact anterior capsule capable of supporting an IOL despite an open posterior capsule, the sulcus fixation of an IOL may be a reasonable option. In this situation, a three-piece lens is often preferred. The critical step of this technique is capturing the optic of the IOL within the anterior or posterior capsulorhexis so that it cannot rotate or become decentered and dislocated. Should optic capture prove impracticable, an IOL with a rounded anterior edge, such as the Tecnis or SofPort (model LI61AO, Bausch + Lomb), is the best choice.
PARS PLANA APPROACH FOR ANTERIOR VITRECTOMY
The pars plana approach for anterior vitrectomy is an essential step in numerous procedures for anterior segment reconstruction, particularly the placement of an IOL in eyes lacking capsular support. This technique is becoming increasingly accessible to surgeons specializing in the anterior or middle segment of the eye owing to advances in anterior segment phaco systems, improvements in fluidics, and the availability of smaller-gauge vitrectors. That said, it is critical for surgeons to acknowledge their limits and undertake these procedures only if they feel confident and skilled in the specific techniques required. Adequate training in the use of the pars plana for vitrectomy is indispensable.
Optimizing Techniques for Flanged Intrascleral Haptic Fixation
By Beeran Meghpara, MD
ISHF represents a significant advance in methods for securing IOLs when capsular support is lacking. Since the technique’s introduction in 2017 by Shin Yamane, MD, PhD, double-needle ISHF has become increasingly popular.1 The scleral fixation of IOLs is not a novel concept, but transconjunctival ISHF offers several advantages over traditional methods. Notably, ISHF eliminates the need for sutures, reducing the risk of associated complications such as suture breakage and exposure, endophthalmitis, and long-term IOL dislocation.
SURGICAL TECHNIQUE
Several surgeons have modified the ISHF technique since it was originally described by Dr. Yamane. The use of scleral incisions necessitates more than topical anesthesia; a cut-down sub-Tenon or retrobulbar block is recommended.
ADDITIONAL SURGICAL PEARLS FOR ISHF
By Beeran Meghpara, MD
IOL considerations
Although most three-piece foldable IOLs are compatible with intrascleral haptic fixation, PVDF haptics offer superior resistance to manipulation-induced bending and breakage compared to PMMA haptics. The CT Lucia 602 (Carl Zeiss Meditec) is currently the only IOL with PVDF haptics available in the United States. There have been instances of IOL rotation due to loose haptic insertion into the optic.1
IOP maintenance
Maintaining IOP with an anterior chamber maintainer or posterior infusion is crucial during sclerotomy creation.
Vitrectomy
A thorough vitrectomy is recommended before IOL insertion to prevent vitreous traction, which can lead to retinal tears and detachment. Removal of the anterior vitreous must be complete, even in eyes that have previously undergone vitrectomy.
Optimal cauterization
The cauterized bulb at the end of the haptic should be of minimal size to avoid conjunctival erosion due to protrusion through the scleral surface.
Preventing reverse pupillary block
A peripheral iridotomy may be performed to mitigate the risk of reverse pupillary block.
1. Safran JP, Safran SG. Intraocular lens tilt due to optic-haptic junction distortion following intrascleral haptic fixation with the Yamane technique. Am J Ophthalmol Case Rep. 2023;30:101845.
The success of ISHF hinges on meticulous planning. Marks are placed for paired 2-mm tunneled sclerotomies 2.5 mm posterior to the 6:00 and 12:00 clock positions to ensure the incisions are exactly 180º apart, equidistant from the limbus, and of equal length. Through a clear corneal incision, a three-piece IOL is inserted into the anterior chamber. Each sclerotomy is created with a 30-gauge, thin-walled needle. The IOL haptics are docked into the needle’s lumen and externalized. Subsequently, a small bulb is fashioned at the end of each haptic with handheld, low-temperature cautery, buried under the conjunctiva, and embedded in the sclera. (Swatch a video below.)
FINAL THOUGHTS
The sutureless Yamane technique for IOL fixation is an invaluable tool for anterior segment surgeons. Combined with judicious selection of IOLs and careful surgical planning, ISHF is an effective solution for IOL fixation eyes lacking capsular support.
1. Yamane S, Sato S, Maruyama-Inoue M, Kadonosono K. Flanged intrascleral intraocular lens fixation with double-needle technique. Ophthalmology. 2017;124(8):1136-1142.
Improving Posterior Chamber IOL Fixation
By Shin Yamane, MD, PhD

The IOL fixation technique, originally reported by Scharioth and Agarwal, introduced a sutureless method of IOL fixation for eyes lacking capsular support.1,2 Although this innovative approach reduced the duration of surgery and mitigated IOL tilt, it also presented challenges, including postoperative hypotony. My colleagues and I developed the needle guide or double-needle technique with the aim of minimizing scleral wounds for haptic fixation.3 The method’s subsequent evolution into the flanged technique, known as the Yamane technique, facilitates transconjunctival surgery that can achieve strong haptic fixation.4
SURGICAL TECHNIQUE
A vitrectomy cutter is used to perform a peripheral iridotomy without mydriasis. A sub-Tenon block is then administered to dilate the pupil. Depending on the situation, a pars plana or anterior vitrectomy is performed before the dislocated IOL is removed. Angled sclerotomies are created with a 30-gauge thin-walled needle through the conjunctiva and positioned 2.5 mm from the limbus. The use of a needle stabilizer is helpful for maintaining a constant needle insertion angle during sclerotomy creation.5
A three-piece IOL is inserted into the anterior chamber, and the trailing haptic is kept external to prevent the IOL from falling into the vitreous cavity. Forceps are then used to insert the leading haptic into the needle’s lumen, after which the trailing haptic is introduced into a second needle’s lumen—thus the double-needle moniker. The haptics are externalized, cauterized to form flanges, and subsequently secured in the scleral tunnels.
MANAGING CHALLENGING CASES AND COMPLICATIONS
Dislocated three-piece IOL. Refixation of a dislocated three-piece IOL may be possible. Following the excision of the capsule surrounding the haptics, flanges are created. The haptic may be inserted directly into the vitreous cavity. Special attention is warranted if the IOL was initially fixated in the bag because haptic deformation may lead to lens tilt and decentration; thus, intracapsular IOL refixation is generally discouraged.
Weak zonules. If postoperative IOL dislocation is a concern due to zonular weakness, the flanged IOL fixation method can be employed during cataract surgery. Fixation is performed between the anterior capsule and iris, followed by optic capture. This method promotes long-term IOL stability without capturing the iris or necessitating a vitrectomy. It is a demanding technique that requires creation of an anterior capsular incision measuring 5 to 5.5 mm in diameter.
Postoperative iris capture. Postoperative iris capture is the most common complication of the Yamane technique. To prevent this, the haptic should be fixated 2.5 rather than 2 mm from the limbus. A peripheral iridectomy can help prevent reverse pupillary block and thereby reduce the incidence of iris capture. If iris capture occurs, mydriasis or optic manipulation with a 30-gauge needle can be attempted. Pilocarpine drops may be administered to prevent recurrence, but if they prove ineffective, a pupilloplasty may be performed.
FLANGE TECHNIQUES
Since the Yamane technique was first described, additional flange-based methods for IOL fixation, which I refer to as flange techniques, have been developed. For example, Sergio Canabrava, MD, introduced an innovative method for IOL fixation in which flanges are created at both ends of a 5-0 or 6-0 polypropylene suture.6 The Canabrava double-flanged technique broadens the scope of sutureless IOL fixation by also addressing iridodialysis and allowing a capsular anchor to be secured to the sclera.
CONCLUSION
The Yamane technique offers a minimally invasive method for secure haptic fixation. The needle insertion angle plays a crucial role in outcomes. The technique and flange-based adaptations represent a significant step forward for IOL fixation.
1. Gabor SG, Pavlidis MM. Sutureless intrascleral posterior chamber intraocular lens fixation. J Cataract Refract Surg. 2007;33:1851-1854.
2. Agarwal A, Kumar DA, Jacob S, et al. Fibrin glue-assisted sutureless posterior chamber intraocular lens implantation in eyes with deficient posterior capsules. J Cataract Refract Surg. 2008;34:1433-1438.
3. Yamane S, Inoue M, Arakawa A, Kadonosono K. Sutureless 27-gauge needle-guided intrascleral intraocular lens implantation with lamellar scleral dissection. Ophthalmology. 2014;121(1):61-66.
4. Yamane S, Sato S, Maruyama-Inoue M, Kadonosono K. Flanged intrascleral intraocular lens fixation with double-needle technique. Ophthalmology. 2017;124(8):1136-1142.
5. Yamane S, Maruyama-Inoue M, Kadonosono K. Needle stabilizer for flanged intraocular lens fixation. Retina. 2019;39(4):801.
6. Canabrava S, Canêdo Domingos Lima AC, Ribeiro G. Four-flanged intrascleral intraocular lens fixation technique: no flaps, no knots, no glue. Cornea. 2020;39(4):527-528.
When to Consider Iris Suture Fixation
By Sara Bozorg, MD

Evaluating a patient with a dislocated IOL can be daunting. The pupil is often small, which can make examination difficult, and it can be hard to identify the lens if it is hiding behind the iris or drifting in and out of view. Surgical planning is based on limited examination findings and then has to be explained concisely to the patient. I typically wrap up this explanation by saying, “We have plans A, B, C, and D and will decide the best approach during surgery.” Plan A is usually either lassoing a dislocated IOL or an IOL exchange with ISHF using the Yamane technique1 combined with a PPV. In certain situations, however, iris suture fixation (ISF) becomes plan A.
ISF is an elegant and successful approach in the right patient. A unique benefit of the technique is that it does not require conjunctival or scleral incisions. I keep the option of ISF in mind when seeing patients who have extensive conjunctival scarring, limited conjunctival real estate (ie, history of multiple glaucoma procedures), or thin sclera.
CASE EXAMPLE
An 89-year-old man presented with an inferiorly dislocated three-piece-IOL and no clear vitreous prolapse (Figure 2). Intraoperatively, more than 10 clock hours of residual capsule were observed, but the tissue was not robust enough to endure the creation of a posterior opening and attempted optic capture. Plan A was therefore ISF.
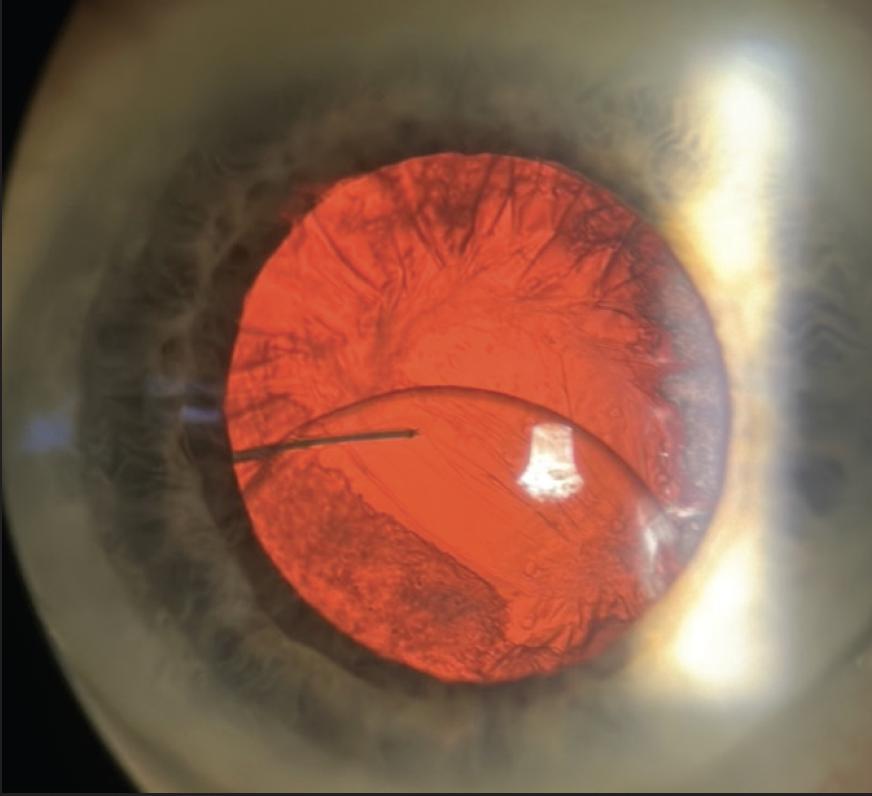
Figure 2. Dislocated three-piece-IOL with residual capsule present.
(Figures 2–5 courtesy of Sara Bozorg, MD)
The original IOL was removed. Triamcinolone acetonide (Triesence, Alcon) was injected, and an anterior vitrectomy was performed to address a minimal amount of prolapsed vitreous. A SofPort AO lens—the only IOL approved by the FDA for sulcus fixation—was implanted and secured with ISF. Another option would have been to place a lens with a rounded anterior optic such as the Tecnis (model ZA9003 or AR40e).
My reasons for performing ISF rather than ISHF in this case were that the former does not require a large PPV, removal of the residual capsule, or the creation of scleral incisions. Moreover, I was confident that the 10-0 polypropylene suture would not break in the patient’s lifetime.
PATIENT SELECTION
Alsetri et al recently defined the best conditions for ISF.2 They found that, when these were met, side effects were minimal, the incidence of postoperative cystoid macular edema was 4%, and it resolved with topical treatment. Their criteria were (1) no prior iris damage and (2) at least 270º (9 clock hours) of residual capsule. I usually add a third criterion for my patients based on my experience: no history of PPV.
THE TECHNIQUE IN 10 STEPS
Approaches to ISF vary. The technique I prefer was outlined by Ahmed et al.3 The following 10 steps are key to success:
No. 1: A three-piece lens (LI60AO or a lens with a rounded anterior optic) is placed in the anterior chamber.
No. 2: The haptics are positioned behind the iris, while the optic is kept in front of the iris.
No. 3: Acetylcholine is instilled over the iris after the IOL has been captured through the pupil.
No. 4: A paracentesis incision is made 1 clock hour away from where the haptic will be sutured.
No. 5: A 10-0 polypropylene suture (CIF-4, Ethicon) is passed through the paracentesis incision without catching corneal fibers.
No. 6: The lens optic is lifted with a blunt instrument. This outlines the haptic to be sutured (Figure 3).
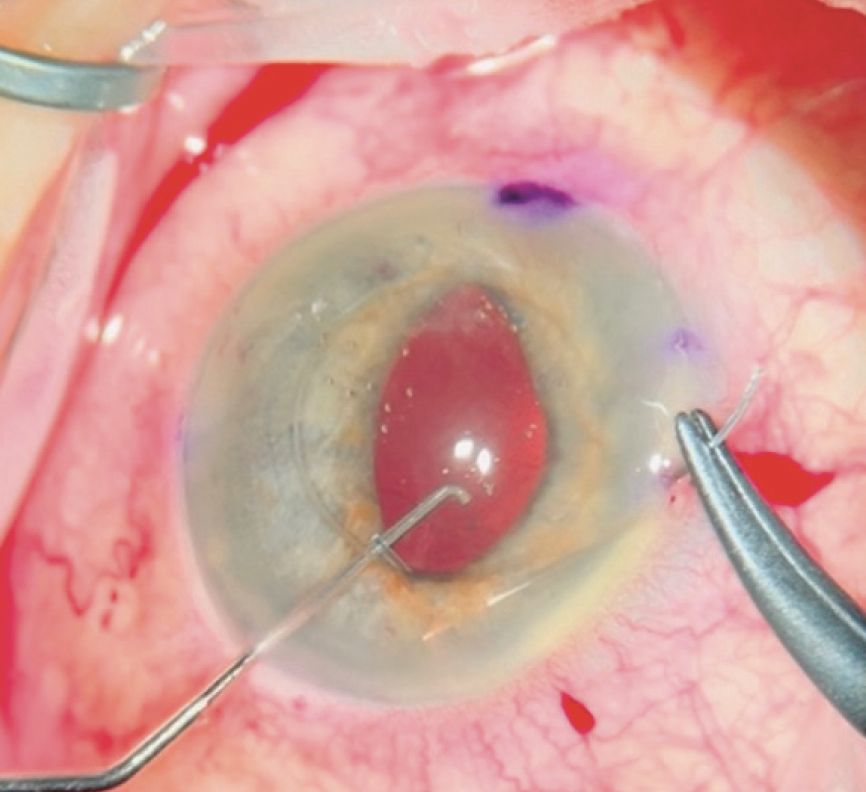
Figure 3. A blunt instrument pushes up on the optic to help outline the haptic for better visualization during suturing.
No. 7: The suture is passed across the anterior chamber and docked into a viscoelastic cannula. The bites should not be large or approach too close to the pupillary margin. The needle is docked into a viscoelastic cannula. Steps No. 4 through 7 are repeated on the other side before any knots are tied.
No. 8: Both sutures are tied with a double throw (the 2 in a 2-1-1 configuration). Either a modified Siepser sliding knot4 or an intraocular suturing technique (McAhmed knot)5 is used. The suture should not be locked yet.
No. 9: The lens is pushed gently behind the iris after the first double throw. Any iris tissue that has been trapped by the suture is gently pulled out with microinstruments to maintain a round pupil (Figure 4).
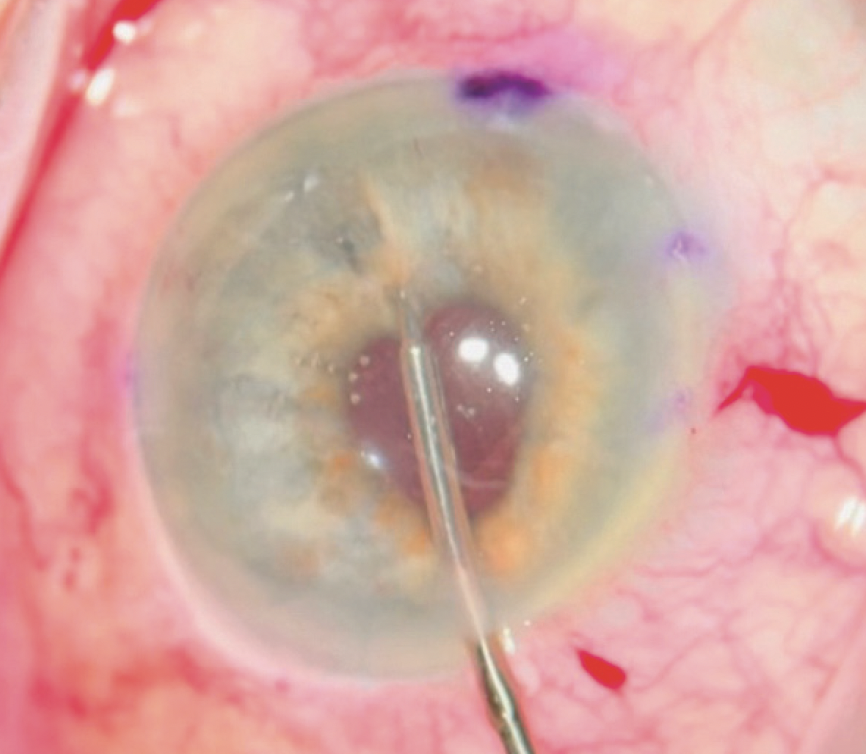
Figure 4. Iris trapped within the first double throw is released after the optic is pushed back.
No. 10: The suture is locked by tying the remaining single throw. Any trapped iris tissue is released (Figure 5).
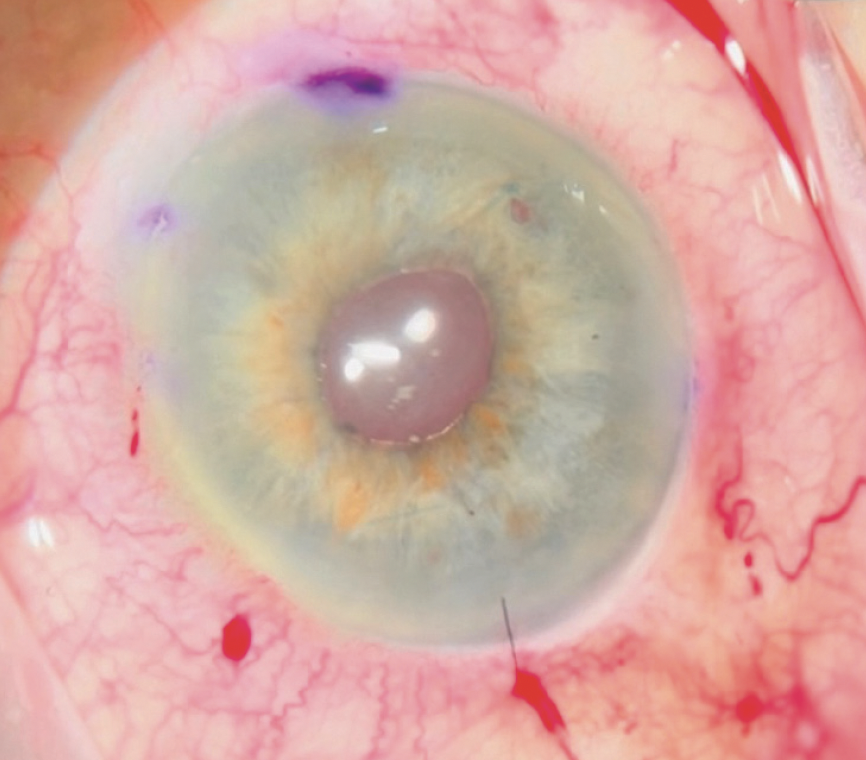
Figure 5. The final pupil is round if all steps are followed.
CONCLUSION
ISF has fallen out of favor, but it can be a highly successful technique in the right patient.
1. Yamane S, Sato S, Maruyama-Inoue M, Kadonosono K. Flanged intrascleral intraocular lens fixation with double-needle technique. Ophthalmology. 2017;124(8):1136-1142.
2. Alsetri H, Masket S, Fram N, et al. Surgical outcomes of IOL iris suture fixation in eyes with residual capsule support. J Cataract Refract Surg. Published online December 11, 2023. doi:10.1097/j.jcrs.0000000000001375
3. Ahmed IIK, Campos-Möller X, Shah M, Sheybani A. Illustrated Advanced Anterior Segment Surgery: A Step-by-Step Guide for Challenging Cases. Slack; 2021.
4. Siepser SB. The closed chamber slipping suture technique for iris repair. Ann Ophthalmol. 1994;26(3):71-72.
5. Ayers B. How to tie a McAhmed knot for iris cerclage. YouTube. Accessed March 1, 2024. https://www.youtube.com/watch?v=zBA_roZJz2s