
The division between anterior and posterior segment specialization often delineates the boundaries of clinical and surgical practice in ophthalmology. The dissolution of these boundaries, however, can lead to significant advances in patient care. When we embrace a collaborative approach that leverages the collective expertise of diverse ophthalmic specialties, our patients benefit. This article recounts my personal journey into intersegmental collaboration, which began with an unanticipated opportunity that propelled me onto a path of learning, growth, and shared knowledge.
THE CATALYST OF COLLABORATION AND GROWTH
A serendipitous encounter with a cornea surgeon, William Richheimer, MD, began my foray into scleral fixation of three-piece IOLs with the Yamane technique.1 Tasked with stepping in for a colleague, I found myself faced with a complex case whose management required a complete change in my surgical approach to treating eyes without capsular support. I had been trained by world-renowned retina specialists at Wills Eye Hospital on the scleral fixation of IOLs with a well-established PTFE (Gore-Tex, W.L. Gore & Associates) suture technique, familiar to most vitreoretinal surgeons. My experience with Dr. Richheimer was enlightening, not only in a technical sense but also for its revelation of the vast potential of collaboration in ophthalmology, outside of the academic ivory tower. Dr. Richheimer, despite feeling unwell on the day of the surgery, provided supervision and guidance that enriched my perspective on and skill set for managing malfunctioning or malpositioned IOLs.
The case ignited in me a passion for intersegmental procedures and set the stage for a significant expansion of my surgical practice. As my proficiency with the scleral fixation of lenses with the Yamane technique increased, the referring ophthalmic community took notice. Individuals with complex combined anterior segment and posterior segment disease, who previously had limited options and often required staged surgical procedures to address their issues, began to find solutions within our practice. The growth was exponential, and soon, what began as a few cases a month burgeoned into a substantial part of my surgical volume.
CONTINUED COLLABORATION TO IMPROVE PATIENT CARE
Advanced biometry. Recognizing the critical role of accurate biometry in patient outcomes and the challenges of performing biometry at outside ophthalmic groups, my retina-only practice agreed to invest in an IOLMaster (Carl Zeiss Meditec). This allowed measurements of ocular dimensions and lens calculations to be performed in house, streamlining surgical planning and enhancing the precision of our interventions. Around the same time, we welcomed an optometrist, Betty Zhang, OD, onto our team. Her expertise on refraction, extensive experience in counseling patients on visual goals for cataract surgery, and deep understanding of retinal pathology as it relates to visual potential became an integral part of our patient care strategy, ensuring that we not only addressed the surgical issues at hand but also optimized patients’ refractive outcomes.
Scleral fixation of a Light Adjustable Lens. One of the most remarkable outcomes of a collaborative approach was the successful scleral fixation of a Light Adjustable Lens (LAL; RxSight) in an eye with a dislocated toric multifocal IOL and vitreous prolapse in the anterior chamber. Historically, achieving the refractive precision desired by a patient with a history of premium IOL implantation was not possible, often leaving them with less-than-ideal UCVA. The availability of a lens that can be adjusted postoperatively with UV light presented an unprecedented opportunity. In collaboration with cornea surgeon Matthew Kruger, MD, I performed a combined vitrectomy and lens exchange with the LAL, and he managed the patient’s postoperative UV laser treatments to correct the -1.00 x +2.00 @ 158º outcome to plano, exceeding the patient’s expectations (Figure). This innovation in the off-label use of an LAL would not have come without collaboration with my anterior segment colleagues. Since this initial case, I have collaborated with several other anterior segment specialists; I perform combined vitrectomy and implantation of an LAL in the sulcus or with scleral fixation, so they can perform postoperative light adjustments to maximize patient outcomes.
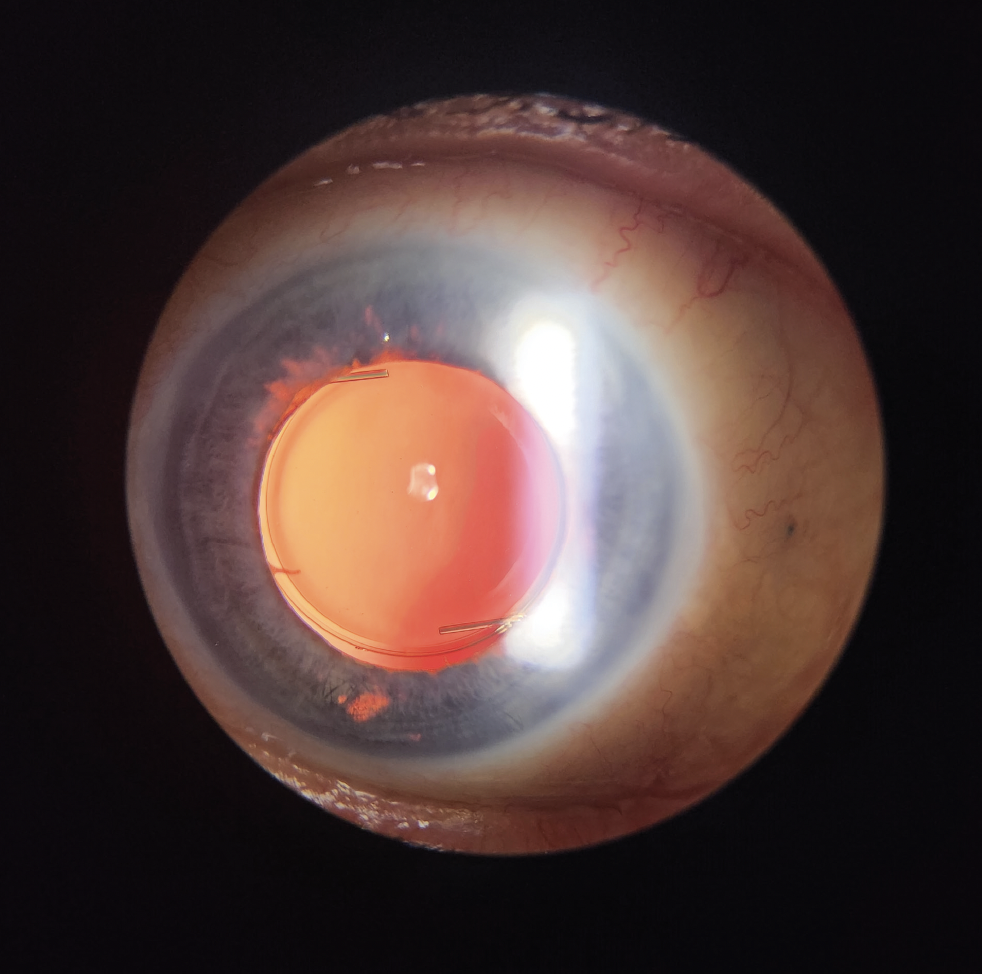
Figure. Postoperative anterior segment photo of a scleral-fixated LAL.
(Image courtesy of Matthew Kruger, MD)
ONGOING COLLABORATION IS KEY
Conversations with my anterior segment colleagues—whether discussing the best IOL formulas for patients with extreme refractive needs or consulting on cases where there is a history of refractive surgery—lead to an exchange of knowledge that is vital. I recently presented my own experience with scleral fixation of the LAL at the EnVision Summit and participated on a panel with expert cornea and refractive specialists (Eva Kim, MD; Sonia Yoo, MD; and Kevin M. Miller, MD) to discuss the importance of maximizing refractive outcomes and safety in patients with combined anterior and posterior segment disease. I learned quite a bit from my interactions with these experts, and they took away important pearls regarding the importance of appropriate comanagement with vitreoretinal surgeons to maximize patient safety.
CONCLUSION
The collective responsibility of ophthalmologists is to push the boundaries of what is possible through continuous learning, partnership, and innovation. The integration of anterior and posterior segment expertise, coupled with technological innovation and a team-oriented approach, has transformed my surgical practice, and I hope it has changed and will continue to change the lives of patients for the better.
1. Yamane S, Sato S, Maruyama-Inoue M, Kadonosono K. Flanged intrascleral intraocular lens fixation with double-needle technique. Ophthalmology. 2017;124(8):1136-1142.




